Abstract
Background/objectives
Visual impairment (VI) is associated with significant disruptions in sleep quality. This study aimed to investigate the association between VI and sleep quality across varying severities of VI and ocular conditions in adults.
Subjects/methods
A cross-sectional, observational, study was conducted among 277 adults with VI and 278 age- and sex-matched controls from two hospitals. Participants underwent comprehensive ocular examinations and completed the Arabic version of the Pittsburgh Sleep Quality Index (PSQI). Sociodemographic and clinical data were collected, and ocular conditions were recorded. Multivariate logistic regression models were used to evaluate the association between VI, its severity, ocular conditions, and poor sleep quality while adjusting for potential confounders.
Results
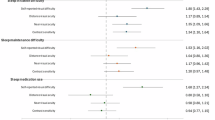
VI patients had worse sleep quality than controls (mean PSQI: 6.83 ± 3.6 vs. 5.30 ± 3.5; p < 0.001), with 57.8% experiencing poor sleep (PSQI > 5) compared to 36.7% of controls(p < 0.001). In multivariate analysis, patients with VI had significantly higher odds of poor sleep quality compared to controls (OR = 2.0 (95% CI: 1.4–2.8); p < 0.001). Moderate VI (OR = 2.1, 95% CI: 1.4–3.2, p = 0.001) and blindness (OR = 2.9, 95% CI: 1.4–5.9, p = 0.004) were significantly associated with poor sleep quality. Diabetic retinopathy (OR = 2.2, 95% CI: 1.4–3.4; p < 0.001) and combined ocular conditions (OR = 3.6, 95% CI: 1.4–9.3; p = 0.009) were significantly associated with poor sleep quality.
Conclusions
VI is significantly associated with poor sleep quality, particularly in moderate VI and blindness. Diabetic retinopathy and combined ocular conditions were associated with poor sleep quality. Comprehensive management strategies addressing sleep in VI patients are essential for improving their overall well-being.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Panigrahi A, Nageswar Rao G, Kumari Konar A. Vision-Related Quality of Life and Its Sociodemographic Correlates Among Individuals With Visual Impairments. J Vis Impair Blindness. 2021;115:319–28.
World Health Organization (2019) World report on vision. https://www.who.int/publications/i/item/9789241516570. Accessed 13 Feb 2025.
Tamura N, Sasai-Sakuma T, Morita Y, Okawa M, Inoue S, Inoue Y. Prevalence and associated factors of circadian rhythm sleep-wake disorders and insomnia among visually impaired Japanese individuals. BMC Public Health. 2021;21:31.
Chen X, Zhu Y, Luo M. The relationship between visual impairment and insomnia among people middle-aged and older in India. Sci Rep. 2024;14:30261.
Choi S, Kim G, Pionke JJ. The Sleep Health of Individuals with Visual Impairments: A Scoping Review. Ophthalmic Epidemiol 2025;32:259–77.
Uchiyama M, Lockley SW. Non-24-Hour Sleep-Wake Rhythm Disorder in Sighted and Blind Patients. Sleep Med Clin. 2015;10:495–516.
Hartley S, Dauvilliers Y, Quera-Salva M-A. Circadian Rhythm Disturbances in the Blind. Curr Neurol Neurosci Rep. 2018;18:65.
Aubin S, Gacon C, Jennum P, Ptito M, Kupers R. Altered sleep-wake patterns in blindness: a combined actigraphy and psychometric study. Sleep Med. 2016;24:100–8.
Xue R, Wan G. Association Between Vision-Related Functional Burden and Sleep Disorders in Adults Aged 20 and Over in the United States. Transl Vis Sci Technol. 2023;12:3.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Al Maqbali M, Hughes C, Gracey J, Rankin J, Dunwoody L, Hacker E. Validation of the Pittsburgh Sleep Quality Index (PSQI) with Arabic cancer patients. Sleep Biol Rhythms. 2020;18:217–23.
Ghemrawi R, Kerek R, Kayed K, Aldulaymi R, Ramadan A, Khair M. Association between visual impairment and sleep duration in college students: A study conducted in UAE and Lebanon. J Am Coll Health. 2023;71:228–34.
von Gall C. The Effects of Light and the Circadian System on Rhythmic Brain Function. Int J Mol Sci. 2022;23:2778.
Skene DJ, Arendt J. Circadian rhythm sleep disorders in the blind and their treatment with melatonin. Sleep Med. 2007;8:651–5.
Nastasi JA. The strategies used by adults with visual impairment. Br J Occup Ther. 2024;87:213–20.
Arns M, Kooij JJS, Coogan AN. Review: Identification and Management of Circadian Rhythm Sleep Disorders as a Transdiagnostic Feature in Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 2021;60:1085–95.
Ramos AR, Wallace DM, Williams NJ, Spence DW, Pandi-Perumal SR, Zizi F, et al. Association between visual impairment and sleep duration: analysis of the 2009 National Health Interview Survey (NHIS). BMC Ophthalmol. 2014;14:1–5.
Barbosa DG, Andrade RD, Santos MdeO, Silva RCD, Beltrame TS, Gomes Felden ÉP. Assessment of sleep in subjects with visual impairment: Comparison using subjective and objective methods. Chronobiol Int. 2017;34:895–902.
Um YH, Kim T-W, Jeong J-H, Hong S-C, Seo H-J, Han K-D Association Between Diabetic Retinopathy and Insomnia Risk: A Nationwide Population-Based Study. Front Endocrinol. https://doi.org/10.3389/fendo.2022.939251 (2022).
Tan NYQ, Chew M, Tham Y-C, Nguyen QD, Yasuda M, Cheng C-Y, et al. Associations between sleep duration, sleep quality and diabetic retinopathy. PLoS ONE. 2018;13:e0196399.
Altaf QA, Dodson P, Ali A, Raymond NT, Wharton H, Fellows H, et al. Obstructive Sleep Apnea and Retinopathy in Patients with Type 2 Diabetes. A Longitudinal Study. Am J Respir Crit Care Med. 2017;196:892–900.
Chang AC, Fox TP, Wang S, Wu AY. Relationship Between Obstructive Sleep Apnea And The Presence And Severity Of Diabetic Retinopathy. RETINA. 2018;38:2197.
Ayaki M, Shiba D, Negishi K, Tsubota K. Depressed visual field and mood are associated with sleep disorder in glaucoma patients. Sci Rep. 2016;6:25699.
Agorastos A, Skevas C, Matthaei M, Otte C, Klemm M, Richard G, et al. Depression, Anxiety, and Disturbed Sleep in Glaucoma. JNP. 2013;25:205–13.
Stoner AM, Patnaik JL, Ertel MK, Capitena-Young CE, SooHoo JR, Pantcheva MB, et al. Subjective and Objective Measurement of Sleep Quality and Activity in Glaucoma. J Glaucoma. 2023;32:265–71.
Jimura H, Yoshikawa T, Obayashi K, Miyata K, Saeki K, Ogata N. Post-Illumination Pupil Response and Sleep Quality in Patients With Glaucoma: The LIGHT Study. Invest Ophthalmol Vis Sci. 2023;64:34.
Bec L, Herber R, Bailly S, Van Ngo TH, Tamisier R, Pépin J-L, et al. Sleep quality in glaucoma patients. Sci Rep. 2024;14:25593.
Sia JT, Lee EPX, Cheung CMG, Fenwick EK, Laude A, Ho KC, et al. Associations between age-related macular degeneration and sleep dysfunction: A systematic review. Clin Exp Ophthalmol. 2022;50:1025–37.
Etindele Sosso FA, Kreidlmayer M, Pearson D, Bendaoud I. Towards A Socioeconomic Model of Sleep Health among the Canadian Population: A Systematic Review of the Relationship between Age, Income, Employment, Education, Social Class, Socioeconomic Status and Sleep Disparities. Eur J Investig Health, Psychol Educ. 2022;12:1143–67.
Gulati I, Kilian C, Buckley C, Mulia N, Probst C Socioeconomic disparities in healthcare access and implications for all-cause mortality among US adults: a 2000-2019 record linkage study. Am J Epidemiol. 2025;194:432–40.
Kim H, Park J, Kim JB. A Case of Circadian Rhythm Sleep-Wake Disorder in Partial Blindness. J Sleep Med. 2018;15:31–34.
Kessel L, Siganos G, Jørgensen T, Larsen M. Sleep Disturbances Are Related to Decreased Transmission of Blue Light to the Retina Caused by Lens Yellowing. Sleep. 2011;34:1215–9.
Gubin DG, Malishevskaya N, Astakhov YS, Astakhov SY, Cornelissen G, Kuznetsov VA, et al. Progressive retinal ganglion cell loss in primary open-angle glaucoma is associated with temperature circadian rhythm phase delay and compromised sleep. Chronobiol Int. 2019;36:564–77.
Zizi F, Jean-Louis G, Magai C, Greenidge KC, Wolintz AH, Heath-Phillip O. Sleep Complaints and Visual Impairment Among Older Americans: A Community-Based Study. J Gerontol Ser A. 2002;57:M691–4.
Adhikari S, van Nispen RMA, Poudel M, van Rens F, Elsman EBM, van der Werf YD, et al. Sleep Patterns in Children With Blindness: A Comparison With Normally Sighted Peers. Invest Ophthalmol Vis Sci. 2023;64:46.
Hayton J, Marshall J, Dimitriou D. Lights Out: Examining Sleep in Children with Vision Impairment. Brain Sci. 2021;11:421.
Khan SA, Heussler H, McGuire T, Dakin C, Pache D, Norris R, et al. Therapeutic options in the management of sleep disorders in visually impaired children: a systematic review. Clin Ther. 2011;33:168–81.
Leger D, Prevot E, Philip P, Yence C, Labaye N, Paillard M, et al. Sleep disorders in children with blindness. Ann Neurol. 1999;46:648–51.
Dietrich SK, Francis-Jimenez CM, Knibbs MD, Umali IL, Truglio-Londrigan M. Effectiveness of sleep education programs to improve sleep hygiene and/or sleep quality in college students: a systematic review. JBI Evid Synth. 2016;14:108.
Asplund R, Lindblad BE. Sleep and sleepiness 1 and 9 months after cataract surgery. Arch Gerontol Geriatr. 2004;38:69–75.
Funding
This work was supported by the deanship of research, Jordan University of Science and Technology, Grant No: [20210196]. The sponsor was not involved in any stage of this work.
Author information
Authors and Affiliations
Contributions
HJ led the conceptualisation, methodology, formal analysis, investigation, writing - original draft, supervision, and funding acquisition. YK was involved in conceptualisation, methodology, formal analysis, writing - review & editing. KA was involved in conceptualisation, resources, writing - review & editing. RA was involved in conceptualisation, writing - review & editing. MA was involved in conceptualisation, methodology, investigation, writing - review & editing. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jammal, H.M., Khader, Y., Almhdawi, K. et al. Association between visual impairment and sleep quality: A cross-sectional, comparative study of severity, eye conditions, and risk factors. Eye 40, 230–237 (2026). https://doi.org/10.1038/s41433-025-04150-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04150-0