Abstract
Objectives
To quantify macular cone cell mosaic metrics in patients with varying degrees of myopia and explore its link to myopia severity using an adaptive optics (AO) fundus camera.
Methods
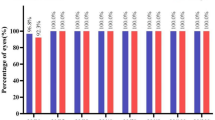
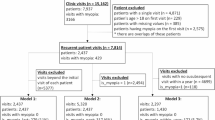
A total of 76 age- and gender-matched patients with varying degrees of myopia (pre-myopia, low, moderate, and high) were recruited. Macular cone cell mosaic metrics (density, spacing, regularity, dispersion) were quantified via adaptive optics (AO) imaging, including correlations between AO-derived parameters and clinical indicators (spherical equivalent refraction, axial length) and predictive efficacy of AO metrics for myopia severity evaluated through receiver operating characteristic (ROC) curve analysis.
Results
As spherical equivalent refraction (SER) decreased, cone density (r = 0.65) and regularity (r = 0.38) significantly declined, while spacing (r = –0.65) and dispersion (r = –0.40) increased (all P < 0.001). Axial length (AL) was negatively correlated with density (r = –0.62) and regularity (r = –0.39), and positively correlated with spacing (r = 0.61) and dispersion (r = 0.38) (all P < 0.001). Predictive efficacy analysis based on AO-derived parameters revealed the highest AUROC value in the HM group (0.96), followed by Pre-M (0.86), LM (0.82), and MM (0.65) groups, indicating that AO metrics demonstrated superior early identification capability for HM severity.
Conclusions
The AO fundus camera enables noninvasive evaluation of macular cone cell mosaic metrics, revealing strong correlations between density, regularity, spacing, dispersion, and myopia severity. These metrics demonstrate potential as biomarkers for evaluating myopic changes, with AO showing enhanced diagnostic efficacy in high myopia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request. The data are not publicly available due to privacy or ethical restrictions.
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Modjtahedi BS, Abbott RL, Fong DS, Lum F, Tan D, Task Force on Myopia. Reducing the global burden of myopia by delaying the onset of myopia and reducing myopic progression in children: the academy’s task force on myopia. Ophthalmology. 2021;128:816–26.
Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739–48.
He HL, Liu YX, Chen XY, Ling SG, Qi Y, Xiong Y, et al. Fundus tessellated density of pathologic myopia. Asia Pac J Ophthalmol (Philos. 2023;12:604–13.
Jones D, Luensmann D. The prevalence and impact of high myopia. Eye Contact Lens. 2012;38:188–96.
Wang Y, Ye J, Shen M, Yao A, Xue A, Fan Y, et al. Photoreceptor degeneration is correlated with the deterioration of macular retinal sensitivity in high myopia. Invest Ophthalmol Vis Sci. 2019;60:2800–10.
Ho WC, Kee CS, Chan HH. Myopia progression in children is linked with reduced foveal mfERG response. Invest Ophthalmol Vis Sci. 2012;53:5320–5.
Chen JC, Brown B, Schmid KL. Delayed mfERG responses in myopia. Vis Res. 2006;46:1221–9.
Zhang B, Li N, Kang J, He Y, Chen XM. Adaptive optics scanning laser ophthalmoscopy in fundus imaging, a review and update. Int J Ophthalmol. 2017;10:1751–8.
Cristescu IE, Baltă F, Zăgrean L. Cone photoreceptor density in type I diabetic patients measured with an adaptive optics retinal camera. Rom J Ophthalmol. 2019;63:153–60.
Soliman MK, Sadiq MA, Agarwal A, Sarwar S, Hassan M, Hanout M, et al. High-resolution imaging of parafoveal cones in different stages of diabetic retinopathy using adaptive optics fundus camera. PLoS One. 2016;11:e0152788.
Antonetti DA, Silva PS, Stitt AW. Current understanding of the molecular and cellular pathology of diabetic retinopathy. Nat Rev Endocrinol. 2021;17:195–206.
Legras R, Gaudric A, Woog K. Distribution of cone density, spacing and arrangement in adult healthy retinas with adaptive optics flood illumination. PLoS One. 2018;13:e0191141.
Yang Y, Wang J, Jiang H, Yang X, Feng L, Hu L, et al. Retinal microvasculature alteration in high myopia. Invest Ophthalmol Vis Sci. 2016;57:6020–30.
Zhang S, Zhang G, Zhou X, Xu R, Wang S, Guan Z, et al. Changes in choroidal thickness and choroidal blood perfusion in guinea pig myopia. Invest Ophthalmol Vis Sci. 2019;60:3074–83.
He HL, Liu YX, Liu H, Zhang X, Song H, Xu TZ, et al. Deep learning-enabled vasculometry depicts phased lesion patterns in high myopia progression. Asia Pac J Ophthalmol (Philos). 2024;13:100086.
Wu Q, Chen Q, Lin B, Huang S, Wang Y, Zhang L, et al. Relationships among retinal/choroidal thickness, retinal microvascular network and visual field in high myopia. Acta Ophthalmol. 2020;98:e709–e714.
Lejoyeux R, Benillouche J, Ong J, Errera MH, Rossi EA, Singh SR, et al. Choriocapillaris: fundamentals and advancements. Prog Retin Eye Res. 2022;87:100997.
Nishida Y, Fujiwara T, Imamura Y, Lima LH, Kurosaka D, Spaide RF. Choroidal thickness and visual acuity in highly myopic eyes. Retina. 2012;32:1229–36.
Flores-Moreno I, Ruiz-Medrano J, Duker JS, Ruiz-Moreno JM. The relationship between retinal and choroidal thickness and visual acuity in highly myopic eyes. Br J Ophthalmol. 2013;97:1010–3.
Wu H, Zhang G, Shen M, Xu R, Wang P, Guan Z, et al. Assessment of choroidal vascularity and choriocapillaris blood perfusion in anisomyopic adults by SS-OCT/OCTA. Invest Ophthalmol Vis Sci. 2021;62:8.
Yang J, Ouyang X, Fu H, Hou X, Liu Y, Xie Y, et al. Advances in biomedical study of the myopia-related signaling pathways and mechanisms. Biomed Pharmacother. 2022;145:112472.
Chinese Optometric Association, Chinese Ophthalmological Society, Ophthalmology and Optometry Committee, Ophthalmologists Association, Chinese Doctor Association, Ophthalmology and Optometry Group, Ophthalmologic Committee, Chinese Non-Government Medical Institutions Association, Eye Refractive Error Prevention and Control Group of the Cross-Straits Medical Exchange Association, Commission of Ophthalmology, Ophthalmology Branch of Chinese Geriatrics Society. Expert Consensus on Prevention and Control of High Myopia (2023). Chin J Optom Ophthalmol Vis Sci. 2023;25:401–7. https://doi.org/10.3760/cma.j.cn115909-20230509-00147.
Babcock HW. The possibility of compensating astronomical seeing. Publ Astronomical Soc Pac. 1953;65:229.
Dabir S, Mangalesh S, Schouten JS, Berendschot TT, Kurian MK, Kumar AK, et al. Axial length and cone density as assessed with adaptive optics in myopia. Indian J Ophthalmol. 2015;63:423–6.
Curcio CA, Sloan KR, Kalina RE, Hendrickson AE. Human photoreceptor topography. J Comp Neurol. 1990;292:497–523.
Baird, Saw PN, Lanca SM, Guggenheim C, Smith JA, Iii EL, et al. Myopia. Nat Rev Dis Prim. 2020;6:99.
Cui M, Zhu Z, Gao Y, Zong X, Li S, Liu J, et al. Research on the predictive performance of using ROC curve to evaluate axial length for myopia in children and adolescents. BMC Ophthalmol. 2025;25:195.
Liu R, Xuan M, Wang DC, Xiao O, Guo XX, Zhang J, et al. Using choroidal thickness to detect myopic macular degeneration. Int J Ophthalmol. 2024;17:317–23.
Pang CE, Sarraf D, Freund KB. Extreme choroidal thinning in high myopia. Retina. 2015;35:407–15.
Gupta P, Cheung CY, Saw S, Koh V, Tan M, Yang A, et al. Choroidal thickness does not predict visual acuity in young high myopes. Acta Ophthalmol. 2016;94:e764–e765.
Zhou Y, Song M, Zhou M, Liu Y, Wang F, Sun X. Choroidal and retinal thickness of highly myopic eyes with early stage of myopic chorioretinopathy: tessellation. J Ophthalmol. 2018;2018:2181602.
Zhang Y, Zhong Y, Mao W, Zhang Z, Zhou Y, Li H, et al. Clinical features evaluation of myopic fundus tessellation from OCTA and MfERG. Photodiagnosis Photodyn Ther. 2025;52:104493.
Sui J, Li H, Bai Y, He Q, Sun Z, Wei R. Morphological characteristics of the foveal avascular zone in pathological myopia and its relationship with macular structure and microcirculation. Graefes Arch Clin Exp Ophthalmol. 2024;262:2121–33.
McBrien NA. Regulation of scleral metabolism in myopia and the role of transforming growth factor-beta. Exp Eye Res. 2013;114:128–40.
Jobling AI, Nguyen M, Gentle A, McBrien NA. Isoform-specific changes in scleral transforming growth factor-beta expression and the regulation of collagen synthesis during myopia progression. J Biol Chem. 2004;279:18121–6.
Jiang B, Wu ZY, Zhu ZC, Ke GJ, Wen YC, Sun SQ. Expression and role of specificity protein 1 in the sclera remodeling of experimental myopia in guinea pigs. Int J Ophthalmol. 2017;10:550–4.
Qian YS, Chu RY, Hu M, Hoffman MR. Sonic hedgehog expression and its role in form-deprivation myopia in mice. Curr Eye Res. 2009;34:623–35.
Chen M, Qian Y, Dai J, Chu R. The sonic hedgehog signaling pathway induces myopic development by activating matrix metalloproteinase (MMP)-2 in Guinea pigs. PLoS One. 2014;9:e96952.
Liu YX, Sun Y. MMP-2 participates in the sclera of guinea pig with form-deprivation myopia via IGF-1/STAT3 pathway. Eur Rev Med Pharm Sci. 2018;22:2541–8.
She M, Li B, Li T, Hu Q, Zhou X. Modulation of the ERK1/2-MMP-2 pathway in the sclera of guinea pigs following induction of myopia by flickering light. Exp Ther Med. 2021;21:371.
Zhao F, Zhou Q, Reinach PS, Yang J, Ma L, Wang X, et al. Cause and effect relationship between changes in scleral matrix metallopeptidase-2 expression and myopia development in mice. Am J Pathol. 2018;188:1754–67.
Wu H, Chen W, Zhao F, Zhou Q, Reinach PS, Deng L, et al. Scleral hypoxia is a target for myopia control. Proc Natl Acad Sci USA. 2018;115:E7091–E7100.
Zhao F, Zhang D, Zhou Q, Zhao F, He M, Yang Z, et al. Scleral HIF-1alpha is a prominent regulatory candidate for genetic and environmental interactions in human myopia pathogenesis. EBioMedicine. 2020;57:102878.
Xie Y, Ouyang X, Wang G. Mechanical strain affects collagen metabolism-related gene expression in scleral fibroblasts. Biomed Pharmacother. 2020;126:110095.
Elsner AE, Chui TY, Feng L, Song HX, Papay JA, Burns SA. Distribution differences of macular cones measured byAOSLO: variation in slope from fovea to periphery more pronounced than differences in total cones. Vis Res. 2017;132:62–8.
Zhang T, Godara P, Blanco ER, Griffin RL, Wang X, Curcio CA, et al. Variability in human cone topography assessed by adaptive optics scanning laser ophthalmoscopy. Am J Ophthalmol. 2015;160:290–300.
Acknowledgements
We thank the patients for their participation in the study. They also gratefully acknowledge Tang Li from Zhitong Vision Science (Chongqing) Biotechnology Co., Ltd. for providing technical support for the AO instrumentation and valuable suggestions.
Funding
This study was supported by grants from the Science and Technology Research Programme of Chongqing Municipal Education Commission (Grant No. KJZD-K202400402), the National Natural Science Foundation of China (No. 81970832, 81371043 and 81800814).
Author information
Authors and Affiliations
Contributions
K-YL was responsible for data collection and examination, data analysis, manuscript drafting and manuscript revision. J-XL was responsible for data collection and examination. Z-YL was responsible for data collection and examination. YY was responsible for data analysis. R-YX was responsible for data collection. CZ was responsible for data collection. QL was responsible for data analysis. S-LL was responsible for manuscript revision. W-JW was responsible for manuscript revision. W-LD (guarantor) was responsible for study design, data collection, examination, data analysis, manuscript revision and supervision of the study process. Y-LZ (guarantor) was data analysis, manuscript drafting, manuscript revision and supervision of the study process. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, KY., Liu, JX., Li, ZY. et al. Macular cone cell mosaic metrics in myopia: severity evaluation and diagnostic efficiency using adaptive optics fundus camera. Eye (2026). https://doi.org/10.1038/s41433-025-04171-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41433-025-04171-9