Abstract
Purpose
To compare outcomes between eyes that underwent penetrating keratoplasty (PKP) following cyanoacrylate tissue adhesive (CTA) application for corneal perforation or thinning and those managed with conservative treatment alone.
Methods
We conducted a single-centre, comparative cohort study of 189 eyes with corneal perforation or thinning treated with CTA at a tertiary care centre. Eyes were categorised into two groups: those managed with CTA alone and those requiring subsequent PKP. The primary outcome was best-corrected visual acuity (BCVA) at final follow-up. Characteristics and outcomes were compared using Fisher’s exact and Mann-Whitney U tests.
Results
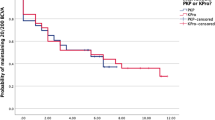
Of 189 eyes, 125 (66%) were managed conservatively with CTA alone and 64 (34%) required PKP. In the CTA group, the most common underlying aetiologies were microbial (31%, n = 37), neurotrophic (28%, n = 33), and trauma-related (22%, n = 26). Among eyes requiring subsequent PKP, microbial (46%, n = 25) aetiologies predominated, with viral keratitis more frequently observed (17%; P = 0.018) and trauma less frequently observed (6%; P = 0.008) compared to eyes managed conservatively. Final BCVA was comparable between groups (median logMAR 2.0 [CTA group] and 1.7 [PKP group]; P = 0.382), as was the median change in BCVA from presentation to final follow-up (P = 0.441). Subgroup analyses of corneal thinning and perforation showed consistent findings.
Conclusions
Visual outcomes were comparable between eyes managed conservatively with CTA and those that underwent PKP, despite more severe baseline disease in the PKP group. These findings underscore the importance of individualised patient selection and may help avoid unnecessary surgical intervention when clinical stability can be achieved conservatively.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Portnoy SL, Insler MS, Kaufman HE. Surgical management of corneal ulceration and perforation. Surv Ophthalmol. 1989;34:47–58.
Deshmukh R, Stevenson LJ, Vajpayee R. Management of corneal perforations: An update. Indian J Ophthalmol. 2020;68:7–14.
Sharma A, Sharma N, Basu S, Sharma R, Aggarwal S, Gupta PC, et al. Tissue Adhesives for the Management of Corneal Perforations and Challenging Corneal Conditions. Clin Ophthalmol. 2023;17:209–23.
Webster RG Jr., Slansky HH, Refojo MF, Boruchoff SA, Dohlman CH. The use of adhesive for the closure of corneal perforations. Report of two cases. Arch Ophthalmol. 1968;80:705–9.
Jhanji V, Young AL, Mehta JS, Sharma N, Agarwal T, Vajpayee RB. Management of Corneal Perforation. Surv Ophthalmol. 2011;56:522–38.
Lekskul M, Fracht HU, Cohen EJ, Rapuano CJ, Laibson PR. Nontraumatic corneal perforation. Cornea. 2000;19:313–9.
Moorthy S, Jhanji V, Constantinou M, Beltz J, Graue-Hernandez EO, Vajpayee RB. Clinical experience with N-butyl cyanoacrylate tissue adhesive in corneal perforations secondary to herpetic keratitis. Cornea. 2010;29:971–5.
Agarwal M, Almuhannadi H, Huang RS, Chan CC. Large-Diameter Optical Penetrating Keratoplasty: Indications, Mid-term Outcomes, and Literature Review. Am J Ophthalmol. 2025;280:1–8.
Weiss JL, Williams P, Lindstrom RL, Doughman DJ. The use of tissue adhesive in corneal perforations. Ophthalmology. 1983;90:610–5.
Loya-Garcia D, Serna-Ojeda JC, Pedro-Aguilar L, Jimenez-Corona A, Olivo-Payne A, Graue-Hernandez EO. Non-traumatic corneal perforations: aetiology, treatment and outcomes. Br J Ophthalmol. 2017;101:634–9.
Leahey AB, Gottsch JD, Stark WJ. Clinical experience with N-butyl cyanoacrylate (Nexacryl) tissue adhesive. Ophthalmology. 1993;100:173–80.
Huang RS, Agarwal M, Mimouni M, Rootman DS, Chan CC. Comparative outcomes of single versus multiple cyanoacrylate tissue adhesive applications in the management of corneal thinning and perforation. Cornea. 2025. Epub ahead of print.
Garg P, Gopinathan U, Nutheti R, Rao GN. Clinical experience with N-butyl cyanoacrylate tissue adhesive in fungal keratitis. Cornea. 2003;22:405–8.
Sharma A, Kaur R, Kumar S, Gupta P, Pandav S, Patnaik B, et al. Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology. 2003;110:291–8.
Setlik DE, Seldomridge DL, Adelman RA, Semchyshyn TM, Afshari NA. The effectiveness of isobutyl cyanoacrylate tissue adhesive for the treatment of corneal perforations. Am J Ophthalmol. 2005;140:920–1.
Cosar CB, Cohen EJ, Rapuano CJ, Maus M, Penne RP, Flanagan JC, et al. Tarsorrhaphy: clinical experience from a cornea practice. Cornea. 2001;20:787–91.
Macsai MS. The management of corneal trauma: advances in the past twenty-five years. Cornea. 2000;19:617–24.
Mallari PLT, McCarty DJ, Daniell M, Taylor H. Increased incidence of corneal perforation after topical fluoroquinolone treatment for microbial keratitis. Am J Ophthalmol. 2001;131:131–3.
Cavanaugh TB, Gottsch JD. Infectious keratitis and cyanoacrylate adhesive. Am J Ophthalmol. 1991;111:466–72.
Anchouche S, Harissi-Dagher M, Segal L, Racine L, Darvish-Zargar M, Robert MC. Cyanoacrylate Tissue Adhesive for the Treatment of Corneal Thinning and Perforations: A Multicenter Study. Cornea. 2020;39:1371–6.
Agarwal M, Huang RS, Mimouni M, Rootman DS, Chan CC. Clinical Outcomes and Predictive Factors for Penetrating Keratoplasty Following Glue Application for Corneal Perforation and Thinning. Am J Ophthalmol. 2025;280:203–8.
Messmer EM, Foster CS. Vasculitic peripheral ulcerative keratitis. Surv Ophthalmol. 1999;43:379–96.
Yin J, Singh RB, Al Karmi R, Yung A, Yu M, Dana R. Outcomes of cyanoacrylate tissue adhesive application in corneal thinning and perforation. Cornea. 2019;38:668–73.
Author information
Authors and Affiliations
Contributions
Ryan S. Huang: Conceptualisation, Methodology, Data curation, Formal analysis, Investigation, Visualisation, Writing – Original draft preparation, Writing – Reviewing and Editing. Manokamna Agarwal: Conceptualisation, Methodology, Investigation, Data curation, Writing – Reviewing and Editing. Michael Mimouni: Conceptualisation, Methodology, Validation, Investigation, Writing – Original draft preparation, Writing – Reviewing and Editing. Clara C. Chan: Conceptualisation, Methodology, Supervision, Project administration, Validation, Resources, Writing – Reviewing and Editing. All authors have equally fulfilled the authorship criteria and contributions outlined by the International Committee of Medical Journal Editors (ICMJE) and approved the current version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Clara C. Chan: Consultant – Aequus, Abbvie, Admare Bioinnovations, Allergan Inc., Aurion, Bausch & Lomb, Johnson & Johnson Vision, Kala Ophthalmics, Labtician Ophthalmics Inc., Novartis, Santen Inc., Sun Ophthalmics, Thea, Valeo Pharma. Financial support (to institution) – Aurion, Corneat, Claris Bio. Lecture fees – Abbvie, Allergan Inc., Johnson & Johnson Vision, Labtician Ophthalmics Inc., Thea. Michael Mimouni: Consultant – Lapidot Medical, Lumenis, EyeYon Medical, Orasis Pharmaceuticals, Precise Bio, Amntiotek, Labtician. Ryan S. Huang and Manokamna Agarwal have no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, R.S., Agarwal, M., Mimouni, M. et al. Comparative effectiveness of penetrating keratoplasty and conservative cyanoacrylate tissue adhesive application for corneal perforation and thinning. Eye (2026). https://doi.org/10.1038/s41433-025-04201-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41433-025-04201-6