Abstract
Objective
To assess the outcomes of surgical management of aqueous misdirection (AM) by endoscopic pars plana vitrectomy with hyaloido–zonulo–iridectomy.
Materials and methods
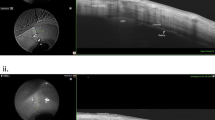
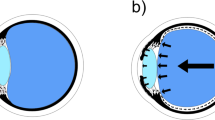
In this prospective, longitudinal, noncomparative interventional study, 53 eyes from 46 patients with AM refractory to medical and laser therapy after intraocular surgery were enrolled. All eyes underwent lens removal (if phakic), endoscopic pars plana vitrectomy, and hyaloido–zonulo–iridectomy. Primary outcomes included intraocular pressure (IOP), best-corrected visual acuity (BCVA), anterior chamber depth (ACD), postoperative complications, relapse rate, and composite surgical success. Surgical success was defined as the combination of IOP control and anterior chamber reformation, using two alternative IOP thresholds ( ≥ 6 and ≤18 mmHg, or ≥6 and ≤21 mmHg). Continuous variables were analysed using linear mixed models and expressed as estimated means (est)± standard error.
Results
Mean age was 59.7 ± 12.2 years. The est. IOP decreased from 34.36 ± 0.82 mmHg to 17.47 ± 0.82 mmHg at 12 months (p < 0.001). The est. BCVA improved from 1.50 ± 0.07 to 0.70 ± 0.07 logMAR at 12 months (p < 0.001). The est. ACD increased from 0.70 ± 0.06 to 3.34 ± 0.06 mm (p < 0.001), with complete anterior chamber reformation in all eyes. Postoperative complications occurred in 22 eyes (41.8%), mostly transient and resolved with medical or YAG laser treatment; only one required glaucoma surgery. At 12 months, overall success was 98.1% using the ≤21 mmHg criterion and 75.5% using the ≤18 mmHg criterion. No relapses were observed.
Conclusions
Surgical management using lens removal, endoscopic anterior vitrectomy, and hyaloido–zonulo–iridectomy is a significantly effective and safe treatment for AM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study, which were used for all statistical analyses and for the creation of all figures, as well as the tables, are available from the corresponding author upon reasonable request.
References
Graefe A. Beiträge zur Pathologie und Therapie des Glaucoms. Albrecht von Graefes Arch für Ophthalmologie. 1869;15:108–252.
Simmons RJ. Malignant glaucoma. Br J Ophthalmol. 1972;56:263–72.
Debrouwere V, Stalmans P, Van Calster J, Spileers W, Zeyen T, Stalmans I. Outcomes of different management options for malignant glaucoma: a retrospective study. Graefe’s Arch Clin Exp Ophthalmol. 2012;250:131–41.
Chang C-J, Huang Y-F. Endoscope-assisted vitrectomy in the management of retinal detachment with corneal opacity. Taiwan J Ophthalmol. 2017;7:164.
Do T, Do NH, Aung T, Nguyen DTNH, Cowan Jr CL. Bacterial endogenous endophthalmitis in Vietnam: a randomized controlled trial comparing vitrectomy with silicone oil versus vitrectomy alone. Clin Ophthalmol. 2014;8:1633–40.
Yu Y-Z, Chen W-X, Peng L-H, Zou Y-P, Pang L, Zou X-L. Endoscopy-assisted vitrectomy for severe ocular penetrating trauma with corneal opacity. Int J Ophthalmol. 2024;17:2256–64.
Epstein DL. The malignant glaucoma syndromes. Chandler and Grant’s Glaucoma, 4th ed Baltimore: Williams and Wilkins. 1997:285-303.
Rękas M, Krix-Jachym K, Żarnowski T. Evaluation of the effectiveness of surgical treatment of malignant glaucoma in pseudophakic eyes through partial PPV with establishment of communication between the anterior chamber and the vitreous cavity. J Ophthalmol. 2015;2015:1–6.
Yoon JH, Kim JH, Kim CG, Kim JW. Incidence of early complications requiring treatment plan changes after vitreoretinal surgery: a single-center study in South Korea. BMC Ophthalmol. 2023;23:282.
Shaarawy T, Sherwood M, Grehn F. WGA guidelines on design and reporting of glaucoma surgical trials: Kugler publications; 2009.
Shaffer RN. The role of vitreous detachment in aphakic and malignant glaucoma. Trans Am Acad Ophthalmol Otolaryngol. 1954;58:217–31.
Quigley HA, Friedman DS, Congdon NG. Possible mechanisms of primary angle-closure and malignant glaucoma. J Glaucoma. 2003;12:167–80.
Chaudhry NA, Flynn HW, Murray TG, Nicholson D, Palmberg PF. Pars plana vitrectomy during cataract surgery for prevention of aqueous misdirection in high-risk fellow eyes. Am J Ophthalmol. 2000;129:387–8.
Epstein DL, Hashimoto JM, Anderson PJ, Grant WM. Experimental perfusions through the anterior and vitreous chambers with possible relationships to malignant glaucoma. Am J Ophthalmol. 1979;88:1078–86.
Byrnes GA, Leen MM, Wong TP, Benson WE. Vitrectomy for ciliary block (malignant) glaucoma. Ophthalmology. 1995;102:1308–11.
Tsai JC, Barton KA, Miller MH, Khaw PT, Hitchings RA. Surgical results in malignant glaucoma refractory to medical or laser therapy. Eye. 1997;11:677–81.
Harbour JW. Pars plana vitrectomy in the management of Phakic and Pseudophakic malignant glaucoma. Arch Ophthalmol. 1996;114:1073.
Zhou C, Qian S, Yao J, Tang Y, Qian J, Lu Y, et al. Clinical analysis of 50 chinese patients with aqueous misdirection syndrome: a retrospective hospital-based study. J Int Med Res. 2012;40:1568–79.
Varma DK, Belovay GW, Tam DY, Ahmed IIK. Malignant glaucoma after cataract surgery. J Cataract Refractive Surg. 2014;40:1843–9.
Author information
Authors and Affiliations
Contributions
Conception or design of the work: HTTP, TD, TA. Acquisition, analysis, or interpretation of data: HTTP, TD, TA. Drafted the work or substantively revised it: HTTP, TD, AS, TA.
Corresponding author
Ethics declarations
Competing interests
TA serves on the Editorial Board of Eye. The authors declare no other conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Do, T., Pham, H.T.T., Servillo, A. et al. Surgical management of aqueous misdirection by endoscopic vitrectomy with Hyaloido-Zonulo-Iridectomy. Eye (2026). https://doi.org/10.1038/s41433-026-04265-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41433-026-04265-y