Abstract
Objectives
Acute syphilitic posterior placoid chorioretinopathy (ASPPC) is traditionally viewed as a uniform presentation of syphilitic posterior uveitis, though recent evidence suggests broader phenotypic variability. This study aimed to characterise ASPPC heterogeneity using multimodal imaging (MMI).
Methods
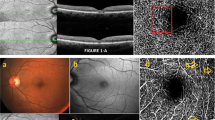
Single-centre retrospective cohort study on patients presenting with syphilitic posterior uveitis or panuveitis. MMI included fundus autofluorescence (FAF), fluorescein angiography (FA), indocyanine green angiography (ICGA), and optical coherence tomography (OCT). Cases were classified as typical ASPPC when a unifocal, well-demarcated placoid lesion was present at the posterior pole, and as atypical when multifocal lesions were funduscopically occult but evident on FAF. Macular sensitivity recovery post-antibiotic treatment was evaluated in a subset of cases using microperimetry.
Results
Among 33 eyes from 21 patients (median age: 51 years, 91% male), 55% had typical ASPPC and 45% an atypical presentation. HIV co-infection was found only in patients with a typical placoid lesion (42%). Both phenotypes consistently demonstrated hyperautofluorescent lesions on FAF, which corresponded to late-phase hypofluorescence on ICGA and ellipsoid zone disruption on OCT. Atypical cases showed a higher prevalence of vitritis (53% vs. 44%, P < 0.001), uveitic macular oedema (27% vs. 0%), and peripheral vascular leakage (73% vs. 28%, P = 0.004). Macular sensitivity improved by a mean of 1.7 dB/month (P = 0.005), with no significant difference observed between typical and atypical presentations.
Conclusion
This study broadens the clinical spectrum of ASPPC by characterising atypical funduscopically occult presentations. Despite phenotypic differences, all cases share identical MMI features, although atypical forms may exhibit more pronounced posterior segment inflammation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology. 1990;97:1281–7.
Mathew RG, Goh BT, Westcott MC. British ocular syphilis study (boss): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55:5394.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification Criteria for Syphilitic Uveitis. Am J Ophthalmol. 2021;228:182–91.
Gass JDM, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97:1288–97.
Eandi CM, Neri P, Adelman RA, Yannuzzi LA, Cunningham ET. Acute syphilitic posterior placoid chorioretinitis. Retina. 2012;32:1915–41.
Pichi F, Ciardella AP, Cunningham ET, Morara M, Veronese C, Jumper JM, et al. Spectral domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinopathy. Retina. 2014;34:373–84.
Villaret J, Errera M-H, Sahel J-A, Gaudric A, Mrejen S, Paques M. Indocyanine green angiography features in acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol. 2022;241:40–6.
Lima BR, Mandelcorn ED, Bakshi N, Nussenblatt RB, Nida Sen H. Syphilitic outer retinopathy. Ocul Immunol Inflamm. 2014;22:4–8.
Saleh MGA, Campbell JP, Yang P, Lin P. Ultra-wide-field fundus autofluorescence and spectral-domain optical coherence tomography findings in syphilitic outer retinitis. Ophthalmic Surg Lasers Imaging Retin. 2017;48:208–15.
Li K-H, Chen S-N. Diffuse phlebitis in patients with syphilitic outer retinopathy. Ocul Immunol Inflamm. 2021;29:1332–7.
Inoue S, Nishimura T, Takanashi N, Machida S. Retinal dysfunction of syphilitic outer retinopathy. Doc Ophthalmologica. 2020;141:187–93.
Amaral C, Joy L, Jimenez H, Cruz-Inñigo YJ, Ulloa-Padilla JP, Oliver AL. Syphilitic outer retinopathy: a case report and review of the literature. J Vitreoretin Dis. 2022;6:63–70.
Zafar S, Mishra K, Sachdeva MM. Syphilitic outer retinopathy: a masquerading diagnosis revealed after steroid-induced progression to panuveitis. Retin Cases Brief Rep. 2023;17:9–12.
Torjani A, Shahlaee A. Acute syphilitic outer retinopathy masquerading as atypical white dot syndrome. Ophthalmology. 2023;130:273.
Zeman L, Cartier MM, Couto C, Schlaen A. Optical Coherence Tomography Angiography findings in Syphilitic Outer Retinitis. Retin Cases Brief Rep. 2024. https://doi.org/10.1097/ICB.0000000000001706.
Mirzania D, Zacks DN, Zhou Y, Huvard MJ. Clinical characteristics and visual outcomes of acute syphilitic posterior placoid chorioretinopathy. Ophthalmol Retin. 2023;7:1080–6.
Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334–43.e1.
Battaglia Parodi M, Bianco L, Arrigo A, Saladino A, Antropoli A, Pina A, et al. Clinical correlation between optical coherence tomography biomarkers and retinal sensitivity in best vitelliform macular dystrophy. Transl Vis Sci Technol. 2022;11:24.
Cicinelli MV, Montesano G, Berni A, Scandale P, Ometto G, Introini U, et al. Photoreceptor integrity in MEWDS: longitudinal structure-function correlations. Invest Ophthalmol Vis Sci. 2024;65:28.
Menean M, Scandale P, Apuzzo A, Barresi C, Checchin L, L’Abbate G, et al. Unraveling the spectrum of uveitis: insights from an epidemiological study in a National Referral Center in Northern Italy. Ocul Immunol Inflamm. 2024: 1–6.
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Ramtohul P, Cabral D, Sadda S, Freund KB, Sarraf D. The OCT angular sign of Henle fiber layer (HFL) hyperreflectivity (ASHH) and the pathoanatomy of the HFL in macular disease. Prog Retin Eye Res. 2023;95:101135.
Pfau M, Jolly JK, Charng J, von der Emde L, Müller PL, Ansari G, et al. Multicenter normative data for mesopic microperimetry. Invest Ophthalmol Vis Sci. 2024;65:27.
Rissotto F, Scandale P, Miserocchi E. Ocular syphilis masquerading as CMV retinitis in a transplanted patient. Eur J Ophthalmol. 2024;34:NP108–12.
Tam J, Liu J, Dubra A, Fariss R. In vivo imaging of the human retinal pigment epithelial mosaic using adaptive optics enhanced indocyanine green ophthalmoscopy. Invest Ophthalmol Vis Sci. 2016;57:4376.
Gaudric A. Value and significance of hypofluorescent lesions seen on late-phase indocyanine green angiography. Ophthalmol Sci. 2024;4:100406.
Vidal-Villegas B, Arcos-Villegas G, Fernández-Vigo JI, Díaz-Valle D. Atypical syphilitic outer retinitis and severe retinal vasculitis as onset manifestations in a patient with concurrent HIV and syphilis infection. Ocul Immunol Inflamm. 2022;30:16–20.
Chen A, Seddon I, Rhead J, Browning DJ. Near Infrared Reflectance Imaging Changes in Acute Syphilitic Outer Retinitis. Ophthalmol Retina. 2026;10:102–8.
Northey LC, Skalicky SE, Gurbaxani A, McCluskey PJ. Syphilitic uveitis and optic neuritis in Sydney, Australia. Br J Ophthalmol. 2015;99:1215–9.
Gaudric A, Mrejen S. Why the dots are black only in the late phase of the indocyanine green angiography in multiple evanescent white dot syndrome. Retin Cases Brief Rep. 2017;11:S81–5.
Russell JF, Pichi F, Scott NL, Hartley MJ, Bell D, Agarwal A, et al. Masqueraders of multiple evanescent white dot syndrome (MEWDS). Int Ophthalmol. 2020;40:627–38.
Cicinelli MV, Ramtohul P, Marchese A, Bandello F, Bailey Freund K, Miserocchi E, et al. Latest advances in white spot syndromes: new findings and interpretations. Prog Retin Eye Res. 2023;97:101207.
Fouad YA, Bianco L, Ramtohul P, Touhami S, Gupta R, Mohammadi S, et al. Multiple evanescent white dot syndrome: typical, atypical, and secondary variants. Prog Retin Eye Res. 2026;110:101420.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the conception or design of the work (LB, MVC, AM), the acquisition (LBi, MM, AP, AA), analysis (LBi, LBo, MM, AP, AA), and interpretation of data (MVC, LB, EM, FB), drafting of the work (LB, MVC, AM, EM), revising it critically for intellectual content (LB, MVC, AM, EM, FB). Each of the coauthors has seen and agrees with the way his or her name is listed.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interest in publishing the present work or conflict of interest to disclose. Francesco Bandello discloses consulting fees for Abbvie, Alimera Sciences, Bayer, Boehringer-ingelheim, Fidia-sooft, Hofmann-La-Roche, Novartis, NTC pharma, Oxurion NV, SIFI.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bianco, L., Cicinelli, M.V., Marchese, A. et al. Beyond placoid: diverse clinical presentations and functional outcomes of acute syphilitic posterior placoid chorioretinopathy. Eye (2026). https://doi.org/10.1038/s41433-026-04272-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41433-026-04272-z