Abstract
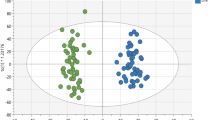
HLA-B27 positivity is strongly associated with acute anterior uveitis (AAU). This study investigated HLA-B27-dependent metabolic alterations in AAU and identified potential biomarkers of disease activity using plasma metabolomics. Untargeted and targeted metabolomics were employed to compare plasma metabolic profiles of HLA-B27-positive and negative patients. Distinct metabolic signatures, characterised by significant alterations in pyruvic acid and L-kynurenine, were identified in HLA-B27-positive individuals compared to HLA-B27-negative individuals. Furthermore, citric acid levels in these HLA-B27-positive patients correlated significantly with disease activity, particularly in those not receiving systemic medication. Pathway analysis revealed significant differences between HLA-B27-positive and negative patients in several key metabolic pathways, including the citrate cycle, tryptophan metabolism, pyruvate metabolism, and glycolysis/gluconeogenesis. A diagnostic model with citric acid alongside C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) demonstrated improved performance in predicting disease activity compared to a model utilising CRP and ESR alone (AUC: 0.727 vs. 0.713 and 0.674 vs. 0.670 in the untargeted and targeted cohorts, respectively). These findings offer insights into the metabolic dysregulation associated with HLA-B27-positive AAU and suggest that citric acid may be a potential biomarker for assessing disease activity, warranting further validation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The clinical datasets supporting this study are restricted due to ethical and legal constraints. However, qualified researchers affiliated with academic institutions may apply for access by contacting corresponding author. Data release is subject to proposal approval by the management committee and the execution of a formal data access agreement.
References
Sobrin L, Pistilli M, Dreger K, Kothari S, Khachatryan N, Artornsombudh P, et al. Factors predictive of remission of chronic anterior uveitis. Ophthalmology. 2020;127:826–34.
Monnet D, Breban M, Hudry C, Dougados M, Brezin AP. Ophthalmic findings and frequency of extraocular manifestations in patients with HLA-B27 uveitis: a study of 175 cases. Ophthalmology. 2004;111:802–9.
Yang P, Wan W, Du L, Zhou Q, Qi J, Liang L, et al. Clinical features of HLA-B27-positive acute anterior uveitis with or without ankylosing spondylitis in a Chinese cohort. Br J Ophthalmol. 2018;102:215–9.
Rosenbaum JT, Asquith M. The microbiome and HLA-B27-associated acute anterior uveitis. Nat Rev Rheumatol. 2018;14:704–13.
Britanova OV, Lupyr KR, Staroverov DB, Shagina IA, Aleksandrov AA, Ustyugov YY, et al. Targeted depletion of TRBV9(+) T cells as immunotherapy in a patient with ankylosing spondylitis. Nat Med. 2023;29:2731–6.
Yang X, Garner LI, Zvyagin IV, Paley MA, Komech EA, Jude KM, et al. Autoimmunity-associated T cell receptors recognize HLA-B*27-bound peptides. Nature. 2022;612:771–7.
Paley MA, Yang X, Hassman LM, Penkava F, Garner LI, Paley GL, et al. Mucosal signatures of pathogenic T cells in HLA-B*27+ anterior uveitis and axial spondyloarthritis. JCI Insight. 2024;9:e174776.
Parthasarathy R, Santiago F, McCluskey P, Kaakoush NO, Tedla N, Wakefield D. The microbiome in HLA-B27-associated disease: implications for acute anterior uveitis and recommendations for future studies. Trends Microbiol. 2023;31:142–58.
Essex, Rios M, Rodriguez V, Rademacher J, Proft F, Löber U, et al. Shared and distinct gut microbiota in spondyloarthritis, acute anterior uveitis, and Crohn’s disease. Arthritis Rheumatol. 2023;76:48–58.
Morandi SC, Herzog EL, Munk M, Kreuzer M, Largiadèr CR, Wolf S, et al. The gut microbiome and HLA-B27-associated anterior uveitis: a case-control study. J Neuroinflamm. 2024;21:120.
Huang X, Ye Z, Cao Q, Su G, Wang Q, Deng J, et al. Gut microbiota composition and fecal metabolic phenotype in patients with acute anterior uveitis. Investig Ophthalmol Vis Sci. 2018;59:1523–31.
Wang W, Yang GJ, Zhang J, Chen C, Jia ZY, Li J, et al. Plasma, urine and ligament tissue metabolite profiling reveals potential biomarkers of ankylosing spondylitis using NMR-based metabolic profiles. Arthritis Res Ther. 2016;18:244.
Zheng W, Wu X, Goudarzi M, Shi J, Song W, Li C, et al. Metabolomic alterations associated with Behçet’s disease. Arthritis Res Ther. 2018;20:214.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature Working G. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Salek RM, Steinbeck C, Viant MR, Goodacre R, Dunn WB. The role of reporting standards for metabolite annotation and identification in metabolomic studies. Gigascience. 2013;2:13.
Xie G, Wang L, Chen T, Zhou K, Zhang Z, Li J, et al. A metabolite array technology for precision medicine. Anal Chem. 2021;93:5709–17.
Brodie JT, Thotathil AZ, Jordan CA, Sims J, Niederer RL. Risk of recurrence in acute anterior uveitis. Ophthalmology. 2024;131:1281-1289.
Verhagen FH, Stigter ECA, Pras-Raves ML, Burgering BMT, Imhof SM, Radstake TRDJ, et al. Aqueous humor analysis identifies higher branched chain amino acid metabolism as a marker for human leukocyte antigen-B27 acute anterior uveitis and disease activity. Am J Ophthalmol. 2019;198:97–110.
Eryavuz Onmaz D, Sivrikaya A, Isik K, Abusoglu S, Albayrak Gezer I, Humeyra Yerlikaya F, et al. Altered kynurenine pathway metabolism in patients with ankylosing spondylitis. Int Immunopharmacol. 2021;99:108018.
Witoszyńska-Sobkowiak J, Sikorska D, Rutkowski R, Niklas K, Żychowska I, Samborski W. Treatment of ankylosing spondylitis with TNFα inhibitors does not affect serum levels of tryptophan metabolites. Inflammopharmacology. 2023;31:2393–400.
Nikolaus S, Schulte B, Al-Massad N, Thieme F, Schulte DM, Bethge J, et al. Increased tryptophan metabolism is associated with activity of inflammatory bowel diseases. Gastroenterology. 2017;153:1504–16.e2.
Platten M, Nollen EAA, Röhrig UF, Fallarino F, Opitz CA. Tryptophan metabolism as a common therapeutic target in cancer, neurodegeneration and beyond. Nat Rev Drug Discov. 2019;18:379–401.
Sen R, Kim E, Napier RJ, Cheng E, Fernandez A, Manning ES, et al. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as biomarkers in axial spondyloarthritis: observational studies from the program to understand the longterm outcomes in spondyloarthritis registry. Arthritis Rheumatol. 2023;75:232–41.
Lee EK, Lee S-Y, Kim BH, Park UC, Yu HG. Visual prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in BehÇet Uveitis. Retina. 2022;42:1189–98.
Ozgonul C, Sertoglu E, Ayyildiz O, Mumcuoglu T, Kucukevcilioglu M, Gokce G, Durukan AH. Novel biomarkers for patients with idiopathic acute anterior uveitis: neutrophil to lymphocyte ratio and platelet to lymphocyte ratio. Int J Ophthalmol. 2017;10:262.
Yildiz Balci S, Turan-Vural E, Turkyilmaz O, Esen F, Aksaray S. Complete blood count parameters and neutrophil-to-lymphocyte ratio values as markers for differentiation between systemic infectious and non-infectious uveitis. Int Ophthalmol. 2020;40:3033–41.
Kim M, Park Y-G, Park Y-H. C-reactive protein/albumin ratio as an indicator of disease activity in Behçet’s disease and human leukocyte antigen-B27-associated uveitis. Graefe’s Arch Clin Exp Ophthalmol. 2021;259:1985–92.
Grumet P, Kodjikian L, de Parisot A, Errera M-H, Sedira N, Heron E, et al. Contribution of diagnostic tests for the etiological assessment of uveitis, data from the ULISSE study (Uveitis: Clinical and medicoeconomic evaluation of a standardized strategy of the etiological diagnosis). Autoimmun Rev. 2018;17:331–43.
Gargaro M, Scalisi G, Manni G, Briseño CG, Bagadia P, Durai V, et al. Indoleamine 2,3-dioxygenase 1 activation in mature cDC1 promotes tolerogenic education of inflammatory cDC2 via metabolic communication. Immunity. 2022;55:1032–50.e14.
Zhang L, Ma J, Takeuchi M, Usui Y, Hattori T, Okunuki Y, et al. Suppression of experimental autoimmune uveoretinitis by inducing differentiation of regulatory T cells via activation of aryl hydrocarbon receptor. Investig Opthalmol Vis Sci. 2010;51:2109–17.
Nugent LF, Shi G, Vistica BP, Ogbeifun O, Hinshaw SJH, Gery I. ITE, A Novel Endogenous Nontoxic Aryl Hydrocarbon Receptor Ligand, Efficiently Suppresses EAU and T-Cell–Mediated Immunity. Investigative Opthalmology & Visual Science. 2013;54.
Huang Y, He J, Liang H, Hu K, Jiang S, Yang L, et al. Aryl Hydrocarbon receptor regulates apoptosis and inflammation in a murine model of experimental autoimmune uveitis. Front Immunol. 2018;9:1713.
Angiari S, Runtsch MC, Sutton CE, Palsson-McDermott EM, Kelly B, Rana N, et al. Pharmacological activation of pyruvate kinase M2 Inhibits CD4(+) T cell pathogenicity and suppresses autoimmunity. Cell Metab. 2020;31:391–405.e8.
Liu Z, Xu J, Li H, Shu J, Su G, Zhou C, et al. PD-1 Targeted nanoparticles inhibit activated T cells and alleviate autoimmunity via suppression of cellular energy metabolism mediated by PKM2. Int J Nanomed. 2022;17:1711–24.
Funding
Supported by 82025009, 80220071 from The National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
XZ, JD, JQ, and YW contributed to the design of the clinical cohorts. KW, XJ, BX, MD, YT, RC, HW, DL, XG, and RL contributed to the collection of blood samples and clinical information. KW and XJ performed data analyses. XZ and JD contributed to statistical guidance and review. KW and XJ wrote the manuscript. XZ and JD guided the study and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, K., Ji, X., Xie, B. et al. Plasma metabolomics reveals distinct metabolic alterations and biomarkers of disease activity in HLA-B27-positive acute anterior uveitis. Eye (2026). https://doi.org/10.1038/s41433-026-04307-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41433-026-04307-5