Abstract
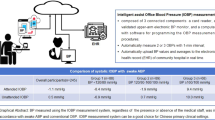
We aimed to assess the difference in the accuracy of readings from automated office blood pressure machines with each other or with manual office blood pressure measurements in Chinese individuals. We collected awake 48-h ambulatory blood pressure monitoring, two automated office blood pressure device (BpTRU and WatchBP) readings, and manual office blood pressure measurements in Chinese patients (n = 135) with hypertension in a randomized sequence. Differences were compared using paired t-tests and Bland–Altman plots. The sensitivity and specificity of the techniques for detecting elevated blood pressure were calculated using awake ambulatory blood pressure monitoring as the reference standard. The WatchBP device’s and awake ambulatory blood pressure readings were similar. The BpTRU device provided significantly lower mean systolic (P < 0.001) and diastolic (P < 0.001) blood pressure readings, while manual office BP provided significantly higher mean systolic (P = 0.008) and diastolic (P < 0.001) blood pressure readings than the awake automated office blood pressure readings. Automated and manual office blood pressure measurements showed similar sensitivity, specificity, and 95% limits of agreement as based on Bland–Altman plots. The mean systolic (P < 0.001) and diastolic (P < 0.02) blood pressure readings of WatchBP and BpTRU differed, and their diagnostic performances were not superior than those of manual office blood pressure measurements in Chinese patients. Therefore, automated office blood pressure measurements cannot be routinely recommended for Chinese individuals in clinical practice. More studies are needed to confirm these results.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hypertension in adults: diagnosis and Hypertension in adults: diagnosis and management management NICE guideline. 2019. www.nice.org.uk/guidance/ng136.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162:192–204.
Lee EKPP, Yeung NCYY, Xu Z, Zhang D, Yu C-PP, Wong SYSS. Effect and acceptability of mindfulness-based stress reduction program on patients with elevated blood pressure or hypertension: a meta-analysis of randomized controlled trials. Hypertension. 2020;76:1992–2001.
Gorostidi M, Vinyoles E, Banegas JR, De La Sierra A. Prevalence of white-coat and masked hypertension in national and international registries. Hypertension Res. 2015;38:1–7.
Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension. 2010;55:195–200.
Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada’s 2018 Guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506–25.
Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Intern Med. 2019;179:351–62.
Pappaccogli M, Di Monaco S, Perlo E, Burrello J, D’Ascenzo F, Veglio F. et al. Comparison of automated office blood pressure with office and out-off-office measurement techniques. Hypertension. 2019;73:481–90. https://doi.org/10.1161/HYPERTENSIONAHA.118.12079.
Myers MG, Kaczorowski J, Dawes M, Godwin M. Automated office blood pressure measurement in primary care. Can Fam Physician. 2014;60:127–32.
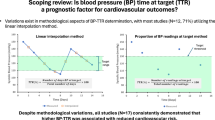
Bo Y, Kwok KO, Chu KKY, Leung EYH, Yu CP, Wong SYS. et al. Comparison between automated office blood pressure measurements and manual office blood pressure measurements—implications in individual patients: a systematic review and meta-analysis. Curr Hypertens Rep. 2021;23:1–12. https://doi.org/10.1007/s11906-020-01118-1.
Sheppard JP, Holder R, Nichols L, Bray E, Richard Hobbs FD, Mant J, et al. Predicting out-of-office blood pressure level using repeated measurements in the clinic: an observational cohort study. J Hypertens. 2014;32:2171.
Andreadis EA, Agaliotis GD, Angelopoulos ET, Tsakanikas AP, Chaveles IA, Mousoulis GP. Automated office blood pressure and 24-h ambulatory measurements are equally associated with left ventricular mass index. Am J Hypertension. 2011;24:661–6.
Andreadis EA, Agaliotis GD, Angelopoulos ET, Tsakanikas AP, Kolyvas GN, Mousoulis GP. Automated office blood pressure is associated with urine albumin excretion in hypertensive subjects. Am J Hypertens. 2012;25:969–73.
Andreadis EA, Geladari CV, Angelopoulos ET, Kolyvas GN, Papademetriou V. Morning surge and peak morning ambulatory blood pressure versus automated office blood pressure in predicting cardiovascular disease. High Blood Press Cardiovasc Prev. 2019;26:209–15.
Armstrong D, Matangi M, Brouillard D, Myers MG. Automated office blood pressure-being alone and not location is what matters most. Blood Press Monit. 2015;20:204–8.
Beckett L, Godwin M. The BpTRU automatic blood pressure monitor compared to 24h ambulatory blood pressure monitoring in the assessment of blood pressure in patients with hypertension. BMC Cardiovasc Disord. 2005;5:18.
Crippa G, Cassi A, Bosi M, Fares M. Usefulness of automated office blood pressure measurement by bptru for the diagnosis of resistant hypertension. J Clin Hypertens. 2011;13:A124.
Crippa G, Cassi A, Bosi M, Fares M. Usefulness of multiple blood pressure measurements using an automated oscillometric monitor (BpTRU) during a campaign for cardiovascular prevention. J Clin Hypertens. 2010;12:A18–147.
Edwards C, Hiremath S, Gupta A, McCormick BB, Ruzicka M. BpTRUth: do automated blood pressure monitors outperform mercury? J Am Soc Hypertens. 2013;7:448–53.
Godwin M, Birtwhistle R, Delva D, Lam M, Casson I, MacDonald S, et al. Manual and automated office measurements in relation to awake ambulatory blood pressure monitoring. Fam Pr. 2011;28:110–7.
Michaud A, Lamarre-Cliche M, Cloutier L. Screening for hypertension: an elevated office blood pressure measurement is valuable, adding an automated one is even better. Blood Press Monit. 2019;24:123–9.
Myers MG, Valdivieso MA. Use of an automated blood pressure recording device, the BpTRU, to reduce the “white coat effect” in routine practice. Am J Hypertens. 2003;16:494–7.
Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens. 2009;27:280–6.
D’Sa L, Senaratne N, Woodcock-Smith J, Miles KM, Wilkinson IB, McEniery CM. Evaluation of the Omron HEM-907 automated blood pressure device: comparison with office and ambulatory blood pressure readings. Hypertens Res. 2019;42:52–58.
Armanyous S, Ohashi Y, Lioudis M, Schold JD, Thomas G, Poggio ED, et al. Diagnostic performance of blood pressure measurement modalities in living kidney donor candidates. Clin J Am Soc Nephrol. 2019;14:738–46.
Mattu GS, Heran BS, Wright JM. Overall accuracy of the BpTRUTM—an automated electronic blood pressure device. Blood Press Monit. 2004;9:47–52.
Stergiou GS, Tzamouranis D, Protogerou A, Nasothimiou E, Kapralos C. Validation of the Microlife Watch BP Office professional device for office blood pressure measurement according to the International protocol. Blood Press Monit. 2008;13:299–303.
Kang Y-Y, Li Y, Huang Q-F, Song J, Shan X-L, Dou Y, et al. Accuracy of home versus ambulatory blood pressure monitoring in the diagnosis of white-coat and masked hypertension. J Hypertens. 2015;33:1580–7.
Lee EKP, Choi RCM, Liu L, Gao T, Yip BHK, Wong SYS. Preference of blood pressure measurement methods by primary care doctors in Hong Kong: a cross-sectional survey. BMC Famliy Pr. 2020;21:1–9.
Primary Care Office, Department of Health H. Hong Kong Reference Framework for Hypertension Care for Adults in Primary Care Settings 2013. Hong Kong; 2013. http://www.pco.gov.hk/english/resource/files/RF_HT_full.pdf.
Filipovský J, Seidlerová J, Ceral J, Vysočanová P, Špác J, Souček M, et al. A multicentre study on unattended automated office blood pressure measurement in treated hypertensive patients. Blood Press. 2018;28:34–39.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
British Hypertension Society: BP Monitors. http://bhsoc.org/bp-monitors/bp-monitors/.
Zeng WF, Liu M, Kang YY, Li Y, Wang JG. Validation of the fully automated A&D TM-2656 blood pressure monitor according to the British Hypertension Society Protocol. Blood Press Monit. 2013;18:223–6.
Matsuoka M, Inoue T, Shinjo T, Miiji A, Tamashiro M, Oba K. et al. Cardiovascular risk profile and frailty in Japanese outpatients: the Nambu Cohort Study. Hypertens Res. 2020;43:817–23. https://doi.org/10.1038/s41440-020-0427-z.
Wan Z, Hu L, Hu M, Lei X, Huang Y, Lv Y. Helicobacter pylori infection and prevalence of high blood pressure among Chinese adults. J Hum Hypertens. 2018;32:158–64. https://doi.org/10.1038/s41371-017-0028-8.
Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24:52–58.
Lamarre-Cliché M, Cheong NNG, Larochelle P. Comparative assessment of four blood pressure measurement methods in hypertensives. Can J Cardiol. 2011;27:455–60.
Gill P, Haque MS, Martin U, Mant J, Mohammed MA, Heer G, et al. Measurement of blood pressure for the diagnosis and management of hypertension in different ethnic groups: one size fits all. BMC Cardiovasc Disord. 2017;17:55.
Martin U, Haque MS, Wood S, Greenfield SM, Gill PS, Mant J, et al. Ethnicity and differences between clinic and ambulatory blood pressure measurements. Am J Hypertens. 2015;28:729–38.
Myers MG, Valdivieso M, Kiss A, Tobe SW. Comparison of two automated sphygmomanometers for use in the office setting. Blood Press Monit. 2009;14:45–47.
Padwal RS, Majumdar SR. Comparability of two commonly used automated office blood pressure devices in the severely obese. Blood Press Monit. 2016;21:313–5.
Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30:449–56.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) Study. Circulation. 2005;111:1777–83.
Acknowledgements
The authors would like to thank all the participants in the study and all the nurses in the Lek Yuen Clinic for their help with the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lee, E.K.P., Zhu, M., Chan, D.C.C. et al. Comparative accuracies of automated and manual office blood pressure measurements in a Chinese population. Hypertens Res 45, 324–332 (2022). https://doi.org/10.1038/s41440-021-00779-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-021-00779-y
Keywords
This article is cited by
-
Update on Hypertension Research in 2021
Hypertension Research (2022)