Abstract
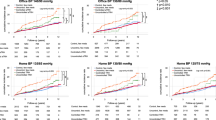
This study aimed to identify the metabolomic alterations associated with hypertension (HTN) and the response of blood pressure (BP) to thiazide diuretics. A total of 50 participants previously untreated for HTN were prospectively recruited. After a 2-week lifestyle adjustment, 30 participants with systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg were classified into the HTN group and prescribed hydrochlorothiazide (HCTZ) at 50 mg per day for 2 weeks. The remaining 20 participants, who had relatively normal BP, were assigned to the normotension group. Metabolomic profiles related to the response of BP to thiazide diuretics were analyzed. A total of 73 differential metabolites were found to be associated with HTN, and 27 metabolites were significantly changed upon HCTZ treatment (HCTZ-sensitive metabolites). Among the identified metabolites, 7 (aspartate, histidine, C5-DC, C5-M-DC, C14:1, phosphatidylcholine ae C34:1, and phosphatidylcholine ae C34:3) were positively associated with HTN and decreased in abundance upon HCTZ treatment (HCTZ-reduced/HTN-associated metabolites). Moreover, multivariate analysis of 20 metabolites whose baseline levels were associated with the response of BP revealed that aspartate, glutamate, lysophosphatidylcholine C16:0, lysophosphatidylcholine C20:3, and sphingomyelin C24:1 were independently related to systolic BP reduction, and lysophosphatidylcholine C20:3 was independently associated with diastolic BP reduction. In conclusion, we identified 5 metabolites independently related to BP changes with HCTZ treatment. An advanced biomarker profile of thiazide-induced metabolomic changes may provide a clue with which to further explore the complex and mixed effects of thiazide treatment in a clinical setting.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808.
Zhou B, Danaei G, Stevens GA, Bixby H, Taddei C, Carrillo-Larco RM, et al. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639–51.
Obermüller N, Bernstein P, Velázquez H, Reilly R, Moser D, Ellison DH, et al. Expression of the thiazide-sensitive Na-Cl cotransporter in rat and human kidney. Am J Physiol. 1995;269:F900–F910.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–97.
Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289:2534–44.
Suchard MA, Schuemie MJ, Krumholz HM, You SC, Chen R, Pratt N, et al. Comprehensive comparative effectiveness and safety of first-line antihypertensive drug classes: a systematic, multinational, large-scale analysis. Lancet. 2019;394:1816–26.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American heart association. Hypertension. 2018;72:e53–e90.
Turner ST, Schwartz GL, Chapman AB, Boerwinkle E. WNK1 kinase polymorphism and blood pressure response to a thiazide diuretic. Hypertension. 2005;46:758–65.
Turner ST, Bailey KR, Fridley BL, Chapman AB, Schwartz GL, Chai HS, et al. Genomic association analysis suggests chromosome 12 locus influencing antihypertensive response to thiazide diuretic. Hypertension. 2008;52:359–65.
Salvi E, Wang Z, Rizzi F, Gong Y, McDonough CW, Padmanabhan S, et al. Genome-wide and gene-based meta-analyses identify novel loci influencing blood pressure response to hydrochlorothiazide. Hypertension. 2017;69:51–59.
Shahin MH, Sá AC, Webb A, Gong Y, Langaee T, McDonough CW, et al. Genome-wide prioritization and transcriptomics reveal novel signatures associated with thiazide diuretics blood pressure response. Circ Cardiovasc Genet. 2017;10:e001404.
Sá ACC, Webb A, Gong Y, McDonough CW, Shahin MH, Datta S, et al. Blood pressure signature genes and blood pressure response to thiazide diuretics: results from the PEAR and PEAR-2 studies. BMC Med Genomics. 2018;11:55.
Singh S, McDonough CW, Gong Y, Bailey KR, Boerwinkle E, Chapman AB, et al. Genome wide analysis approach suggests chromosome 2 locus to be associated with thiazide and thiazide like-diuretics blood Pressure Response. Sci Rep. 2019;9:17323.
Huang CC, Chung CM, Hung SI, Leu HB, Wu TC, Huang PH, et al. Genetic variation in renin predicts the effects of thiazide diuretics. Eur J Clin Invest. 2011;41:828–35.
Shahin MH, Gong Y, McDonough CW, Rotroff DM, Beitelshees AL, Garrett TJ, et al. A genetic response score for hydrochlorothiazide use: insights from genomics and metabolomics integration. Hypertension. 2016;68:621–9.
Shahin MH, Gong Y, Frye RF, Rotroff DM, Beitelshees AL, Baillie RA, et al. Sphingolipid metabolic pathway impacts thiazide diuretics blood pressure response: insights from genomics, metabolomics, and lipidomics. J Am Heart Assoc. 2017;7:e006656.
Trabado S, Al-Salameh A, Croixmarie V, Masson P, Corruble E, Fève B, et al. The human plasma-metabolome: Reference values in 800 French healthy volunteers; impact of cholesterol, gender and age. PLoS One. 2017;12:e0173615.
Varma VR, Oommen AM, Varma S, Casanova R, An Y, Andrews RM, et al. Brain and blood metabolite signatures of pathology and progression in Alzheimer disease: a targeted metabolomics study. PLoS Med. 2018;15:e1002482.
Goïta Y, Chao de la Barca JM, Keïta A, Diarra MB, Dembélé KC, Chabrun F, et al. Sexual dimorphism of metabolomic profile in arterial hypertension. Sci Rep. 2020;10:7517.
Dietrich S, Floegel A, Weikert C, Prehn C, Adamski J, Pischon T, et al. Identification of serum metabolites associated with incident hypertension in the european prospective investigation into cancer and nutrition-potsdam study. Hypertension. 2016;68:471–7.
Lin YT, Salihovic S, Fall T, Hammar U, Ingelsson E, Ärnlöv J, et al. Global Plasma metabolomics to identify potential biomarkers of blood pressure progression. Arterioscler Thromb Vasc Biol. 2020;40:e227–e237.
Hiltunen TP, Rimpelä JM, Mohney RP, Stirdivant SM, Kontula KK. Effects of four different antihypertensive drugs on plasma metabolomic profiles in patients with essential hypertension. PLoS One. 2017;12:e0187729.
Rotroff DM, Shahin MH, Gurley SB, Zhu H, Motsinger-Reif A, Meisner M, et al. Pharmacometabolomic assessments of atenolol and hydrochlorothiazide treatment reveal novel drug response phenotypes. CPT Pharmacomet Syst Pharm. 2015;4:669–79.
Kim M, Jung S, Kim SY, Lee SH, Lee JH. Prehypertension-associated elevation in circulating lysophosphatidlycholines, Lp-PLA2 activity, and oxidative stress. PLoS One. 2014;9:e96735.
Jiang H, Nie L, Li Y, Xie J. Application of ultra-performance liquid chromatography coupled with mass spectrometry to metabonomic study on spontaneously hypertensive rats and intervention effects of Ping Gan prescription. J Sep Sci. 2012;35:483–9.
Kim JY, Kim OY, Paik JK, Kwon DY, Kim HJ, Lee JH. Association of age-related changes in circulating intermediary lipid metabolites, inflammatory and oxidative stress markers, and arterial stiffness in middle-aged men. Age (Dordr). 2013;35:1507–19.
Hoover RS, Poch E, Monroy A, Vázquez N, Nishio T, Gamba G, et al. N-Glycosylation at two sites critically alters thiazide binding and activity of the rat thiazide-sensitive Na(+):Cl(-) cotransporter. J Am Soc Nephrol. 2003;14:271–82.
Li AP, Yang L, Cui T, Zhang LC, Liu YT, Yan Y, et al. Uncovering the mechanism of Astragali Radix against nephrotic syndrome by intergrating lipidomics and network pharmacology. Phytomedicine. 2020;77:153274.
Luo H, Beaumont K, Vaughn DA, Fanestil DD. Solubilization of thiazide diuretic receptors from rat kidney membranes. Biochim Biophys Acta. 1990;1052:119–22.
Welker P, Böhlick A, Mutig K, Salanova M, Kahl T, Schlüter H, et al. Renal Na+-K+-Cl- cotransporter activity and vasopressin-induced trafficking are lipid raft-dependent. Am J Physiol Ren Physiol. 2008;295:F789–F802.
Ke C, Zhu X, Zhang Y, Shen Y. Metabolomic characterization of hypertension and dyslipidemia. Metabolomics. 2018;14:117.
Zhao JV, Kwok MK, Schooling CM. Effect of glutamate and aspartate on ischemic heart disease, blood pressure, and diabetes: a Mendelian randomization study. Am J Clin Nutr. 2019;109:1197–206.
Hou E, Sun N, Zhang F, Zhao C, Usa K, Liang M, et al. Malate and aspartate increase L-arginine and nitric oxide and attenuate hypertension. Cell Rep. 2017;19:1631–9.
Acknowledgements
We thank Jie-Ling Li for her excellent technical support. This work was supported by research grants VGHUST108-G1-3-1, VGHUST108-G1-3-2, VGHUST108-G1-3-3, and V110C-058 from Taipei Veterans General Hospital, Taipei, Taiwan, and by research grants NSC 100-2314-B-075-055, MOST108-2314-B-075-062-MY3, and MOST 109-2311-B-010-003 from the Ministry of Science and Technology, Taiwan. The funders had no role in the study design, the data collection and analysis, the decision to publish, or the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, CC., Huang, YL., Lin, CH. et al. Plasma metabolomic profiles associated with hypertension and blood pressure in response to thiazide diuretics. Hypertens Res 45, 464–473 (2022). https://doi.org/10.1038/s41440-021-00825-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-021-00825-9
Keywords
This article is cited by
-
Identification of serum metabolic markers in non-obese hypertensive patients using non-targeted metabolomics
Scientific Reports (2025)
-
Metabolomic profiling in kidney cells treated with a sodium glucose-cotransporter 2 inhibitor
Scientific Reports (2023)
-
Do not take a chance! We do not tell fortunes
Hypertension Research (2022)