Abstract
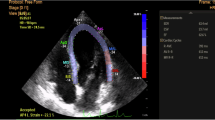
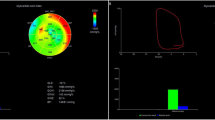
Minor ST-T changes on electrocardiograms are observed in patients with hypertensive heart disease with a preserved left ventricular ejection fraction (LVEF); however, the relationship between minor ST-T changes and global myocardial work on echocardiograms remains unclear. We evaluated the global longitudinal strain (GLS), global work index (GWI), global constructive work (GCW), global wasted work (GWW), and global work efficiency (GWE) in 186 hypertensive patients with preserved LVEF (>50%) using an offline analysis system (View Pal, GE). Minor ST-T changes as well as major ST-T changes (depression in ST in lead V5 > 1 mV) were also evaluated by electrocardiography. The mean age was 79.4 ± 8.2 years (men 37.6%). Patients with minor and major ST-changes had a smaller absolute GLS (−20.3 ± 3.1, −18.2 ± 3.7, and −15.2 ± 5.0%, P < 0.001) and a smaller constructive workload [GWI (2148 ± 486, 1938 ± 462, and 1685 ± 701 mmHg%, P = 0.002) and GCW (2419 ± 510, 2185 ± 466, and 1865 ± 702 mmHg%, P < 0.001)] than those with no ST-T changes. Additionally, patients with minor and major ST-T changes had increased wasted myocardial work [GWW (87 ± 61, 105 ± 56, and 127 ± 75 mmHg%, P = 0.045)], which resulted in reductions in the myocardial work efficiency [GWE (95 ± 4, 94 ± 3, and 89 ± 12%, P < 0.001)]. Even after adjustments for confounding factors, including EF, diastolic function parameters, LV hypertrophy, history of heart failure and atrial fibrillation, patients with minor ST-T changes had significantly smaller LV global constructive work in comparison to those without [GWI (2260 ± 33 vs. 2025 ± 76 mmHg%, P = 0.007) and GCW (2501 ± 45 vs. 2210 ± 105 mmHg%, P = 0.003)]. In conclusion, in hypertensive patients with preserved LVEF, minor ST-T changes on electrocardiograms were associated with reduced constructive work in the LV.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC) developed with the special contribution of the heart failure association (hfa) of the ESC. Eur Heart J. 2016;37:2129–2200.
Scheltens T, de Beus MF, Hoes AW, Rutten FH, Numans ME, Mosterd A, et al. The potential yield of ecg screening of hypertensive patients: the Utrecht health project. J Hypertens. 2010;28:1527–33.
Ishikawa J, Ishikawa S, Kabutoya T, Gotoh T, Kayaba K, Schwartz JE, et al. Cornell product left ventricular hypertrophy in electrocardiogram and the risk of stroke in a general population. Hypertension. 2009;53:28–34.
Ishikawa J, Ishikawa S, Kario K. Levels of Cornell voltage and Cornell product for predicting cardiovascular and stroke mortality and morbidity in the general Japanese population. Circ J. 2014;78:465–75.
Ishikawa J, Hirose H, Schwartz JE, Ishikawa S. Minor electrocardiographic st-t change and risk of stroke in the general Japanese population. Circ J. 2018;82:1797–804
Kumar A, Lloyd-Jones DM. Clinical significance of minor nonspecific st-segment and t-wave abnormalities in asymptomatic subjects: a systematic review. Cardiol Rev. 2007;15:133–42.
Hare JL, Brown JK, Marwick TH. Association of myocardial strain with left ventricular geometry and progression of hypertensive heart disease. Am J Cardiol. 2008;102:87–91.
Liu YW, Tsai WC, Su CT, Lin CC, Chen JH. Evidence of left ventricular systolic dysfunction detected by automated function imaging in patients with heart failure and preserved left ventricular ejection fraction. J Card Fail. 2009;15:782–9.
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, et al. A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2019;20:31–39.
Jentzer JC, Anavekar NS, Burstein BJ, Borlaug BA, Oh JK. Noninvasive echocardiographic left ventricular stroke work index predicts mortality in cardiac intensive care unit patients. Circ Cardiovasc Imaging. 2020;13:e011642.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (jsh 2019). Hypertens Res. 2019;42:1235–481.
Okin PM, Devereux RB, Gerdts E, Snapinn SM, Harris KE, Jern S, et al. for the LIFE Study Investigators. Impact of diabetes mellitus on regression of electrocardiographic left ventricular hypertrophy and the prediction of outcome during antihypertensive therapy: the losartan intervention for endpoint (life) reduction in hypertension study. Circulation. 2006;113:1588–96.
Schillaci G, Pirro M, Pasqualini L, Vaudo G, Ronti T, Gemelli F, et al. Prognostic significance of isolated, non-specific left ventricular repolarization abnormalities in hypertension. J Hypertens. 2004;22:407–14.
Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in m-mode echocardiography: Results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–83.
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American society of echocardiography committee on standards, subcommittee on quantitation of two-dimensional echocardiograms. J Am Soc Echocardiogr. 1989;2:358–67.
Samson R, Le Jemtel TH. Therapeutic stalemate in heart failure with preserved ejection fraction. J Am Heart Assoc. 2021;10:e021120.
Jaglan A, Roemer S, Perez Moreno AC, Khandheria BK. Myocardial work in stage 1 and 2 hypertensive patients. Eur Heart J Cardiovasc Imaging. 2021;22:744–50.
Wang T, Li L, Huang J, Fan L. Assessment of subclinical left ventricle myocardial dysfunction using global myocardial work in type 2 diabetes mellitus patients with preserved left ventricle ejection fraction. Diabetol Metab Syndr. 2022;14:17.
Edwards NFA, Scalia GM, Shiino K, Sabapathy S, Anderson B, Chamberlain R, et al. Global myocardial work is superior to global longitudinal strain to predict significant coronary artery disease in patients with normal left ventricular function and wall motion. J Am Soc Echocardiogr. 2019;32:947–57.
Li Y, Zheng Q, Cui C, Liu Y, Hu Y, Huang D, et al. Application value of myocardial work technology by non-invasive echocardiography in evaluating left ventricular function in patients with chronic heart failure. Quant Imaging Med Surg. 2021;12:244–56.
Manganaro R, Marchetta S, Dulgheru R, Sugimoto T, Tsugu T, Ilardi F, et al. Correlation between non-invasive myocardial work indices and main parameters of systolic and diastolic function: results from the eacvi norre study. Eur Heart J Cardiovasc Imaging. 2020;21:533–41.
Lakatos BK, Ruppert M, Tokodi M, Oláh A, Braun S, Karime C, et al. Myocardial work index: a marker of left ventricular contractility in pressure- or volume overload-induced heart failure. ESC Heart Fail. 2021;8:2220–31.
Acknowledgements
The first author currently belongs to the Department of Cardiology, Tokyo Metropolitan Tama Medical Center (Tokyo, Japan).
Funding
This study was supported in part by a grant from the Tokyo Metropolitan Geriatric Hospital and Institute of Gerontology. The corresponding author (JI) was supported in part by a research grant from Tokyo Metropolitan Geriatric Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakamura, S., Ishikawa, J., Sakurayama, C. et al. Minor ST-T changes on electrocardiograms are associated with reduced constructive myocardial work in hypertensive patients with a preserved ejection fraction. Hypertens Res 45, 1373–1381 (2022). https://doi.org/10.1038/s41440-022-00957-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-022-00957-6