Abstract
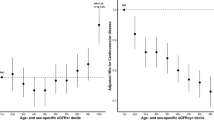
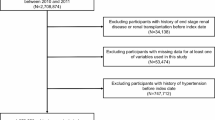
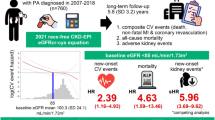
Plasma total homocysteine (tHcy) and kidney function are both associated with mortality risk, but the degree to which kidney function modifies the impact of tHcy on mortality remains unknown. This prospective cohort study included a total of 14,225 hypertensive adults. Cox proportional hazard regression was used to analyze the separate and combined association of tHcy and estimated glomerular filtration rate (eGFR) with all-cause and cause-specific mortality. Mediation analysis was conducted to explore the mediating effect of eGFR. During a median follow-up of 4.0 years, 805 deaths were identified, including 397 deaths from cardiovascular disease (CVD). There were significant, positive relationships of tHcy with all-cause mortality (per 5 μmol/L; HR: 1.09; 95% CI: 1.07, 1.11), CVD mortality (HR: 1.11; 95% CI: 1.08, 1.13), and non-CVD mortality (HR: 1.07; 95% CI: 1.04, 1.10). The proportions of eGFR mediating these relationships were 39.1%, 35.7%, and 49.7%, respectively. There were additive interactions between tHcy and eGFR. Compared with those with low tHcy (<15 μmol/L) and high eGFR (≥90 mL·min−1·1.73 m−2), participants with high tHcy (≥20 μmol/L) and low eGFR (<60 mL·min−1·1.73 m−2) had the highest risk of all-cause mortality (HR: 4.89; 95% CI: 3.81, 6.28), CVD mortality (HR: 5.80; 95% CI: 4.01, 8.40), and non-CVD mortality (HR: 4.25; 95% CI: 3.02, 5.97). In conclusion, among Chinese hypertensive adults, high tHcy and impaired kidney function were independently and jointly associated with higher risks of all-cause and cause-specific mortality. Importantly, kidney function explained most (nearly 40%) of the increased risk of mortality conferred by high tHcy.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–32.
Towfighi A, Markovic D, Ovbiagele B. Pronounced association of elevated serum homocysteine with stroke in subgroups of individuals: a nationwide study. J Neurol Sci. 2010;298:153–7.
McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol. 1969;56:111–28.
Hankey GJ, Eikelboom JW. Homocysteine and vascular disease. Lancet 1999;354:407–13.
Clarke R, Collins R, Lewington S, Donald A, Alfthan G, Tuomilehto J, et al. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA 2002;288:2015–22.
Yuan S, Mason AM, Carter P, Burgess S, Larsson SC. Homocysteine, B vitamins, and cardiovascular disease: a Mendelian randomization study. BMC Med. 2021;19:97.
Jiang S, Li J, Zhang Y, Venners SA, Tang G, Wang Y, et al. Methylenetetrahydrofolate reductase C677T polymorphism, hypertension and risk of stroke: a prospective, nested case-control study. Int J Neurosci. 2017;127:253–60.
Li J, Jiang S, Zhang Y, Tang G, Wang Y, Mao G, et al. H-type hypertension and risk of stroke in Chinese adults: A prospective, nested case-control study. J Transl Int Med. 2015;3:171–8.
Tu W, Yan F, Chao B, Ji X, Wang L. Status of hyperhomocysteinemia in China: results from the China Stroke High-risk Population Screening Program, 2018. Front Med. 2021;15:903–12.
Collaboration GBDCKD. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020;395:709–33.
Cianciolo G, De Pascalis A, Di Lullo L, Ronco C, Zannini C, La Manna G. Folic Acid and Homocysteine in Chronic Kidney Disease and Cardiovascular Disease Progression: Which Comes First? Cardiorenal Med. 2017;7:255–66.
Shi Y, Ding C, Hu L, Li M, Huang X, Zhou W, et al. Saturation Effects of Plasma Homocysteine on Chronic Kidney Disease in Chinese Adults With H-type Hypertension: A Cross-sectional Study. J Ren Nutr. 2021;31:459–66.
Park S, Lee S, Kim Y, Cho S, Kim K, Kim YC, et al. Causal Effects of Homocysteine, Folate, and Cobalamin on Kidney Function: A Mendelian Randomization Study. Nutrients 2021;13:906.
Menon V, Wang X, Greene T, Beck GJ, Kusek JW, Selhub J, et al. Homocysteine in chronic kidney disease: Effect of low protein diet and repletion with B vitamins. Kidney Int. 2005;67:1539–46.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–69.
Shi Z, Guan Y, Huo YR, Liu S, Zhang M, Lu H, et al. Elevated Total Homocysteine Levels in Acute Ischemic Stroke Are Associated With Long-Term Mortality. Stroke. 2015;46:2419–25.
Nygard O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997;337:230–6.
Hoogeveen EK, Kostense PJ, Jakobs C, Dekker JM, Nijpels G, Heine RJ, et al. Hyperhomocysteinemia increases risk of death, especially in type 2 diabetes: 5-year follow-up of the Hoorn Study. Circulation. 2000;101:1506–11.
Lu J, Chen K, Chen W, Liu C, Jiang X, Ma Z, et al. Association of Serum Homocysteine with Cardiovascular and All-Cause Mortality in Adults with Diabetes: A Prospective Cohort Study. Oxid Med Cell Longev. 2022;2022:2156483.
Dangour AD, Breeze E, Clarke R, Shetty PS, Uauy R, Fletcher AE. Plasma homocysteine, but not folate or vitamin B-12, predicts mortality in older people in the United Kingdom. J Nutr. 2008;138:1121–8.
Xiu LL, Lee MS, Wahlqvist ML, Chen RC, Huang YC, Chen KJ, et al. Low and high homocysteine are associated with mortality independent of B group vitamins but interactive with cognitive status in a free-living elderly cohort. Nutr Res. 2012;32:928–39.
Mendonca N, Jagger C, Granic A, Martin-Ruiz C, Mathers JC, Seal CJ, et al. Elevated Total Homocysteine in All Participants and Plasma Vitamin B12 Concentrations in Women Are Associated With All-Cause and Cardiovascular Mortality in the Very Old: The Newcastle 85+ Study. J Gerontol A Biol Sci Med Sci. 2018;73:1258–64.
Vollset SE, Refsum H, Tverdal A, Nygard O, Nordrehaug JE, Tell GS, et al. Plasma total homocysteine and cardiovascular and noncardiovascular mortality: the Hordaland Homocysteine Study. Am J Clin Nutr. 2001;74:130–6.
Waskiewicz A, Sygnowska E, Broda G. Homocysteine concentration and the risk of death in the adult Polish population. Kardiol Pol. 2012;70:897–902.
Mo T, Long P, Wang Y, Peng R, Niu R, Wang Q, et al. Genetic susceptibility, homocysteine levels, and risk of all-cause and cause-specific mortality: A prospective cohort study. Clin Chim Acta. 2023;538:1–8.
Menon V, Sarnak MJ, Greene T, Wang X, Pereira AA, Beck GJ, et al. Relationship between homocysteine and mortality in chronic kidney disease. Circulation. 2006;113:1572–7.
Looker HC, Fagot-Campagna A, Gunter EW, Pfeiffer CM, Sievers ML, Bennett PH, et al. Homocysteine and vitamin B(12) concentrations and mortality rates in type 2 diabetes. Diabetes Metab Res Rev. 2007;23:193–201.
Li M, Zhan A, Huang X, Hu L, Zhou W, Wang T, et al. Positive association between triglyceride glucose index and arterial stiffness in hypertensive patients: the China H-type Hypertension Registry Study. Cardiovasc Diabetol. 2020;19:139.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18:137–50.
Li R, Chambless L. Test for additive interaction in proportional hazards models. Ann Epidemiol. 2007;17:227–36.
Xu B, Kong X, Xu R, Song Y, Liu L, Zhou Z, et al. Homocysteine and all-cause mortality in hypertensive adults without pre-existing cardiovascular conditions: Effect modification by MTHFR C677T polymorphism. Medicine. 2017;96:e5862.
Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998;338:1042–50.
Stuhlinger MC, Tsao PS, Her JH, Kimoto M, Balint RF, Cooke JP. Homocysteine impairs the nitric oxide synthase pathway: role of asymmetric dimethylarginine. Circulation. 2001;104:2569–75.
den Heijer T, Vermeer SE, Clarke R, Oudkerk M, Koudstaal PJ, Hofman A, et al. Homocysteine and brain atrophy on MRI of non-demented elderly. Brain. 2003;126:170–5.
Hasan T, Arora R, Bansal AK, Bhattacharya R, Sharma GS, Singh LR. Disturbed homocysteine metabolism is associated with cancer. Exp Mol Med. 2019;51:1–13.
Herrmann M, Peter Schmidt J, Umanskaya N, Wagner A, Taban-Shomal O, Widmann T, et al. The role of hyperhomocysteinemia as well as folate, vitamin B(6) and B(12) deficiencies in osteoporosis: a systematic review. Clin Chem Lab Med. 2007;45:1621–32.
Yang J, Hu X, Zhang Q, Cao H, Wang J, Liu B. Homocysteine level and risk of fracture: A meta-analysis and systematic review. Bone. 2012;51:376–82.
Zhao W, Gao F, Lv L, Chen X. The interaction of hypertension and homocysteine increases the risk of mortality among middle-aged and older population in the United States. J Hypertens. 2022;40:254–63.
Zhou F, Liu C, Ye L, Wang Y, Shao Y, Zhang G, et al. The Relative Contribution of Plasma Homocysteine Levels vs. Traditional Risk Factors to the First Stroke: A Nested Case-Control Study in Rural China. Front Med. 2021;8:727418.
Swart KM, van Schoor NM, Blom HJ, Smulders YM, Lips P. Homocysteine and the risk of nursing home admission and mortality in older persons. Eur J Clin Nutr. 2012;66:188–95.
Fan R, Zhang A, Zhong F. Association between Homocysteine Levels and All-cause Mortality: A Dose-Response Meta-Analysis of Prospective Studies. Sci Rep. 2017;7:4769.
Mendelsohn ME, Karas RH. Molecular and cellular basis of cardiovascular gender differences. Science. 2005;308:1583–7.
Yi F, Li PL. Mechanisms of homocysteine-induced glomerular injury and sclerosis. Am J Nephrol. 2008;28:254–64.
Fox CS, Gona P, Larson MG, Selhub J, Tofler G, Hwang SJ, et al. A multi-marker approach to predict incident CKD and microalbuminuria. J Am Soc Nephrol. 2010;21:2143–9.
Jardine MJ, Kang A, Zoungas S, Navaneethan SD, Ninomiya T, Nigwekar SU, et al. The effect of folic acid based homocysteine lowering on cardiovascular events in people with kidney disease: systematic review and meta-analysis. BMJ. 2012;344:e3533.
Xu X, Qin X, Li Y, Sun D, Wang J, Liang M, et al. Efficacy of Folic Acid Therapy on the Progression of Chronic Kidney Disease: The Renal Substudy of the China Stroke Primary Prevention Trial. JAMA Intern Med. 2016;176:1443–50.
Al-Aly Z, Zeringue A, Fu J, Rauchman MI, McDonald JR, El-Achkar TM, et al. Rate of kidney function decline associates with mortality. J Am Soc Nephrol. 2010;21:1961–9.
Midttun O, Theofylaktopoulou D, McCann A, Fanidi A, Muller DC, Meyer K, et al. Circulating concentrations of biomarkers and metabolites related to vitamin status, one-carbon and the kynurenine pathways in US, Nordic, Asian, and Australian populations. Am J Clin Nutr. 2017;105:1314–26.
Acknowledgements
Thank you to Dr. Xiping Xu from the Shenzhen Evergreen Medical Institute, who provided critical insights in the early stages of the work.
Funding
This study was supported by funding from the following: Cultivation of backup projects for National Science and Technology Awards (20223AEI91007), Jiangxi Science and Technology Innovation Base Plan - Jiangxi Clinical Medical Research Center (20223BCG74012), Science and Technology Innovation Base Construction Project (20221ZDG02010), Jiangxi Provincial Natural Science Foundation (20212ACB206019, 20224BAB206090, 20232BAB206140), Fund project of the Second Affiliated Hospital of Nanchang University (2021efyA01, 2022YNFY2017).
Author information
Authors and Affiliations
Contributions
CD: study concept and design, acquisition of data, data analysis, data interpretation, drafting of the manuscript, and revision of the manuscript for important intellectual content. JL, YW, WF, TC, ZC, YS, CY, TY, PZ, WZ, CY, TW and LZ: acquisition of data, critical review and revision of the manuscript for important intellectual content. XH, HB and XC: study concept and design, acquisition of data, data management, critical review and revision of the manuscript for important intellectual content.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ding, C., Li, J., Wei, Y. et al. Associations of total homocysteine and kidney function with all-cause and cause-specific mortality in hypertensive patients: a mediation and joint analysis. Hypertens Res 47, 1500–1511 (2024). https://doi.org/10.1038/s41440-024-01613-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01613-x
Keywords
This article is cited by
-
Mutual mediation effects of homocysteine and PCSK9 on coronary lesion severity in patients with acute coronary syndrome: interplay with inflammatory and lipid markers
Lipids in Health and Disease (2025)
-
Combined effect of hyperhomocysteinemia and mild-to-moderate chronic kidney disease on mortality and cardiovascular events in the Japanese general population: the Yamagata (Takahata) study
Clinical and Experimental Nephrology (2025)
-
Associations of physiologic subtypes based on HOMA2 indices of β-cell function and insulin sensitivity with the risk of kidney function decline, cardiovascular disease, and all-cause mortality from the 4C study
Cardiovascular Diabetology (2024)
-
Is renal function the key to disease risk management in elevated homocysteine levels?
Hypertension Research (2024)
-
Decoding the fatty liver-hyperuricemia link in the obese and nonobese hypertensive patients: insights from a cohort study
Scientific Reports (2024)