Abstract
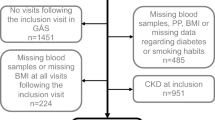
It remains unclear the age-specific associations of risk factors with deaths and mortality burden attributable across age. In a territory-wide retrospective cohort, 1,012,228 adults with hypertension were identified. Comorbidities including diabetes, chronic kidney disease (CKD), cardiovascular disease (CVD), heart failure, and cancer, and risk factors including current smoking and suboptimal control of blood pressure (BP), glucose and low-density lipoprotein cholesterol were defined. Associations of comorbidities/risk factors with all-cause and cause-specific mortality across age groups (18–54, 55–64, 65–74, and ≥75 years) were assessed. Population attributable fractions were also quantified. During a median follow-up of 10.7 years, 244,268 (24.1%) patients died, with pneumonia (7.2%), cancer (5.1%), and CVD (4.2%) being the leading causes. Despite increasing deaths with age, relative risk of mortality related to comorbidities/risk factors decreased with age; similar patterns were found for cause-specific mortality. The assessed risk factors accounted for 24.0% (95% CI 22.5%, 25.4%) deaths, with highest proportion in the youngest group (33.5% [28.1%, 38.5%] in 18–54 years vs 19.4% [17.0%, 21.6%] in ≥75 years). For mortality burden, CKD was the overall leading risk factor (12.7% [12.4%, 12.9%]) with higher proportions in older patients (11.1–13.1% in ≥65 years), while diabetes was the leading risk factor in younger patients (15.9–13.5% in 18–54 years). The association of comorbidities or risk factors with mortality is stronger in younger patients with hypertension, despite lower absolute mortality in young patients than in the elderly. Leading risk factors differed across age, highlighting the importance of targeted and precise risk management.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data will not be made available to others because the data custodians have not given permission. The syntax is available upon reasonable request.
References
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 Countries. Circulation. 2016;134:441–50.
Asayama K, Stolarz-Skrzypek K, Yang WY, Hansen TW, Brguljan-Hitij J, Odili AN, et al. What did we learn from the international databases on ambulatory and home blood pressure in relation to cardiovascular outcome? Hypertens Res. 2023;46:934–49.
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44.
Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44:398–404.
Wang JG, Zhang W, Li Y, Liu L. Hypertension in China: epidemiology and treatment initiatives. Nat Rev Cardiol. 2023;20:531–45.
Lauder L, Mahfoud F, Azizi M, Bhatt DL, Ewen S, Kario K, et al. Hypertension management in patients with cardiovascular comorbidities. Eur Heart J. 2023;44:2066–77.
Wang C, Yuan Y, Zheng M, Pan A, Wang M, Zhao M, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality. J Am Coll Cardiol. 2020;75:2921–30.
Lacey B, Lewington S, Clarke R, Kong XL, Chen Y, Guo Y, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Glob Health. 2018;6:e641–e9.
Collaboration PS. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Liu J, Zhao D, Liu J, Qi Y, Sun J, Wang W. Prevalence of diabetes mellitus in outpatients with essential hypertension in China: a cross-sectional study. BMJ Open. 2013;3:e003798.
Song J, Sheng CS, Huang QF, Li LH, Ma CS, Guo XH, et al. Management of hypertension and diabetes mellitus by cardiovascular and endocrine physicians: a China registry. J Hypertens. 2016;34:1648–53.
Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379:815–22.
Spiegelman D, Hertzmark E, Wand HC. Point and interval estimates of partial population attributable risks in cohort studies: examples and software. Cancer Causes Control. 2007;18:571–9.
Smith JR, Sharrett AR, Pike JR, Gottesman RF, Knopman DS, Lee M, et al. Dementia occurring over a 32-year follow-up attributable to hypertension observed at different ages: Implications for dementia prevention. Alzheimers Dement. 2023;19:3435–47.
Lee A. Seamless health care for chronic diseases in a dual health care system: managed care and the role of family physicians. J Manag Med. 1998;12:398–405, 322.
Yu EYT, Wan EYF, Mak IL, Chao DVK, Ko WWK, Leung M, et al. Assessment of hypertension complications and health service use 5 years after implementation of a multicomponent intervention. JAMA Netw Open. 2023;6:e2315064.
Wan EY, Fung CS, Yu EY, Fong DY, Chen JY, Lam CL. Association of visit-to-visit variability of systolic blood pressure with cardiovascular disease and mortality in primary care chinese patients with type 2 diabetes-A retrospective population-based cohort study. Diabetes Care. 2017;40:270–9.
Jin Q, Lau ESH, Luk AO, Tam CHT, Ozaki R, Lim CKP et al. Circulating metabolomic markers linking diabetic kidney disease and incident cardiovascular disease in type 2 diabetes: analyses from the Hong Kong Diabetes Biobank. Diabetologia. 2024. https://doi.org/10.1007/s00125-024-06108-5.
Jin Q, Kuen Lam CL, Fai Wan EY. Association of eGFR slope with all-cause mortality, macrovascular and microvascular outcomes in people with type 2 diabetes and early-stage chronic kidney disease. Diabetes Res Clin Pract. 2023;205:110924.
Jin Q, Luk AO, Lau ESH, Tam CHT, Ozaki R, Lim CKP, et al. Nonalbuminuric diabetic kidney disease and risk of all-cause mortality and cardiovascular and kidney outcomes in type 2 diabetes: findings from the hong kong diabetes biobank. Am J Kidney Dis. 2022;80:196–206.e1.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334–57.
6. Glycemic Targets: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45:S83–96.
Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37 Suppl 1:S81-90.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38:2459–72.
Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons; Hoboken, New Jersey; 2004.
Mahmoodi BK, Matsushita K, Woodward M, Blankestijn PJ, Cirillo M, Ohkubo T, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: a meta-analysis. Lancet. 2012;380:1649–61.
Hallan SI, Matsushita K, Sang Y, Mahmoodi BK, Black C, Ishani A, et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA. 2012;308:2349–60.
van Vark LC, Bertrand M, Akkerhuis KM, Brugts JJ, Fox K, Mourad JJ, et al. Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158,998 patients. Eur Heart J. 2012;33:2088–97.
Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–47.
Jacobs E, Hoyer A, Brinks R, Kuss O, Rathmann W. Burden of mortality attributable to diagnosed diabetes: a nationwide analysis based on claims data from 65 million people in Germany. Diabetes Care. 2017;40:1703–9.
Sugiyama D, Okamura T, Watanabe M, Higashiyama A, Okuda N, Nakamura Y, et al. Risk of hypercholesterolemia for cardiovascular disease and the population attributable fraction in a 24-year Japanese cohort study. J Atheroscler Thromb. 2015;22:95–107.
Gu D, Kelly TN, Wu X, Chen J, Samet JM, Huang J-f, et al. Mortality attributable to smoking in China. N. Engl J Med. 2009;360:150–9.
Ghazi L, Oparil S, Calhoun DA, Lin CP, Dudenbostel T. Distinctive risk factors and phenotype of younger patients with resistant hypertension: age is relevant. Hypertension. 2017;69:827–35.
Aguilar D. Preventing Heart Failure in People With Hypertension: The Time Is Now. JACC Heart Fail. 2023;11:689–90.
Maeda D, Dotare T, Matsue Y, Teramoto K, Sunayama T, Tromp J, et al. Blood pressure in heart failure management and prevention. Hypertens Res 2023;46:817–33.
Anker SD, Usman MS, Butler J SGLT2 inhibitors: from antihyperglycemic agents to all-around heart failure therapy. In. Vol 146. Am Heart Assoc2022, 299-302.
Kjeldsen SE, Stenehjem A, Os I, Van de Borne P, Burnier M, Narkiewicz K, et al. Treatment of high blood pressure in elderly and octogenarians: European Society of Hypertension statement on blood pressure targets. Blood Press. 2016;25:333–6.
Boshuizen HC, Izaks GJ, van Buuren S, Ligthart GJ. Blood pressure and mortality in elderly people aged 85 and older: community based study. BMJ. 1998;316:1780–4.
Daw J. Contribution of four comorbid conditions to racial/ethnic disparities in mortality risk. Am J Prevent Med. 2017;52:S95–S102.
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49.
Acknowledgements
The authors thank the Statistics and Workforce Planning Department at the Hong Kong Hospital Authority for data extraction.
Funding
This study is supported by the start-up fund from the University of Hong Kong. No funding organization had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Study design and conception: QJ, EYFW; data acquisition: QJ, JM; statistical analysis: QJ, JM; data interpretation: QJ, EYFW; manuscript draft: QJ, EYFW; critical revision: QJ, CLKL, EYFW; funding acquisition: CLKL, EYFW; supervision or mentorship: EYFW. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
EYFW has received research grants from the Health Bureau, the Hong Kong Research Grant Council, the Narcotics Division of Security Bureau of the Government of the Hong Kong SAR, and National Natural Science Foundation of China outside the submitted work. CLKL has received research grants from the Health Bureau of the Government of the Hong Kong SAR, the Hong Kong Research Grant Council, the Hong Kong College of Family Physicians, and Kerry Group Kuok Foundation outside the submitted work.
Ethical approval
This study was approved by the Institutional Review Board of The University of Hong Kong (UW 19-329). As all data used in this study have been anonymized and retrieved from the Clinical Management System of the Hong Kong Hospital Authority, no consent to participate from the patient was required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jin, Q., Mei, J., Wong, Y.C. et al. Associations and attributable burden between risk factors and all-cause and cause-specific mortality at different ages in patients with hypertension. Hypertens Res 47, 2053–2063 (2024). https://doi.org/10.1038/s41440-024-01717-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01717-4
Keywords
This article is cited by
-
Efficacy and safety of esaxerenone in hypertensive patients with chronic kidney disease, with or without type 2 diabetes mellitus: a pooled analysis of five clinical studies
Hypertension Research (2025)
-
Early onset of hypertension and increased relative risks of chronic kidney disease and mortality: two population-based cohort studies in United Kingdom and Hong Kong
Hypertension Research (2025)
-
Protecting young and middle-aged adults from a high risk of mortality owing to various risk factors
Hypertension Research (2024)
-
Hypertension in Asia: Genetic, lifestyle, and clinical insights
Hypertension Research (2024)