Abstract
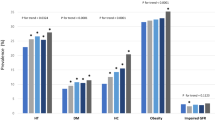
Adherence to lifestyle recommendations is crucial in managing hypertension, independent of medical treatment. This study aimed to evaluate the implementation of adherence to lifestyle recommendations and analyze the trends in adherence to lifestyle recommendations among patients with hypertension in Korea from 2007 to 2021 using the Korea National Health and Nutrition Examination Survey (KNHANES). The study included adults aged ≥20 years. Factors such as regular physical activity, smoking and alcohol abstinence, weight and stress management, and adherence to a healthy diet were analyzed. In 2021, A doublefold increase was observed in the proportion of patients with hypertension who adhered to sodium restriction compared to 2007. However, 70% of patients with hypertension consume more sodium than recommended. Moreover, potassium intake has steadily decreased since 2014, with only 23.8% of patients with hypertension meeting the recommended intake. The body mass index (BMI) and waist circumference of patients with hypertension have gradually increased, with fewer patients maintaining an appropriate weight. The neglect of diet and weight control among young patients with hypertension who experience high stress levels poses challenges in modifying their lifestyles. Patients with hypertension in Korea still consume high amounts of sodium, whereas potassium intake is gradually decreasing. Additionally, obesity rates have been increasing, especially among young patients with hypertension. A multidisciplinary approach is necessary for improving the lifestyle habits of hypertensive patients.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Collaborators GBDRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–94.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart Disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation 2018;137:e67–492.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–82.
Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606.
Kang SH, Kim SH, Cho JH, Yoon CH, Hwang SS, Lee HY, et al. Prevalence, awareness, treatment, and control of hypertension in Korea. Sci Rep. 2019;9:10970.
Neuhauser HK, Adler C, Rosario AS, Diederichs C, Ellert U. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008-11. J Hum Hypertens. 2015;29:247–53.
Roy A, Praveen PA, Amarchand R, Ramakrishnan L, Gupta R, Kondal D, et al. Changes in hypertension prevalence, awareness, treatment and control rates over 20 years in National Capital Region of India: results from a repeat cross-sectional study. BMJ Open. 2017;7:e015639.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 2020;141:e139–596.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–57.
Kim HL, Lee EM, Ahn SY, Kim KI, Kim HC, Kim JH, et al. The 2022 focused update of the 2018 Korean Hypertension Society Guidelines for the management of hypertension. Clin Hypertens. 2023;29:11.
Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014;43:69–77.
Lee HH, Cho SMJ, Lee H, Baek J, Bae JH, Chung WJ, et al. Korea Heart Disease Fact Sheet 2020: analysis of nationwide data. Korean Circ J. 2021;51:495–503.
Jackson SL, Park S, Loustalot F, Thompson-Paul AM, Hong Y, Ritchey MD. Characteristics of US adults who would be recommended for lifestyle modification without antihypertensive medication to manage blood pressure. Am J Hypertens. 2021;34:348–58.
Donfrancesco C, Buttari B, Marcozzi B, Sieri S, Di Lonardo A, Lo Noce C, et al. Nutrition, physical activity and smoking habit in the Italian general adult population: CUORE Project Health Examination Survey 2018-2019. Healthcare. 2024;12:475.
Akbarpour S, Khalili D, Zeraati H, Mansournia MA, Ramezankhani A, Fotouhi A. Healthy lifestyle behaviors and control of hypertension among adult hypertensive patients. Sci Rep. 2018;8:8508.
Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315.
Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2015;33:1509–20.
Graudal N, Hubeck-Graudal T, Jurgens G, Taylor RS. Dose-response relation between dietary sodium and blood pressure: a meta-regression analysis of 133 randomized controlled trials. Am J Clin Nutr. 2019;109:1273–8.
Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:CD004022.
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378.
Park HK, Lee Y, Kang BW, Kwon KI, Kim JW, Kwon OS, et al. Progress on sodium reduction in South Korea. BMJ Glob Health. 2020;5:e002028.
He FJ, Brinsden HC, MacGregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens. 2014;28:345–52.
Alonso S, Tan M, Wang C, Kent S, Cobiac L, MacGregor GA, et al. Impact of the 2003 to 2018 population salt intake reduction program in England: a modeling study. Hypertension. 2021;77:1086–94.
Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006;49:59–75.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Valenzuela PL, Carrera-Bastos P, Galvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM, et al. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol. 2021;18:251–75.
Blumenthal JA, Sherwood A, Gullette EC, Babyak M, Waugh R, Georgiades A, et al. Exercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioning. Arch Intern Med. 2000;160:1947–58.
Okamura T, Tanaka T, Babazono A, Yoshita K, Chiba N, Takebayashi T, et al. The high-risk and population strategy for occupational health promotion (HIPOP-OHP) study: study design and cardiovascular risk factors at the baseline survey. J Hum Hypertens. 2004;18:475–85.
Tamaki J, Kikuchi Y, Yoshita K, Takebayashi T, Chiba N, Tanaka T, et al. Stages of change for salt intake and urinary salt excretion: baseline results from the High-Risk and Population Strategy for Occupational Health Promotion (HIPOP-OHP) study. Hypertens Res. 2004;27:157–66.
Nomura S, Sakamoto H, Ghaznavi C, Inoue M. Toward a third term of Health Japan 21—implications from the rise in non-communicable disease burden and highly preventable risk factors. Lancet Reg Health West Pac. 2022;21:100377.
Dye CJ, Williams JE, Evatt JH. Improving hypertension self-management with community health coaches. Health Promot Pr. 2015;16:271–81.
Villinger K, Wahl DR, Boeing H, Schupp HT, Renner B. The effectiveness of app-based mobile interventions on nutrition behaviours and nutrition-related health outcomes: a systematic review and meta-analysis. Obes Rev. 2019;20:1465–84.
Thomas JG, Bond DS, Raynor HA, Papandonatos GD, Wing RR. Comparison of smartphone-based behavioral obesity treatment with gold standard group treatment and control: a randomized trial. Obesity. 2019;27:572–80.
Kario K, Nomura A, Harada N, Okura A, Nakagawa K, Tanigawa T, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021. https://doi.org/10.1093/eurheartj/ehab559.
Islam FMA, Lambert EA, Islam SMS, Islam MA, Biswas D, McDonald R, et al. Lowering blood pressure by changing lifestyle through a motivational education program: a cluster randomized controlled trial study protocol. Trials. 2021;22:438.
Taher M, Yule C, Bonaparte H, Kwiecien S, Collins C, Naylor A, et al. Telehealth versus self-directed lifestyle intervention to promote healthy blood pressure: a protocol for a randomised controlled trial. BMJ Open. 2021;11:e044292.
Bolmsjo BB, Wolff M, Nymberg VM, Sandberg M, Midlov P, Calling S. Text message-based lifestyle intervention in primary care patients with hypertension: a randomized controlled pilot trial. Scand J Prim Health Care. 2020;38:300–7.
Funding
This research was supported by the 2021 Chung-Ang University research grant. The content is solely the responsibility of the authors and does not necessarily represent the official view of any funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, J.H., Park, G.T., Park, KT. et al. Temporal trends in adherence to lifestyle recommendations of patients with hypertension in Korea, 2007–2021. Hypertens Res 48, 157–167 (2025). https://doi.org/10.1038/s41440-024-01838-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01838-w