Abstract
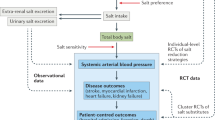
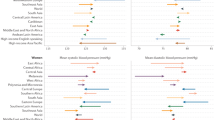
The association between high salt intake and elevated blood pressure levels has been well-documented. However, studies on how effectively this knowledge translates into actionable practices, particularly across different ethnic groups, remain limited. This study aimed to evaluate the knowledge, attitudes, and practices (KAP) towards dietary salt intake across ethnicities and determine its association with hypertension. 5128 Malaysian adults recruited from a national blood pressure screening study completed questionnaires on demographics, and KAP related to dietary salt intake. There were 57.4% Malay, 23.5% Chinese, 10.4% Indian, and 8.7% individuals of other ethnic groups. Overall, more than 90% of the participants knew that a high salt intake causes serious health problems, but only around one-third knew the relationship between high salt intake and strokes and heart failure. Participants of different ethnic groups displayed significant differences in the KAP domains, where Indians generally exhibited better knowledge, attitudes, and reported better practices such as reading salt labels and using spices. Those who were unaware of the difference between salt and sodium and who reported not reading salt labels had higher odds of having elevated blood pressure. These findings demonstrate that while there is a suboptimal translation of salt knowledge into practice in Malaysia, with significant differences in KAP observed between ethnic groups, the potential of improving health outcomes by improving the clarity and awareness of salt labels is substantial. Tailored education promoting salt-label reading, minimizing processed foods intake and discretionary salt use should be ethnic-specific to better curb this escalating hypertension epidemic.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, YCC, upon reasonable request.
References
Soo MJ, Chow ZY, Ching SM, Tan CH, Lee KW, Devaraj NK, et al. Prevalence, awareness and control of hypertension in Malaysia from 1980-2018: a systematic review and meta-analysis. World J Meta-Anal. 2020;8:320–44.
MOH. National Health and Morbidity Survey 2019 Non-communicable diseases, healthcare demand, and health literacy. Retrieved on 6 Feb 2024 from chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/ https://iptk.moh.gov.my/images/technical_report/2020/4_Infographic_Booklet_NHMS_2019_-_English.pdf.
Wang K, Jin Y, Wang M, Liu J, Bu X, Mu J, et al. Global cardiovascular diseases burden attributable to high sodium intake from 1990 to 2019. J Clin Hypertens. 2023;25:868–79.
Messerli FH, Hofstetter L, Syrogiannouli L, Rexhaj E, Siontis GCM, Seiler C, et al. Sodium intake, life expectancy, and all-cause mortality. Eur Heart J. 2021;42:2103–12.
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733.
Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38:791–813.
Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–34.
Shao S, Hua Y, Yang Y, Liu X, Fan J, Zhang A, et al. Salt reduction in China: a state-of-the-art review. Risk Manag Health Policy. 2017;10:17–28.
WHO. Salt reduction. Retrieved on 6 February 2024 from https://www.who.int/news-room/fact-sheets/detail/salt-reduction#:~:text=The%20global%20mean%20intake%20of,5%20g%2Fday%20salt) 2023).
Institute for Public Health (IPH). Population-Based Salt Intake Survey To Support The National Salt Reduction Programme For Malaysia (Malaysian Community Salt Survey – MyCoSS). Retrieved on 6 February 2024 from chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/ https://iku.gov.my/images/IKU/Document/SALT-FULL_Report.pdf.
Lu X, Crowley SD. Inflammation in salt-sensitive hypertension and renal damage. Curr Hypertens Rep. 2018;20:103.
Elijovich F, Weinberger MH, Anderson CAM, Appel LJ, Bursztyn M, Cook NR, et al. Salt Sensitivity of Blood Pressure: A Scientific Statement From the American Heart Association. Hypertension. 2016;68:e7–46.
Graudal N, Hubeck-Graudal T, Jürgens G, Taylor RS. Dose-response relation between dietary sodium and blood pressure: a meta-regression analysis of 133 randomized controlled trials. Am J Clin Nutr. 2019;109:1273–8.
Jaques DA, Wuerzner G, Ponte B. Sodium intake as a cardiovascular risk factor: a narrative review. Nutrients. 2021;13:3177.
Bailey MA, Dhaun N. Salt sensitivity: causes, consequences, and recent advances. Hypertension. 2024;81:476–89.
Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM, et al. 2021 Dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2021;144:e472–87.
Trieu K, Neal B, Hawkes C, Dunford E, Campbell N, Rodriguez-Fernandez R, et al. Salt reduction initiatives around the world - a systematic review of progress towards the global target. PLoS ONE. 2015;10:e0130247.
Ni Mhurchu C, Capelin C, Dunford EK, Webster JL, Neal BC, Jebb SA. Sodium content of processed foods in the United Kingdom: analysis of 44,000 foods purchased by 21,000 households. Am J Clin Nutr. 2011;93:594–600.
Charchar FJ, Prestes PR, Mills C, Ching SM, Neupane D, Marques FZ, et al. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2024;42:23–49.
Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62:18–26.
CodeBlue. Report: 41% Of Malaysia’s Adults Will Be Obese By 2035 retrieved by 6 February 2024 from https://codeblue.galencentre.org/2023/03/03/report-41-of-malaysias-adults-will-be-obese-by-2035/.
Ahmad MH, Man CS, Othman F, He FJ, Salleh R, Noor NSM, et al. High sodium food consumption pattern among Malaysian population. J Health Popul Nutr. 2021;40 Suppl 1:4.
Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, et al. May measurement month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J. 2019;40:2006–17.
British and Irish Hypertension Society. Validated BP monitors for home use. https://bihsoc.org/wp-content/uploads/2023/12/Validated-BP-Monitors-For-Home-Use-British-and-Irish-Hypertension-Society-1.pdf. Accessed 11 January 2021.
WHO. WHO/PAHO Regional Expert Group for Cardiovascular Disease Prevention through Population wide Dietary Salt Reduction: protocol for population level sodium determination in 24 h urine samples. Geneva, Switzerland: World Health Organization; 2010. https://www3.paho.org/hq/dmdocuments/2013/Final-Report-Regional-Expert-Group-Nov-2011-Eng.pdf. Accessed 6 Feb 2024.
WHO. Physical status: the use of and interpretation of anthropometry, Report of a WHO Expert Committee. World Health Organization; 1995.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Sairenchi T, Iso H, Irie F, Fukasawa N, Yamagishi K, Kanashiki M, et al. Age-specific relationship between blood pressure and the risk of total and cardiovascular mortality in Japanese men and women. Hypertens Res. 2005;28:901–9.
Tran D-MT, Zimmerman LM. Cardiovascular risk factors in young adults: a literature review. J Cardiovasc Nurs. 2015;30:298–310.
Lewington S, Clarke R, Qizilbash N. Prospective studies collaboration age-specific relevance of usual BP to vascular mortality: ameta-analysis of individual data for one million adults in 61 prospective studies published erratum appears. Lancet. 2003;361:1903–13.
Chan CMJ, Dickens BSL, Chong MF-F. Understanding knowledge, attitudes and behaviours related to dietary sodium intake in a multi-ethnic population in Singapore. Public Health Nutr. 2023;26:2802–14.
Johnson C, Mohan S, Rogers K, Shivashankar R, Thout SR, Gupta P, et al. The association of knowledge and behaviours related to salt with 24-h urinary salt excretion in a population from North and South India. Nutrients. 2017;9:144.
Aparna P, Salve HR, Anand K, Ramakrishnan L, Gupta SK, Nongkynrih B. Knowledge and behaviors related to dietary salt and sources of dietary sodium in North India. J Fam Med Prim Care. 2019;8:846–52.
Ahmad NHN, Taha CSC, Harith SJAjom, biomedicine. Sodium intake and its association with knowledge, attitudes and practices among health sciences students in Universiti Sultan Zainal Abidin (Unisza). Asian J Med Biomed. 2020;4(SI1):91–103.
Ismail M, Regu T, Jimponey MJ, Michael V, Mohamed FN, Hussin R, et al. Knowledge, attitude and practice towards salt intake and health among non-academic staff of Universiti Kebangsaan Malaysia: a pilot study. Life Sci Med Biomed. 2021;5:1–8.
Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. J Hypertens. 2011;29:1043–50.
Campbell NR, Johnson JA, Campbell TS. Sodium consumption: an individual’s choice? Int J Hypertens. 2012;2012:860954.
Hyseni L, Elliot-Green A, Lloyd-Williams F, Kypridemos C, O’Flaherty M, McGill R, et al. Systematic review of dietary salt reduction policies: evidence for an effectiveness hierarchy? PLoS ONE. 2017;12:e0177535.
House J, Brons A, Wertheim-Heck S, van der Horst H. What is culturally appropriate food consumption? A systematic literature review exploring six conceptual themes and their implications for sustainable food system transformation. Agric Human Values. 2023. https://doi.org/10.1007/s10460-023-10515-6.
Zaki NAM, Ambak R, Othman F, Wong NI, Man CS, Morad MFA, et al. The prevalence of hypertension among Malaysian adults and its associated risk factors: data from Malaysian Community Salt Study (MyCoSS). J Health Popul Nutr. 2021;40 Suppl 1:8.
Song Y, Ma W, Yi X, Wang S, Sun X, Tian J, et al. Chronic diseases knowledge and related factors among the elderly in Jinan, China. PLoS ONE. 2013;8:e68599.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325.
Ministry of Economy, Department of Statistics Malaysia Official Portal. https://www.dosm.gov.my/portal-main/release-content/8c705dac-ef05-11ed-96d5-1866daa77ef9 (accessed 22 May 23).
Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 h urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988;297:319–28.
Stamler J, Chan Q, Daviglus ML, Dyer AR, Van Horn L, Garside DB, et al. Relation of dietary sodium (salt) to blood pressure and its possible modulation by other dietary factors: the INTERMAP study. Hypertension. 2018;71:631–7.
Kario K, Wang J-G. Could 130/80 mm Hg be adopted as the diagnostic threshold and management goal of hypertension in consideration of the characteristics of Asian populations? Hypertension. 2018;71:979–84.
Acknowledgements
We would like to thank the MMM 2018 at the International Society of Hypertension (ISH), Malaysian Society of Hypertension (MSH), Malaysian Society of Hypertension-Sunway University Young Investigator Network (MSH-SU YIN), and the Malaysian Society for World Action on Salt, Sugar and Health (MyWASSH) for their support in this study. We would also like to thank the following individuals who contributed to the data collection activities for MMM 2018, Abdul Hafiz Mohamad Gani, Dalyana Hamid, Tay Chai Li, Wong Ping Foo, Haslinda Hassan, Noor Marzlin Marzukhi, Kong Sie Zin, Sunita Bavanandan, Nadratulmazlyna Mansor, Ng Wei Leik, Christine Shamla Selvaraj, Ahmad Fithri Azam Abdul Rahman, Hanisah Shafie, Dr Zeti, Ding Ai Lee, Syariza Radzi, Hanis Saadah Husin, Azli Shahril Othman, Pei San Kang.
Author information
Authors and Affiliations
Contributions
YCC conceived and devised the concept of examining the KAP of salt intake in this sub-study. YCC, SMC, NKD, PBO, and MTC developed the KAP questionnaire on salt. All other authors contributed to data collection. YCC, NKD, JEKO, SMC, FCFL, MTC analysed the data. YCC SMC and MTC wrote the manuscript. All other authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was obtained from the Malaysian National Medical Research Register (NMRR-18-876-40691) and Universiti Malaya Medical Center (MREC ID NO: 2018320-6146).
Conflict of interest
YCC received on behalf of the Malaysian Society on Salt, Sugar and Health (MyWASSH), an unrestricted educational grant from Medtronic.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chia, Y.C., Ching, S.M., Chew, M.T. et al. Ethnic differences in knowledge, attitudes, and practices related to dietary salt intake and association with hypertension in Malaysia: a multi-centre cross-sectional study. Hypertens Res 48, 131–147 (2025). https://doi.org/10.1038/s41440-024-01851-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01851-z