Abstract
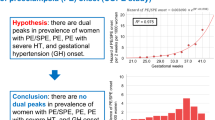
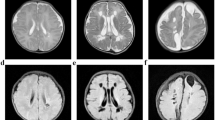
Our aim was to evaluate the effects of any types of hypertensive disorders of pregnancy (HDP) on the development of either cerebral palsy (CP) or developmental delay (DD) at 3 years old in singleton very low-birth-weight (VLBW) infants born at 24–31 weeks of gestation. This was a retrospective cohort study of VLBW infants born at 24–31 weeks in 2013–2016 in Japan, using a nationwide obstetrical database, and Neonatal Research Network Japan (NRNJ) Database, accompanied by a secondary survey of women complicated with HDP (EOPE-DQ study). In 529 candidates for long-term follow-up in 7 tertiary centers, the percentage undergoing follow-up for CP at 3 years old was 56.1%, and the percentage receiving follow-up for DD at 3 years old was 54.1%. The percentage of PE/SPE/GH was significantly lower in infants with CP than in controls (1/22 [4.5%] vs. 66/274 [24.1%], p = 0.034); especially, in infants born at 28–31 weeks, the percentage of PE/SPE/GH was significantly lower in infants with CP than in controls (0/13 [0%] vs. 44/151 [29.1%], p = 0.021). The percentage of PE/SPE/GH was not different between infants with DD and controls (9/49 [18.4%] vs. 54/237 [22.8%], p = 0.574). The percentage of composite risk factors (either bronchopulmonary dysplasia at a postmenstrual age of 36 weeks, intraventricular hemorrhage, hypoxic ischemic encephalopathy, sepsis, necrotizing enterocolitis, or periventricular leukomalacia) was significantly higher in infants with DD than in controls. In conclusion, PE/SPE/GH around 30 weeks may be associated with a low incidence of CP.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Schroers JE, Shanmugalingam R, Lee G, Rutherford D, Makris A. Prevalence of long term metabolic, cardiovascular, cerebrovascular and renal disease in patients with hypertensive disorders in pregnancy remote from pregnancy (POMCH). Pregnancy Hypertens. 2022;28:162–7.
Bokuda K, Ichihara A. Preeclampsia up to date-What’s going on? Hypertens Res. 2023;46:1900–7.
An H, Jin M, Li Z, Zhang L, Li H, Zhang Y, et al. Impact of gestational hypertension and pre-eclampsia on preterm birth in China: a large prospective cohort study. BMJ Open. 2022;12:e058068.
Nakamura N, Ushida T, Nakatochi M, Kobayashi Y, Moriyama Y, Imai K, et al. Mortality and neurological outcomes in extremely and very preterm infants born to mothers with hypertensive disorders of pregnancy. Sci Rep. 2021;11:1729.
Koulouraki S, Paschos V, Pervanidou P, Christopoulos P, Gerede A, Eleftheriades M. Short- and Long-Term Outcomes of Preeclampsia in Offspring: Review of the Literature. Child (Basel). 2023;10:826.
Korzeniewski SJ, Sutton E, Escudero C, Roberts JM. The Global Pregnancy Collaboration (CoLab) symposium on short- and long-term outcomes in offspring whose mothers had preeclampsia: A scoping review of clinical evidence. Front Med (Lausanne). 2022;9:984291.
Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359:262–73.
Chen D, Huang M, Yin Y, Gui D, Gu Y, Zhuang T, et al. Risk factors of cerebral palsy in children: a systematic review and meta-analysis. Transl Pediatr. 2022;11:556–64.
Strand KM, Heimstad R, Iversen AC, Austgulen R, Lydersen S, Andersen GL, et al. Mediators of the association between pre-eclampsia and cerebral palsy: population based cohort study. BMJ. 2013;347:f4089.
Blair E, Watson L, Australian Cerebral Palsy Register Group. Cerebral palsy and perinatal mortality after pregnancy-induced hypertension across the gestational age spectrum: observations of a reconstructed total population cohort. Dev Med Child Neurol. 2016;58:76–81.
Yoneda N, Yoneda S, Tsuda S, Ito M, Shiozaki A, Niimi H, et al. Pre-eclampsia Complicated With Maternal Renal Dysfunction Is Associated With Poor Neurological Development at 3 Years Old in Children Born Before 34 Weeks of Gestation. Front Pediatr. 2021;9:624323.
Kono Y, Yonemoto N, Nakanishi H, Hosono S, Hirano S, Kusuda S, et al. A Retrospective Cohort Study on Mortality and Neurodevelopmental Outcomes of Preterm Very Low Birth Weight Infants Born to Mothers with Hypertensive Disorders of Pregnancy. Am J Perinatol. 2022;39:1465–77.
Chang HY, Chen CP, Sun FJ, Chen CY. Influence of pre-eclampsia on 2-year neurodevelopmental outcome of very-low-birth-weight infants. Int J Gynaecol Obstet. 2023;161:979–88.
Szymonowicz W, Yu VY. Severe pre-eclampsia and infants of very low birth weight. Arch Dis Child. 1987;62:712–6.
Spinillo A, Iasci A, Capuzzo E, Egbe TO, Colonna L, Fazzi E. Two-year infant neurodevelopmental outcome after expectant management and indicated preterm delivery in hypertensive pregnancies. Acta Obstet Gynecol Scand. 1994;73:625–9.
Cheng SW, Chou HC, Tsou KI, Fang LJ, Tsao PN. Delivery before 32 weeks of gestation for maternal pre-eclampsia: neonatal outcome and 2-year developmental outcome. Early Hum Dev. 2004;76:39–46.
Spinillo A, Montanari L, Gardella B, Roccio M, Stronati M, Fazzi E. Infant sex, obstetric risk factors, and 2-year neurodevelopmental outcome among preterm infants. Dev Med Child Neurol. 2009;51:518–25.
Mann JR, McDermott S, Griffith MI, Hardin J, Gregg A. Uncovering the complex relationship between pre-eclampsia, preterm birth and cerebral palsy. Paediatr Perinat Epidemiol. 2011;25:100–10.
Mor O, Stavsky M, Yitshak-Sade M, Mastrolia SA, Beer-Weisel R, Rafaeli-Yehudai T, et al. Early onset preeclampsia and cerebral palsy: a double hit model? Am J Obstet Gynecol. 2016;214:105.e1–9.
Masuzaki H, Takeda S, Ikeda T, Kimura T, Kudo Y, Kubo T, et al. Houkoku: Syuusanki iinkai [Annual Report: Perinatal Medicine Committee] [in Japanese]. Acta Obstet Gynaecol Jpn. 2015;67:1517–66.
Takeda S, Kanayama N, Itakura A, Ito H, Unno N, Kikuchi A, et al. Houkoku: Syuusanki iinkai [Annual Report: Perinatal Medicine Committee] [in Japanese]. Acta Obstet Gynaecol Jpn. 2016;68:1381–403.
Takeda S, Kanayama N, Itakura A, Ito H, Unno N, Kikuchi A, et al. Houkoku: Syuusanki iinkai [Annual Report: Perinatal Medicine Committee] [in Japanese]. Acta Obstet Gynaecol Jpn. 2017;69:1445–79.
Kanayama N, Ikeda T, Itakura A, Ito H, Unno N, Sameshima H, et al. Houkoku: Syuusanki iinkai [Annual Report: Perinatal Medicine Co; mmittee] [in Japanese]. Acta Obstet Gynaecol Jpn. 2018;70:1504–37.
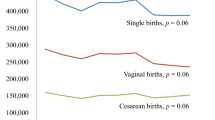
Ohkuchi A, Suzuki H, Matsubara K, Watanabe K, Saitou T, Oda H, et al. Exponential increase of the gestational-age-specific incidence of PE onset (COPE study): a multicenter retrospective cohort study in women with maternal check-ups at <20 weeks of gestation in Japan. Hypertens Res. 2022;45:1679–89.
Neonatal Research Network Database Japan. Accessed January 10, 2024 at: http://plaza.umin.ac.jp/nrndata/indexe.htm
Network Database Operation Manual Ver6.3 (Year 2017). Accessed January 10, 2023 at: http://plaza.umin.ac.jp/nrndata/pdf/manual2.pdf.
Blanc WA. Pathology of the placenta, membranes, and umbilical cord in bacterial, fungal, and viral infections inman. Monogr Pathol. 1981;22:67–132.
Itabashi K, Fujimura M, Kusuda S, Tamura M, Hayashi T, Takahashi T, et al. Atarashii zaitai kikan betsu shussei ji taikaku hyoujun ti no dounyuu ni tsuite [Introduction of new gestational age-specific standards for birth size] [in Japanese]. Acta Paediatrica Japonica. 2010;114:1271–93.
Watanabe K, Matsubara K, Nakamoto O, Ushijima J, Ohkuchi A, Koide K, et al. Outline of the new definition and classification of “Hypertensive Disorders of Pregnancy (HDP)”; a revised JSSHP statement of 2005. Hypertens Res Pregnancy. 2018;6:33–7.
Watanabe K, Naruse K, Tanaka K, Metoki H, Suzuki Y. Outline of definition and classification of “Pregnancy induced hypertension(PIH)”. Hypertens Res Pregnancy. 2013;1:3–4.
Satoh K ‘Atarashii “Ninshin Tyuudokushou” no teigi bunrui shian (2004)’ no Nihoh Sannka Fujinka Gakkai heno Teian Keika (Proposal process to Japan Society of Obstetrics and Gynecology for ‘New definition and classification idea of TOXEMIA OF PREGNANCY’). In Japan Society for the Study of TOXEMIA OF PREGNANCY (ed), Historical Perspective of Study of Pregnancy-Induced Hypertension in Japan. MEDICAL VIEW: Tokyo, Japan, 2015, pp. 76–81.
Ishii N, Kono Y, Yonemoto N, Kusuda S, Fujimura M. Neonatal Research Network, Japan. Outcomes of infants born at 22 and 23 weeks’ gestation. Pediatrics. 2013;132:62–71.
Bax MC. Terminology and classification of cerebral palsy. Dev Med Child Neurol. 1964;6:295–7.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Society for the Kyoto Scale of Psychological Development Test (ed). Shinban K Shiki Hattatsu Kensahou, 2001 Nenban) [the Kyoto Scale of Psychological Development Test 2001] [in Japanese]. Nakanishiya Shuppan; Kyoto, Japan, 2008.
The Japan Neonatal Follow-up Study Group. Protocol for the multicenter follow-up study of VLBW infants (in Japanese). Accessed January 10, 2020 at: http://highrisk-followup.jp/schedule/
Kono Y, Yonemoto N, Kusuda S, Hirano S, Iwata O, Tanaka K, et al. Developmental assessment of VLBW infants at 18 months of age: a comparison study between KSPD and Bayley III. Brain Dev. 2016;38:377–85.
Trønnes H, Wilcox AJ, Lie RT, Markestad T, Moster D. Risk of cerebral palsy in relation to pregnancy disorders and preterm birth: a national cohort study. Dev Med Child Neurol. 2014;56:779–85.
Tsamantioti E, Lisonkova S, Muraca G, Örtqvist AK, Razaz N. Chorioamnionitis and risk of long-term neurodevelopmental disorders in offspring: a population-based cohort study. Am J Obstet Gynecol. 2022;227:287.e1–7.
Resch B, Resch E, Maurer-Fellbaum U, Pichler-Stachl E, Riccabona M, Hofer N, et al. The whole spectrum of cystic periventricular leukomalacia of the preterm infant: results from a large consecutive case series. Childs Nerv Syst. 2015;31:1527–32.
Yoon BH, Romero R, Park JS, Kim CJ, Kim SH, Choi JH, et al. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am J Obstet Gynecol. 2000;182:675–81.
Twilhaar ES, Wade RM, de Kieviet JF, van Goudoever JB, van Elburg RM, Oosterlaan J. Cognitive Outcomes of Children Born Extremely or Very Preterm Since the 1990s and Associated Risk Factors: A Meta-analysis and Meta-regression. JAMA Pediatr. 2018;172:361–7.
Acknowledgements
The authors did not receive any funding relevant to this article to disclose. However, this study was supported by JSSHP. The supporting society had no role in the design or conduct of the study. The authors would like to thank all participating institutions and patients involved in the study for their valuable contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohkuchi, A., Suzuki, H., Kanai, A. et al. Early-onset preeclampsia/gestational hypertension may be associated with a low incidence of cerebral palsy at 3 years old in singleton very low-birth-weight infants born at 28–31 weeks of gestation (EOPE-DQ study): a multi-center retrospective cohort study in 2013–2016. Hypertens Res 48, 88–101 (2025). https://doi.org/10.1038/s41440-024-01929-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01929-8
Keywords
This article is cited by
-
Interpretable machine learning model for predicting low birth weight in singleton pregnancies: a retrospective cohort study
BMC Pregnancy and Childbirth (2025)
-
Approaching the paradoxical relationship between hypertensive disorders of pregnancy and cerebral palsy among infants born very preterm with very low birth weight
Hypertension Research (2025)