Abstract
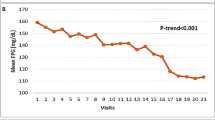
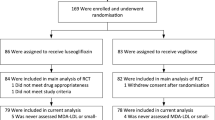
Sleep apnea (SA) is prevalent among patients with heart failure (HF) and contributes to a poor prognosis. Sodium–glucose cotransporter 2 (SGLT2) inhibitors have demonstrated efficacy in reducing the risk of serious clinical events in patients with HF. Additionally, SGLT2 inhibitors may reduce the risk of incident SA and mitigate its severity in patients with cardiovascular disease and T2DM. We aimed to investigate whether the SGLT2 inhibitor tofogliflozin reduced the severity of SA, as assessed using the apnea–hypopnea index (AHI), in patients with HF and T2DM and whether a decrease in AHI correlates with changes in body composition and cardiorenal function parameters. This is a single-arm, prospective pathophysiologic study involving patients with HF, T2DM, and SA, defined as having an AHI of 15 events/h and more. SA was assessed using polysomnography. Changes in AHI before and 6 months after starting oral administration of tofogliflozin (20 mg) were assessed. Additionally, body composition and cardiorenal functions were assessed before and 6 months after tofogliflozin administration. Ten patients with HF, T2DM, and SA were finally enrolled (60% men, 66.9 ± 13.4 years). Tofogliflozin reduced AHI from 43.2 [30.2] to 35.3 [13.1] events/h (p = 0.024) at 6 months. Hemoglobin A1c, body weight, and body water content decreased significantly. However, no significant changes were observed in the cardiorenal function parameters. A linear relationship was observed between the changes in body water content and AHI (r = 0.642, p = 0.045). Tofogliflozin reduced AHI, possibly associated with a reduction in body water content.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–402.
Ferrier K, Campbell A, Yee B, Richards M, O’Meeghan T, Weatherall M, et al. Sleep-disordered breathing occurs frequently in stable outpatients with congestive heart failure. Chest. 2005;128:2116–22.
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu KL, et al. Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol. 2007;49:1625–31.
Kasai T, Floras JS, Bradley TD. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation. 2012;126:1495–510.
Sato A, Kato T, Kasai T, Ishiwata S, Shoichiro Y, Hiroki M, et al. Relationship between inflammatory biomarkers and sleep-disordered breathing in patients with heart failure. Sleep Biol Rhythms. 2021;19:55–61.
Kato T, Suda S, Kasai T. Positive airway pressure therapy for heart failure. World J Cardiol. 2014;6:1175–91.
Akashiba T, Inoue Y, Uchimura N, Ohi M, Kasai T, Kawana F, et al. Sleep apnea syndrome (SAS) clinical practice guidelines 2020. Respir Investig. 2022;60:3–32.
Kasai T, Narui K, Dohi T, Yanagisawa N, Ishiwata S, Ohno M, et al. Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest. 2008;133:690–6.
Naughton MT, Rahman MA, Hara K, Floras JS, Bradley TD. Effect of continuous positive airway pressure on intrathoracic and left ventricular transmural pressures in patients with congestive heart failure. Circulation. 1995;91:1725–31.
Hall AB, Ziadi MC, Leech JA, Chen SY, Burwash IG, Renaud J, et al. Effects of short-term continuous positive airway pressure on myocardial sympathetic nerve function and energetics in patients with heart failure and obstructive sleep apnea: a randomized study. Circulation. 2014;130:892–901.
Kasai T, Bradley TD. Obstructive sleep apnea and heart failure: pathophysiologic and therapeutic implications. J Am Coll Cardiol. 2011;57:119–27.
Naito R, Kasai T, Dohi T, Takaya H, Narui K, Momomura SI. Factors associated with the improvement of left ventricular systolic function by continuous positive airway pressure therapy in patients with heart failure with reduced ejection fraction and obstructive sleep apnea. Front Neurol. 2022;13:781054.
Naito R, Kasai T, Tomita Y, Kasagi S, Narui K, Momomura SI. Clinical outcomes of chronic heart failure patients with unsuppressed sleep apnea by positive airway pressure therapy. Front Cardiovasc Med. 2023;10:1156353.
McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–24.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Bohm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
Neeland IJ, Eliasson B, Kasai T, Marx N, Zinman B, Inzucchi SE, et al. The impact of empagliflozin on obstructive sleep apnea and cardiovascular and renal outcomes: an exploratory analysis of the EMPA-REG OUTCOME trial. Diabetes Care. 2020;43:3007–15.
Wojeck BS, Inzucchi SE, Neeland IJ, Mancuso JP, Frederich R, Masiukiewicz U, et al. Ertugliflozin and incident obstructive sleep apnea: an analysis from the VERTIS CV trial. Sleep Breath. 2023;27:669–72.
Sawada K, Karashima S, Kometani M, Oka R, Takeda Y, Sawamura T, et al. Effect of sodium glucose cotransporter 2 inhibitors on obstructive sleep apnea in patients with type 2 diabetes. Endocr J. 2018;65:461–7.
Furukawa S, Miyake T, Senba H, Sakai T, Furukawa E, Yamamoto S, et al. The effectiveness of dapagliflozin for sleep-disordered breathing among Japanese patients with obesity and type 2 diabetes mellitus. Endocr J. 2018;65:953–61.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Version 2.2. Darien, IL: American Academy of Sleep Medicine; 2015.
Yamada Y, Nishizawa M, Uchiyama T, Kasahara Y, Shindo M, Miyachi M, et al. Developing and validating an age-independent equation using multi-frequency bioelectrical impedance analysis for estimation of appendicular skeletal muscle mass and establishing a cutoff for sarcopenia. Int J Environ Res Public Health. 2017;14:809.
Ballesteros-Pomar MD, Gonzalez-Arnaiz E, Pintor-de-la Maza B, Barajas-Galindo D, Ariadel-Cobo D, Gonzalez-Roza L, et al. Bioelectrical impedance analysis as an alternative to dual-energy X-ray absorptiometry in the assessment of fat mass and appendicular lean mass in patients with obesity. Nutrition. 2022;93:111442.
Shah P, Abel AAI, Boyalla V, Pellicori P, Kallvikbacka-Bennett A, Sze S, et al. A comparison of non-invasive methods of measuring body composition in patients with heart failure: a report from SICA-HF. ESC Heart Fail. 2021;8:3929–34.
Konishi M, Kagiyama N, Kamiya K, Saito H, Saito K, Ogasahara Y, et al. Impact of sarcopenia on prognosis in patients with heart failure with reduced and preserved ejection fraction. Eur J Prev Cardiol. 2021;28:1022–9.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14.
Blackman A, Foster GD, Zammit G, Rosenberg R, Aronne L, Wadden T, et al. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE Sleep Apnea randomized clinical trial. Int J Obes. 2016;40:1310–9.
Neeland IJ, McGuire DK, Chilton R, Crowe S, Lund SS, Woerle HJ, et al. Empagliflozin reduces body weight and indices of adipose distribution in patients with type 2 diabetes mellitus. Diabetes Vasc Dis Res. 2016;13:119–26.
Kaku K, Watada H, Iwamoto Y, Utsunomiya K, Terauchi Y, Tobe K, et al. Efficacy and safety of monotherapy with the novel sodium/glucose cotransporter-2 inhibitor tofogliflozin in Japanese patients with type 2 diabetes mellitus: a combined Phase 2 and 3 randomized, placebo-controlled, double-blind, parallel-group comparative study. Cardiovasc Diabetol. 2014;13:65.
Karg MV, Bosch A, Kannenkeril D, Striepe K, Ott C, Schneider MP, et al. SGLT-2-inhibition with dapagliflozin reduces tissue sodium content: a randomised controlled trial. Cardiovasc Diabetol. 2018;17:5.
Yumino D, Wang H, Floras JS, Newton GE, Mak S, Ruttanaumpawan P, et al. Prevalence and physiological predictors of sleep apnea in patients with heart failure and systolic dysfunction. J Card Fail. 2009;15:279–85.
Kasai T, Motwani SS, Elias RM, Gabriel JM, Taranto Montemurro L, Yanagisawa N, et al. Influence of rostral fluid shift on upper airway size and mucosal water content. J Clin Sleep Med. 2014;10:1069–74.
Yumino D, Redolfi S, Ruttanaumpawan P, Su MC, Smith S, Newton GE, et al. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation. 2010;121:1598–605.
Kasai T, Motwani SS, Yumino D, Gabriel JM, Montemurro LT, Amirthalingam V, et al. Contrasting effects of lower body positive pressure on upper airways resistance and partial pressure of carbon dioxide in men with heart failure and obstructive or central sleep apnea. J Am Coll Cardiol. 2013;61:1157–66.
Kasai T. Fluid retention and rostral fluid shift in sleep-disordered breathing. Curr Hypertens Rev. 2016;12:32–42.
da Silva BC, Kasai T, Coelho FM, Zatz R, Elias RM. Fluid redistribution in sleep apnea: therapeutic implications in edematous states. Front Med. 2017;4:256.
Redolfi S, Yumino D, Ruttanaumpawan P, Yau B, Su MC, Lam J, et al. Relationship between overnight rostral fluid shift and obstructive sleep apnea in nonobese men. Am J Respir Crit Care Med. 2009;179:241–6.
Oelze M, Kroller-Schon S, Welschof P, Jansen T, Hausding M, Mikhed Y, et al. The sodium–glucose co-transporter 2 inhibitor empagliflozin improves diabetes-induced vascular dysfunction in the streptozotocin diabetes rat model by interfering with oxidative stress and glucotoxicity. PLoS ONE. 2014;9:e112394.
Li X, Flynn ER, do Carmo JM, Wang Z, da Silva AA, Mouton AJ, et al. Direct cardiac actions of sodium–glucose cotransporter 2 inhibition improve mitochondrial function and attenuate oxidative stress in pressure overload-induced heart failure. Front Cardiovasc Med. 2022;9:859253.
Mone P, Varzideh F, Jankauskas SS, Pansini A, Lombardi A, Frullone S, et al. SGLT2 inhibition via empagliflozin improves endothelial function and reduces mitochondrial oxidative stress: insights from frail hypertensive and diabetic patients. Hypertension. 2022;79:1633–43.
Chen S, Coronel R, Hollmann MW, Weber NC, Zuurbier CJ. Direct cardiac effects of SGLT2 inhibitors. Cardiovasc Diabetol. 2022;21:45.
Christou K, Moulas AN, Pastaka C, Gourgoulianis KI. Antioxidant capacity in obstructive sleep apnea patients. Sleep Med. 2003;4:225–8.
Simiakakis M, Kapsimalis F, Chaligiannis E, Loukides S, Sitaras N, Alchanatis M. Lack of effect of sleep apnea on oxidative stress in obstructive sleep apnea syndrome (OSAS) patients. PLoS ONE. 2012;7:e39172.
Eisele HJ, Markart P, Schulz R. Obstructive sleep apnea, oxidative stress, and cardiovascular disease: evidence from human studies. Oxid Med Cell Longev. 2015;2015:608438.
Hosseini H, Homayouni-Tabrizi M, Amiri H, Safari-Faramani R, Moradi MT, Fadaei R, et al. The effect of continuous positive airway pressure on total antioxidant capacity in obstructive sleep apnea: a systematic review and meta-analysis. Sleep Breath. 2022. https://doi.org/10.1007/s11325-022-02733-9.
Christou K, Markoulis N, Moulas AN, Pastaka C, Gourgoulianis KI. Reactive oxygen metabolites (ROMs) as an index of oxidative stress in obstructive sleep apnea patients. Sleep Breath. 2003;7:105–10.
Peres BU, Allen AJH, Shah A, Fox N, Laher I, Almeida F, et al. Obstructive sleep apnea and circulating biomarkers of oxidative stress: a cross-sectional study. Antioxidants. 2020;9:476.
Jurado-Gamez B, Fernandez-Marin MC, Gomez-Chaparro JL, Munoz-Cabrera L, Lopez-Barea J, Perez-Jimenez F, et al. Relationship of oxidative stress and endothelial dysfunction in sleep apnoea. Eur Respir J. 2011;37:873–9.
Kobayashi S, Susa T, Tanaka T, Wada Y, Okuda S, Doi M, et al. Urinary 8-hydroxy-2′-deoxyguanosine reflects symptomatic status and severity of systolic dysfunction in patients with chronic heart failure. Eur J Heart Fail. 2011;13:29–36.
Shigiyama F, Kumashiro N, Miyagi M, Ikehara K, Kanda E, Uchino H, et al. Effectiveness of dapagliflozin on vascular endothelial function and glycemic control in patients with early-stage type 2 diabetes mellitus: DEFENCE study. Cardiovasc Diabetol. 2017;16:84.
Dekkers CCJ, Petrykiv S, Laverman GD, Cherney DZ, Gansevoort RT, Heerspink HJL. Effects of the SGLT-2 inhibitor dapagliflozin on glomerular and tubular injury markers. Diabetes Obes Metab. 2018;20:1988–93.
Ito H, Matsumoto S, Izutsu T, Kusano E, Kondo J, Inoue H, et al. Different renoprotective effects of luseogliflozin depend on the renal function at the baseline in patients with type 2 diabetes: a retrospective study during 12 months before and after initiation. PLoS ONE. 2021;16:e0248577.
Yamagishi K, Ohira T, Nakano H, Bielinski SJ, Sakurai S, Imano H, et al. Cross-cultural comparison of the sleep-disordered breathing prevalence among Americans and Japanese. Eur Respir J. 2010;36:379–84.
Funding
This study was partly supported by JSPS KAKENHI (Grant Numbers, JP21K08116 and JP21K16034) and a Grant-in-Aid for Scientific Research (Grant Numbers, 20FC1027 and 23FC1031) from the Ministry of Health, Labor and Welfare of Japan, a research grant from the Japanese Center for Research on Women in Sport, Juntendo University. These funding sources did not play any other role in this study.
Author information
Authors and Affiliations
Contributions
SI contributed to the study. SI and TK contributed to the study design. AS, SS, HM, JS, SY, AM, MS, TK, MH, SN, MK, and FK collected data. SI, RN, KM, and TK performed data and statistical analyses. SI and TK drafted the manuscript. SI, TK, AS, SS, HM, JS, SY, AM, MS, TK, MH, SN, MK, and FK performed critical revision, editing, and approval of the final manuscript. SI, TK, HD, and TM are responsible for the overall content of guarantors.
Corresponding author
Ethics declarations
Conflict of interest
SI and T Kasai contributed to the study design. AS, SS, HM, JS, SY, AM, MS, T Kato, MH, SN, MK, and FK collected data. SI, RN, KM, and T Kasai performed data and statistical analyses. SI and T Kasai drafted the manuscript. SI, T Kasai, AS, SS, HM, JS, SY, AM, MS, T Kato, MH, SN, MK, and FK performed critical revision, editing, and approval of the final manuscript. SI, T Kasai, HD, and TM are responsible for the overall content of guarantors
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishiwata, S., Kasai, T., Sato, A. et al. Tofogliflozin reduces sleep apnea severity in patients with type 2 diabetes mellitus and heart failure: a prospective study. Hypertens Res 48, 388–397 (2025). https://doi.org/10.1038/s41440-024-01982-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01982-3