Abstract
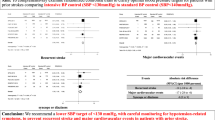
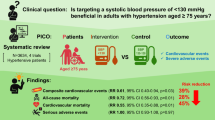
We conducted a systematic review and meta-analysis to evaluate the effects of intensive versus standard antihypertensive therapy on cardiovascular outcomes in adult patients with hypertension. The primary endpoints were composite cardiovascular events, all-cause death, cardiovascular death, and serious adverse events. The secondary endpoints included cognitive impairment, hypotension, syncope, acute kidney injury, and composite renal outcomes. Eight trials classifying a systolic blood pressure (SBP) target of <130 mmHg as intensive control was adopted in the primary analysis. The intensive blood pressure (BP) control significantly reduced the relative risk (RR) for cardiovascular events and cardiovascular death compared to standard BP control (RR 0.83 [95% confidence interval, 0.76–0.90] and 0.74 [0.56–0.97], respectively). The intensive BP control tended to reduce the RR for all-cause death, but not significant (0.89 [0.78–1.02]). On the other hand, the intensive BP control significantly increased the RR for serious adverse events, hypotension, and syncope (1.59 [1.19–2.12], 1.96 [1.04–3.70], and 2.36 [1.95–2.85], respectively). The intensive BP control significantly increased the RR for acute kidney injury (2.65 [1.78–3.95]), but did not affect for composite renal outcomes (1.38 [0.83–2.31]). For cognitive impairment, no significant increase or decrease in risk was observed (0.93 [0.68–1.26]). Based on these findings, we recommend the intensive BP control targeting SBP below 130 mmHg to achieve significant reductions in cardiovascular events and cardiovascular death, accompanied by careful monitoring for potential adverse events including acute kidney injury, hypotension, syncope related with the intensive BP control.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Fujiyoshi A, Ohkubo T, Miura K, Murakami Y, Nagasawa S-y, Okamura T, et al. Blood pressure categories and long-term risk of cardiovascular disease according to age group in Japanese men and women. Hypertens Res. 2012;35:947–53.
Takashima N, Ohkubo T, Miura K, Okamura T, Murakami Y, Fujiyoshi A, et al. Long-term risk of BP values above normal for cardiovascular mortality: a 24-year observation of Japanese aged 30 to 92 years. J Hypertens. 2012;30:2299–306.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899–911.
Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N Engl J Med. 2019;381:243–51.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Bundy JD, Li C, Stuchlik P, Bu X, Kelly TN, Mills KT, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2:775–81.
Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:28–36.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure-lowering treatment on cardiovascular outcomes and mortality: 13 – benefits and adverse events in older and younger patients with hypertension: overview, meta-analyses and meta-regression analyses of randomized trials. J Hypertens. 2018;36:1622–36.
Luo D, Cheng Y, Zhang H, Ba M, Chen P, Li H, et al. Association between high blood pressure and long term cardiovascular events in young adults: systematic review and meta-analysis. BMJ. 2020;370:m3222.
Rahimi K, Bidel Z, Nazarzadeh M, Copland E, Canoy D, Ramakrishnan R, et al. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–36.
Bidel Z, Nazarzadeh M, Canoy D, Copland E, Gerdts E, Woodward M, et al. Sex-specific effects of blood pressure lowering pharmacotherapy for the prevention of cardiovascular disease: an individual participant-level data meta-analysis. Hypertension. 2023;80:2293–302.
Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43.
Whelton PK, O’Connell S, Mills KT, He J. Optimal antihypertensive systolic blood pressure: a systematic review and meta-analysis. Hypertension. 2024;81:2329–39.
Sakima A, Satonaka H, Nishida N, Yatsu K, Arima H. Optimal blood pressure targets for patients with hypertension: a systematic review and meta-analysis. Hypertens Res. 2019;42:483–95.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary. J Am Coll Cardiol. 2018;71:2199–269.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071.
McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension: developed by the task force on the management of elevated blood pressure and hypertension of the European Society of Cardiology (ESC) and endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO). Eur Heart J. 2024;45:3912–4018.
ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85.
Sprint Research Group, Wright JT Jr., Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
The SPRINT Research Group. Final report of a trial of intensive versus standard blood-pressure control. N Engl J Med. 2021;384:1921–30.
Liu J, Li Y, Ge J, Yan X, Zhang H, Zheng X, et al. Lowering systolic blood pressure to less than 120 mm Hg versus less than 140 mm Hg in patients with high cardiovascular risk with and without diabetes or previous stroke: an open-label, blinded-outcome, randomised trial. Lancet. 2024;404:245–55.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
White WB, Wakefield DB, Moscufo N, Guttmann CRG, Kaplan RF, Bohannon RW, et al. Effects of Intensive versus standard ambulatory blood pressure control on cerebrovascular outcomes in older people (INFINITY). Circulation. 2019;140:1626–35.
Hayashi K, Saruta T, Goto Y, Ishii M, on behalf of the JSG. Impact of renal function on cardiovascular events in elderly hypertensive patients treated with efonidipine. Hypertens Res. 2010;33:1211–20.
Jatos Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008;31:2115–27.
Ogihara T, Saruta T, Rakugi H, Matsuoka H, Shimamoto K, Shimada K, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly. Hypertension. 2010;56:196–202.
Wei Y, Jin Z, Shen G, Zhao X, Yang W, Zhong Y, et al. Effects of intensive antihypertensive treatment on Chinese hypertensive patients older than 70 years. J Clin Hypertens. 2013;15:420–7.
Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, Ganau A, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374:525–33.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–10.
Mant J, McManus RJ, Roalfe A, Fletcher K, Taylor CJ, Martin U, et al. Different systolic blood pressure targets for people with history of stroke or transient ischaemic attack: PAST-BP (Prevention After Stroke—Blood Pressure) randomised controlled trial. BMJ. 2016;352:i708.
Bath PM, Scutt P, Blackburn DJ, Ankolekar S, Krishnan K, Ballard C, et al. Intensive versus Guideline blood pressure and lipid lowering in patients with previous stroke: main results from the pilot ‘Prevention of Decline in Cognition after Stroke Trial’ (PODCAST) randomised controlled trial. PLoS ONE. 2017;12:e0164608.
Markus HS, Egle M, Croall ID, Sari H, Khan U, Hassan A, et al. PRESERVE: randomized trial of intensive versus standard blood pressure control in small vessel disease. Stroke. 2021;52:2484–93.
Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M, et al. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365:939–46.
Kitagawa K, Yamamoto Y, Arima H, Maeda T, Sunami N, Kanzawa T, et al. Effect of standard vs intensive blood pressure control on the risk of recurrent stroke: a randomized clinical trial and meta-analysis. JAMA Neurol. 2019;76:1309–18.
Schrier R, McFann K, Johnson A, Chapman A, Edelstein C, Brosnahan G, et al. Cardiac and renal effects of standard versus rigorous blood pressure control in autosomal-dominant polycystic kidney disease: results of a seven-year prospective randomized study. J Am Soc Nephrol. 2002;13:1733–9.
SPS3 Study Group BO, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13.
Appel LJ, Wright JT, Greene T, Agodoa LY, Astor BC, Bakris GL, et al. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010;363:918–29.
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673–82.
Kitagawa K, Arima H, Yamamoto Y, Ueda S, Rakugi H, Kohro T, et al. Intensive or standard blood pressure control in patients with a history of ischemic stroke: RESPECT post hoc analysis. Hypertens Res. 2022;45:591–601.
Benavente OR, White CL, Pearce L, Pergola P, Roldan A, Benavente M-F, et al. The secondary prevention of small subcortical strokes (SPS3) study. Int J Stroke. 2011;6:164–75.
Norris K, Bourgoigne J, Gassman J, Hebert L, Middleton J, Phillips RA, et al. Cardiovascular outcomes in the African American study of kidney disease and hypertension (AASK) trial. Am J Kidney Dis. 2006;48:739–51.
Beddhu S, Rocco MV, Toto R, Craven TE, Greene T, Bhatt U, et al. Effects of intensive systolic blood pressure control on kidney and cardiovascular outcomes in persons without kidney disease. Ann Intern Med. 2017;167:375–83.
The SPRINT MIND Investigators for the SPRINT Research Group. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321:553–61.
Williamson JD, Launer LJ, Bryan RN, Coker LH, Lazar RM, Gerstein HC, et al. Cognitive function and brain structure in persons with type 2 diabetes mellitus after intensive lowering of blood pressure and lipid levels: a randomized clinical trial. JAMA Intern Med. 2014;174:324–33.
Rocco MV, Sink KM, Lovato LC, Wolfgram DF, Wiegmann TB, Wall BM, et al. Effects of intensive blood pressure treatment on acute kidney injury events in the systolic blood pressure intervention trial (SPRINT). Am J Kidney Dis. 2018;71:352–61.
Bress AP, Greene T, Derington CG, Shen J, Xu Y, Zhang Y, et al. Patient selection for intensive blood pressure management based on benefit and adverse events. J Am Coll Cardiol. 2021;77:1977–90.
Fleg JL, Evans GW, Margolis KL, Barzilay J, Basile JN, Bigger JT, et al. Orthostatic hypotension in the ACCORD (Action to Control Cardiovascular Risk in Diabetes) blood pressure trial. Hypertension. 2016;68:888–95.
Pearce LA, McClure LA, Anderson DC, Jacova C, Sharma M, Hart RG, et al. Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke: a secondary analysis from the SPS3 randomised trial. Lancet Neurol. 2014;13:1177–85.
Peralta CA, McClure LA, Scherzer R, Odden MC, White CL, Shlipak M, et al. Effect of intensive versus usual blood pressure control on kidney function among individuals with prior lacunar stroke. Circulation. 2016;133:584–91.
Ismail-Beigi F, Craven TE, O’Connor PJ, Karl D, Calles-Escandon J, Hramiak I, et al. Combined intensive blood pressure and glycemic control does not produce an additive benefit on microvascular outcomes in type 2 diabetic patients. Kidney Int. 2012;81:586–94.
Margolis KL, Palermo L, Vittinghoff E, Evans GW, Atkinson HH, Hamilton BP, et al. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med. 2014;29:1599–606.
Wu W, Liu J, Li A, Li J, Yang Y, Ye X, et al. Effect of intensive blood pressure control on carotid morphology and hemodynamics in chinese patients with hyperhomocysteinemia-type hypertension and high risk of stroke. Med Sci Monit. 2019;25:5717–26.
Lessing C, Schmitz A, Albers B, Schrappe M. Impact of sample size on variation of adverse events and preventable adverse events: systematic review on epidemiology and contributing factors. Qual Saf Health Care. 2010;19:e24.
Inker LA, Heerspink HJL, Tighiouart H, Levey AS, Coresh J, Gansevoort RT, et al. GFR slope as a surrogate end point for kidney disease progression in clinical trials: a meta-analysis of treatment effects of randomized controlled trials. J Am Soc Nephrol. 2019;30:1735–45.
Kohro T, Yamazaki T, Izumi T, Daida H, Kurabayashi M, Miyauchi K, et al. Intensively lowering both low-density lipoprotein cholesterol and blood pressure does not reduce cardiovascular risk in Japanese coronary artery disease patients. Circ J. 2011;75:2062–70.
Weir MR, Yeh F, Silverman A, Devereux RB, Galloway JM, Henderson JA, et al. Safety and feasibility of achieving lower systolic blood pressure goals in persons with type 2 diabetes: the SANDS trial. J Clin Hypertens. 2009;11:540–8.
Howard BV, Roman MJ, Devereux RB, Fleg JL, Galloway JM, Henderson JA, et al. Effect of lower targets for blood pressure and LDL cholesterol on atherosclerosis in diabetes: the SANDS randomized trial. JAMA. 2008;299:1678–89.
Acknowledgements
This systematic review and meta-analysis is a project adopted by the Japanese Society of Hypertension for Management of Hypertension 2025 (JSH2025). We sincerely appreciate Dr. Hisatomi Arima for supervising the draft to ensure that its structure was appropriate for systematic review and meta-analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haze, T., Katsurada, K., Sakata, S. et al. Effect of intensive versus standard blood pressure control on cardiovascular outcomes in adult patients with hypertension: a systematic review and meta-analysis. Hypertens Res 48, 1846–1858 (2025). https://doi.org/10.1038/s41440-025-02131-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02131-0
Keywords
This article is cited by
-
The conservative–challenging paradigm of antihypertensive therapy in JSH2025: a comparative perspective with contemporary Western guidelines
Hypertension Research (2026)
-
The Japanese Society of Hypertension Guidelines for the management of elevated blood pressure and hypertension 2025 (JSH2025)
Hypertension Research (2026)
-
Advancing evidence-based blood pressure targets in JSH2025
Hypertension Research (2026)
-
Achievement rate of blood pressure control <130/80 mmHg as the core metric of implementation hypertension, based on the new JSH2025 and AHA/ACC2025 guidelines
Hypertension Research (2025)
-
Key highlights of the Japanese Society of Hypertension Guidelines for the management of elevated blood pressure and hypertension 2025 (JSH2025)
Hypertension Research (2025)