Abstract
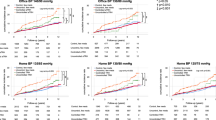
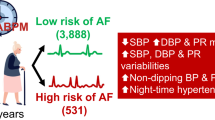
Vascular Ehlers-Danlos syndrome (vEDS) is an inherited connective tissue disorder characterized by arterial fragility. Celiprolol is a β1-adrenoceptor antagonist with partial β2 agonist activity capable of reducing rates of vascular events in this setting, though the underlying mechanisms have yet to be elucidated. In particular, no conclusive evidence exists on its impact on blood pressure (BP) parameters in patients with vEDS. Accordingly, the aim of our study was to perform a comprehensive assessment of BP profile in a cohort of patients with vEDS receiving celiprolol titrated to the maximum tolerated dose. Consecutive outpatients with molecularly confirmed vEDS undergoing office BP measurement and 24-h ambulatory BP monitoring (ABPM) were retrospectively evaluated. Using 24-h systolic BP, diastolic BP, mean BP, and pulse pressure (PP) (mmHg) values, indices of short-term BP variability were calculated. A generalized linear regression model was applied to analyze the correlation between initial values of BP parameters and their variation with celiprolol therapy. Overall, 20 subjects were included (12 females). Eight patients (40%) had 24-h ABPM values consistent with hypertension. Five subjects (25%) defined hypertensives at 24-h ABPM had optimal BP control at office BP measurement, suggesting a “masked” hypertension. A significant correlation was found between initial values of indices of short-term PP variability and their change with celiprolol therapy, with a particularly high Pearson’s index for PP coefficient of variation (r = −0.926; p < 0.001). In patients with vEDS, 24-h ABPM is confirmed a reliable tool in identifying hypertension phenotypes. Treatment with celiprolol may reduce PP variability proportionally to its initial magnitude. Dedicated studies on larger cohorts should evaluate whether short-term PP variability is a reliable prognostic marker and therapeutic target in this clinical setting.

In our study, treatment with celiprolol seemed to reduce short-term PP variability proportionally to its initial magnitude in patients with vEDS. Furthermore, two out of four patients experiencing vascular events during the study period displayed the highest short-term PP variability values recorded in the entire cohort. Further research should evaluate whether such parameters are reliable prognostic markers and therapeutic targets in this clinical setting. ABPM ambulatory blood pressure monitoring, ARV average real variability, BP blood pressure, CV coefficient of variation, DBP diastolic blood pressure, PP pulse pressure, SBP systolic blood pressure, SD standard deviation, TRI time-rate index, vEDS vascular Ehlers-Danlos syndrome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research data is not publicly available.
References
Byers PH, Belmont J, Black J, De Backer J, Frank M, Jeunemaitre X, et al. Diagnosis, natural history, and management in vascular Ehlers-Danlos syndrome. Am J Med Genet C Semin Med Genet. 2017;175:40–7.
Pepin MG, Schwarze U, Rice KM, Liu M, Leistritz D, Byers PH. Survival is affected by mutation type and molecular mechanism in vascular Ehlers-Danlos syndrome (EDS type IV). Genet Med. 2014;16:881–8.
Pepin M, Schwarze U, Superti-Furga A, Byers PH. Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med. 2000;342:673–80.
Frank M, Adham S, Seigle S, Legrand A, Mirault T, Henneton P, et al. Vascular Ehlers-Danlos syndrome: long-term observational study. J Am Coll Cardiol. 2019;73:1948–57.
Baderkhan H, Wanhainen A, Stenborg A, Stattin EL, Bjorck M. Celiprolol treatment in patients with vascular Ehlers-Danlos syndrome. Eur J Vasc Endovasc Surg. 2021;61:326–31.
Buso G, Paini A, Agabiti-Rosei C, De Ciuceis C, Bertacchini F, Stassaldi D, et al. Despite celiprolol therapy, patients with vascular Ehlers-Danlos syndrome remain at risk of vascular events: a 12-year experience in an Italian referral center. Vasc Med. 2023: 29:265–73.
Boutouyrie P, Bussy C, Hayoz D, Hengstler J, Dartois N, Laloux B, et al. Local pulse pressure and regression of arterial wall hypertrophy during long-term antihypertensive treatment. Circulation. 2000;101:2601–6.
Ong KT, Perdu J, De Backer J, Bozec E, Collignon P, Emmerich J, et al. Effect of celiprolol on prevention of cardiovascular events in vascular Ehlers-Danlos syndrome: a prospective randomised, open, blinded-endpoints trial. Lancet. 2010;376:1476–84.
Caruso FS, Berger BM, Darragh A, Weng T, Vukovich R. Effect of celiprolol, a new beta 1-alpha 2 blocker, on the cardiovascular response to exercise. J Clin Pharmacol. 1986;26:32–8.
Ritelli M, Rovati C, Venturini M, Chiarelli N, Cinquina V, Castori M, et al. Application of the 2017 criteria for vascular Ehlers-Danlos syndrome in 50 patients ascertained according to the Villefranche nosology. Clin Genet. 2020;97:287–95.
Mancia G, Kreutz R, Brunstrom M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–66.
Zakopoulos NA, Tsivgoulis G, Barlas G, Papamichael C, Spengos K, Manios E, et al. Time rate of blood pressure variation is associated with increased common carotid artery intima-media thickness. Hypertension. 2005;45:505–12.
Mena L, Pintos S, Queipo NV, Aizpurua JA, Maestre G, Sulbaran T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23:505–11.
Dolan E, Thijs L, Li Y, Atkins N, McCormack P, McClory S, et al. Ambulatory arterial stiffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension. 2006;47:365–70.
Gavish B, Ben-Dov IZ, Bursztyn M. Linear relationship between systolic and diastolic blood pressure monitored over 24 h: assessment and correlates. J Hypertens. 2008;26:199–209.
Pauca AL, O’Rourke MF, Kon ND. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension. 2001;38:932–7.
Wilkinson IB, MacCallum H, Flint L, Cockcroft JR, Newby DE, Webb DJ. The influence of heart rate on augmentation index and central arterial pressure in humans. J Physiol. 2000;525:263–70.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802.
de Simone G, Roman MJ, De Marco M, Bella JN, Izzo R, Lee ET, et al. Hemodynamic correlates of abnormal aortic root dimension in an adult population: the Strong Heart Study. J Am Heart Assoc. 2015;4:e002309.
Covella M, Milan A, Totaro S, Cuspidi C, Re A, Rabbia F, et al. Echocardiographic aortic root dilatation in hypertensive patients: a systematic review and meta-analysis. J Hypertens. 2014;32:1928–35.
Vasan RS, Larson MG, Levy D. Determinants of echocardiographic aortic root size. The Framingham Heart Study. Circulation. 1995;91:734–40.
Kobeissi E, Hibino M, Pan H, Aune D. Blood pressure, hypertension and the risk of abdominal aortic aneurysms: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. 2019;34:547–55.
Dong N, Piao H, Li B, Xu J, Wei S, Liu K. Poor management of hypertension is an important precipitating factor for the development of acute aortic dissection. J Clin Hypertens. 2019;21:804–12.
Boutouyrie P, Germain DP, Fiessinger JN, Laloux B, Perdu J, Laurent S. Increased carotid wall stress in vascular Ehlers-Danlos syndrome. Circulation. 2004;109:1530–5.
Buso G, Corvini F, Fusco EM, Messina M, Cherubini F, Laera N, et al. Current evidence and future perspectives in the medical management of vascular Ehlers-Danlos syndrome: focus on vascular prevention. J Clin Med. 2024;13:4255.
Jondeau G, Boutouyrie P, Lacolley P, Laloux B, Dubourg O, Bourdarias JP, et al. Central pulse pressure is a major determinant of ascending aorta dilation in Marfan syndrome. Circulation. 1999;99:2677–81.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55.
Schutte AE, Kollias A, Stergiou GS. Blood pressure and its variability: classic and novel measurement techniques. Nat Rev Cardiol. 2022;19:643–54.
Mancia G, Parati G, Pomidossi G, Casadei R, Di Rienzo M, Zanchetti A. Arterial baroreflexes and blood pressure and heart rate variabilities in humans. Hypertension. 1986;8:147–53.
Parati G, Saul JP, Di Rienzo M, Mancia G. Spectral analysis of blood pressure and heart rate variability in evaluating cardiovascular regulation. A critical appraisal. Hypertension. 1995;25:1276–86.
Conway J, Boon N, Davies C, Jones JV, Sleight P. Neural and humoral mechanisms involved in blood pressure variability. J Hypertens. 1984;2:203–8.
Schillaci G, Bilo G, Pucci G, Laurent S, Macquin-Mavier I, Boutouyrie P, et al. Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension. 2012;60:369–77.
Parati G, Ochoa JE, Salvi P, Lombardi C, Bilo G. Prognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetes. Diabetes Care. 2013;36(Suppl 2):S312–24.
Mancia G, Parati G, Hennig M, Flatau B, Omboni S, Glavina F, et al. Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens. 2001;19:1981–9.
Tatasciore A, Renda G, Zimarino M, Soccio M, Bilo G, Parati G, et al. Awake systolic blood pressure variability correlates with target-organ damage in hypertensive subjects. Hypertension. 2007;50:325–32.
Manios E, Tsagalis G, Tsivgoulis G, Barlas G, Koroboki E, Michas F, et al. Time rate of blood pressure variation is associated with impaired renal function in hypertensive patients. J Hypertens. 2009;27:2244–8.
de la Sierra A, Williams B, Bursztyn M, Parati G, Stergiou GS, Vinyoles E, et al. Prognostic relevance of short-term blood pressure variability. The Spanish ABPM Registry. Hypertension. 2024;81:1125–31.
Palatini P, Reboldi G, Saladini F, Angeli F, Mos L, Rattazzi M, et al. Dipping pattern and short-term blood pressure variability are stronger predictors of cardiovascular events than average 24-h blood pressure in young hypertensive subjects. Eur J Prev Cardiol. 2022;29:1377–86.
Zhang L, Tian W, Feng R, Song C, Zhao Z, Bao J, et al. Prognostic impact of blood pressure variability on aortic dissection patients after endovascular therapy. Medicine. 2015;94:e1591.
Katsanos AH, Alexandrov AV, Mandava P, Kohrmann M, Soinne L, Barreto AD, et al. Pulse pressure variability is associated with unfavorable outcomes in acute ischaemic stroke patients treated with intravenous thrombolysis. Eur J Neurol. 2020;27:2453–62.
Kamieniarz-Medrygal M, Kazmierski R. Significance of pulse pressure variability in predicting functional outcome in acute ischemic stroke: a retrospective, single-center, observational cohort study. Sci Rep. 2023;13:3618.
Huang JT, Cheng HM, Yu WC, Lin YP, Sung SH, Chen CH. Increased nighttime pulse pressure variability but not ambulatory blood pressure levels predicts 14-year all-cause mortality in patients on hemodialysis. Hypertension. 2019;74:660–8.
Nawarskas JJ, Cheng-Lai A, Frishman WH. Celiprolol: a unique selective adrenoceptor modulator. Cardiol Rev. 2017;25:247–53.
Mancia G, Facchetti R, Cuspidi C, Bombelli M, Corrao G, Grassi G. Limited reproducibility of MUCH and WUCH: evidence from the ELSA study. Eur Heart J. 2020;41:1565–71.
Acknowledgements
We express our gratitude to Dr. Stefania Orini, MD, for her valuable contribution to the conceptualization of statistical analysis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Buso, G., Gatta, R., Corvini, F. et al. Short-term pulse pressure variability: a novel prognostic marker and therapeutic target in patients with vascular Ehlers-Danlos syndrome? Preliminary results from a pilot study. Hypertens Res 48, 1529–1541 (2025). https://doi.org/10.1038/s41440-025-02135-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02135-w