Abstract
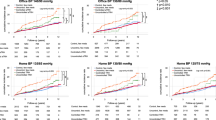
Although hypertension is a risk factor for cardiovascular (CVD) events in stage B heart failure (HF), data on the prognostic value of home blood pressure (BP) measurements in stage B HF are limited. We retrospectively analyzed the cases of 568 patients with stage B HF and at least one cardiovascular risk factor who underwent home BP monitoring. Stage B HF was defined as BNP ≥ 35 pg/mL or NT-proBNP ≥125 pg/mL, Troponin T > 0.014 ng/mL, LVEF < 50%, enlarged left ventricular dimensions in diastole (men: ≥60 mm; women: ≥54 mm), enlarged left atrium (men: >40 mm; women: >38 mm), or increased left ventricular mass (men: >115 g/m2; women: >95 g/m2). Office hypertension was defined as systolic BP ≥ 140 mmHg. Home BP was measured in the morning, evening, and nighttime; morning/evening home hypertension was defined as ≥135 mmHg and nighttime home hypertension as ≥120 mmHg. During a mean follow-up of 7.8 ± 3.6 years, 66 CVD events occurred. An unadjusted Cox regression model gave the following hazard ratios (HRs) and 95% confidence intervals (CIs) for CVD-events risk in patients with office, morning, evening, and nighttime home hypertension: HR 1.69 (95% CI 1.03–2.78), 1.73 (1.02–2.95), 1.44 (0.89–2.33) and 2.33 (1.34–4.04), respectively. In a multivariate Cox regression analysis adjusting for significant variables, the association with CVD events remained only for nighttime home hypertension (HR 1.89; 95% CI 1.06–3.38), not other hypertension types. In conclusion, hypertension defined based on nighttime home BP was associated with CVD-events risk in stage B HF patients.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Young KA, Scott CG, Rodeheffer RJ, Chen HH. Progression of preclinical heart failure: a description of stage A and B heart failure in a community population. Circ Cardiovasc Qual Outcomes. 2021;14:e007216.
Tsutsui H, Isobe M, Ito H, Okumura K, Ono M, Kitakaze M, et al. JCS 2017/JHFS 2017 Guideline on diagnosis and treatment of acute and chronic heart failure-digest version. Circ J. 2019;83:2084–184.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e895–e1032.
Parveen S, Zareini B, Arulmurugananthavadivel A, Kistorp C, Faber J, Køber L, et al. Association between early detected heart failure stages and future cardiovascular and non-cardiovascular events in the elderly (Copenhagen Heart Failure Risk Study). BMC Geriatr. 2022;22:230.
Kaneko H, Yano Y, Itoh H, Morita K, Kiriyama H, Kamon T, et al. Association of Blood Pressure Classification Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Risk of Heart Failure and Atrial Fibrillation. Circulation. 2021;143:2244–53.
Miao H, Zou C, Yang S, Chia YC, Van Huynh M, Sogunuru GP, et al. Targets and management of hypertension in heart failure: focusing on the stages of heart failure. J Clin Hypertens 2022;24:1218–25.
Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, Hashimoto J, et al. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens. 2004;22:1099–104.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5.
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population. Hypertension. 2016;68:54–61.
Komori T, Eguchi K, Tomizawa H, Ishikawa J, Hoshide S, Shimada K, et al. Factors associated with incident ischemic stroke in hospitalized heart failure patients: a pilot study. Hypertens Res. 2008;31:289–94.
Kario K, Kanegae H, Tomitani N, Okawara Y, Fujiwara T, Yano Y, et al. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension. 2019;73:1240–8.
Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid CM, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur J Heart Fail. 2021;23:352–80.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Khattar RS, Swales JD, Dore C, Senior R, Lahiri A. Effect of aging on the prognostic significance of ambulatory systolic, diastolic, and pulse pressure in essential hypertension. Circulation. 2001;104:783–9.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14.
Teichholz LE, Kreulen T, Herman MV, Gorlin R. Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence of absence of asynergy. Am J Cardiol. 1976;37:7–11.
Hoshide S, Kanegae H, Kario K. Nighttime home blood pressure as a mediator of N-terminal pro-brain natriuretic peptide in cardiovascular events. Hypertens Res. 2021;44:1138–46.
Kario K. Nocturnal hypertension: new technology and evidence. Hypertension. 2018;71:997–1009.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e61.
Acknowledgements
We greatly appreciate the study investigators at each of the study sites who participated in the J-HOP study.
Funding
This study was financially supported in part by a grant from the 21st Century Center of Excellence Project run by Japan’s Ministry of Education, Culture, Sports, Science, and Technology (MEXT); a grant from the Foundation for Development of the Community (Tochigi); a grant from Omron Healthcare Co., Ltd; a Grant-in-Aid for Scientific Research (B; 21390247) from The Ministry of Education, Culture, Sports, Science, and Technology of Japan, 2009–2013; and funds from the MEXT-supported program for the Strategic Research Foundation at Private Universities, 2011–2015 Cooperative Basic and Clinical Research on Circadian Medicine (S1101022) to K. Kario. Funding sponsors had no role in forming study design and conducting of the study; the collection, management, analysis, and interpretation of the data; the preparation of the article; and decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T.K.: none. S.H.: none, K. Kario has received research grants from Omron Healthcare Co., Ltd., A&D Co., Ltd., and Fukuda Denshi Co., Ltd.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Komori, T., Hoshide, S. & Kario, K. The prognostic impact of home blood pressure measurements in patients with stage B heart failure. Hypertens Res 48, 1779–1786 (2025). https://doi.org/10.1038/s41440-025-02174-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02174-3
Keywords
This article is cited by
-
Home blood pressure monitoring for improved risk assessment in heart failure: are brachial measurements sufficient?
Hypertension Research (2025)