Abstract
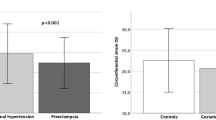
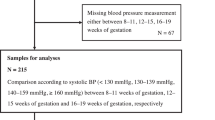
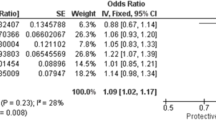
Preeclampsia (PE) is a pregnancy disorder characterized by systemic endothelial damage that leads to long-term cardiovascular complications. The endothelial glycocalyx (EG) covers the luminal surface of endothelium playing a critical role in vascular homeostasis. In this study we aimed to evaluate EG thickness and blood pressure (BP) trends in women with a history of PE vs. normotensive pregnancy. Fifty-five women participated in the study (18 controls, 34 with PE, and 3 with gestational hypertension). Six years postpartum, we evaluated the sublingual microcirculation by sidestream dark-field microscopy, and assessed BP in the sitting and orthostatic position. At follow-up, women with PE had reduced EG thickness in vessels ≥ 8 µm, expressed by an increased perfused boundary region (PBR), compared to healthy controls (median 3.14 vs. 2.88 µm, p = 0.002). A trend towards increased red blood cell velocity in vessels ≥ 10 µm was also observed in PE vs. controls. The systolic and diastolic BP, as well as within-visit BP variability, were significantly higher in PE vs. controls. Adverse neonatal outcomes, umbilical artery Doppler and BP during both the pregnancy and the follow-up visit, were associated with maternal PBR value in vessels ≥ 8 µm. This study contributes to the existing literature on PE and the increased risk of future cardiovascular disease, highlighting the critical role of EG and BP regulatory mechanisms. Our results showed that the severity of hemodynamic and neonatal impairments during pregnancy may irreversibly affect the EG and thereby be associated with long-term maternal vascular dysfunction.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24–43.
Dimitriadis E, Rolnik DL, Zhou W, Estrada-Gutierrez G, Koga K, Francisco RPV, et al. Pre-eclampsia. Nat Rev Dis Prim. 2023;9:8.
Yang Q, Han K, Wang J, Zou Y. Literature overview of association between preeclampsia and cardiovascular risk. Anatol J Cardiol. 2023;27:179–84.
Sederholm Lawesson S, Swahn E, Pihlsgard M, Andersson T, Angeras O, Bacsovics Brolin E, et al. Association between history of adverse pregnancy outcomes and coronary artery disease assessed by coronary computed tomography angiography. JAMA. 2023;329:393–404.
Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, Nirantharakumar K, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. BMJ. 2020;371:m3502.
Thomopoulos C, Hitij JB, De Backer T, Gkaliagkousi E, Kreutz R, Lopez-Sublet M, et al. Management of hypertensive disorders in pregnancy: a Position Statement of the European Society of Hypertension Working Group ‘Hypertension in Women’. J Hypertens. 2024(e-pub ahead of print 2024/05/01; https://doi.org/10.1097/hjh.0000000000003739).
Armaly Z, Jadaon JE, Jabbour A, Abassi ZA. Preeclampsia: novel mechanisms and potential therapeutic approaches. Front Physiol. 2018;9:973.
Reitsma S, Slaaf DW, Vink H, van Zandvoort MA, oude Egbrink MG. The endothelial glycocalyx: composition, functions, and visualization. Pflug Arch. 2007;454:345–59.
Afsar B, Afsar RE. The role of glycosaminoglycans in blood pressure regulation. Microcirculation. 2023;30:e12832.
Hu Z, Cano I, D’Amore PA. Update on the role of the endothelial glycocalyx in angiogenesis and vascular inflammation. Front Cell Dev Biol. 2021;9:734276.
Rana S, Burke SD, Karumanchi SA. Imbalances in circulating angiogenic factors in the pathophysiology of preeclampsia and related disorders. Am J Obstet Gynecol. 2022;226:S1019–s34.
Piani F, Tossetta G, Cara-Fuentes G, Agnoletti D, Marzioni D, Borghi C Diagnostic and prognostic role of CD93 in cardiovascular disease: a systematic review. Biomolecules. 2023;13:1–14.
Piani F, Tossetta G, Fantone S, Agostinis C, Di Simone N, Mandalà M, et al. First Trimester CD93 as a Novel Marker of Preeclampsia and Its Complications: A Pilot Study. High Blood Press Cardiovasc Prev. 2023;30:591–4.
Maselienė T, Struckutė E, Breivienė R, Ramašauskaitė D, Dženkevičiūtė V The importance of inflammatory and angiogenic markers in the evaluation of early cardiovascular disease risk in women with hypertensive disorders of pregnancy. J Cardiovasc Dev Dis. 2023;10.
Nieuwdorp M, Mooij HL, Kroon J, Atasever B, Spaan JA, Ince C, et al. Endothelial glycocalyx damage coincides with microalbuminuria in type 1 diabetes. Diabetes. 2006;55:1127–32.
Dane MJ, Khairoun M, Lee DH, van den Berg BM, Eskens BJ, Boels MG, et al. Association of kidney function with changes in the endothelial surface layer. Clin J Am Soc Nephrol. 2014;9:698–704.
Scioscia M, Siwetz M, Robillard PY, Brizzi A, Huppertz B. Placenta and maternal endothelium during preeclampsia: Disruption of the glycocalyx explains increased inositol phosphoglycans and angiogenic factors in maternal blood. J Reprod Immunol. 2023;160:104161.
Hansen DN, Odgaard HS, Uldbjerg N, Sinding M, Sørensen A. Screening for small-for-gestational-age fetuses. Acta Obstet Gynecol Scand. 2020;99:503–9.
Rovas A, Osiaevi I, Buscher K, Sackarnd J, Tepasse PR, Fobker M, et al. Microvascular dysfunction in COVID-19: the MYSTIC study. Angiogenesis. 2021;24:145–57.
Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, Muiesan ML, et al. European Society of Hypertension clinical practice guidelines for the management of arterial hypertension. Eur J Intern Med. 2024(e-pub ahead of print 2024/06/25; https://doi.org/10.1016/j.ejim.2024.05.033).
Palatini P, Kollias A, Saladini F, Asmar R, Bilo G, Kyriakoulis KG, et al. Assessment and management of exaggerated blood pressure response to standing and orthostatic hypertension: consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2024;42:939–47.
Chow S-C SJ, Wang H. Sample size calculations in clinical research. 2nd ed. Boca Raton: Chapman & Hall/CRC. 2008.
Weissgerber TL, Garcia-Valencia O, Milic NM, Codsi E, Cubro H, Nath MC, et al. Early onset preeclampsia is associated with glycocalyx degradation and reduced microvascular perfusion. J Am Heart Assoc. 2019;8:e010647.
Rolnik DL, Wright D, Poon LC, O’Gorman N, Syngelaki A, de Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613–22.
Inversetti A, Pivato CA, Cristodoro M, Latini AC, Condorelli G, Di Simone N, et al. Update on long-term cardiovascular risk after pre-eclampsia: a systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes. 2024;10:4–13.
D’Souza AW, Hissen SL, Okada Y, Jarvis SS, Washio T, Akins JD, et al. Differential regulation of sympathetic neural burst frequency and amplitude throughout normal pregnancy: a longitudinal study. Am J Physiol Regul Integr Comp Physiol. 2023;324:R249–r59.
Catov JM, Muldoon MF, Gandley RE, Brands J, Hauspurg A, Hubel CA, et al. Maternal vascular lesions in the placenta predict vascular impairments a decade after delivery. Hypertension. 2022;79:424–34.
George K, Poudel P, Chalasani R, Goonathilake MR, Waqar S, George S, et al. A systematic review of maternal serum syndecan-1 and preeclampsia. Cureus. 2022;14:e25794.
Carlberg N, Cluver C, Hesse C, Thörn SE, Gandley R, Damén T, et al. Circulating concentrations of glycocalyx degradation products in preeclampsia. Front Physiol. 2022;13:1022770.
Mugerli S, Zupančič D, Rok R, Lučovnik M. Transmission electron microscopy demonstration of reduced endothelial glycocalyx in severe preeclampsia. Placenta. 2022;126:64–9.
Koeppen BM SB. Berne and Levy physiology, 6th edn. Elsevier Inc, (New York. 2008).
Papaioannou TG, Georgiopoulos G, Stamatelopoulos KS, Protogerou AD, Alexandraki KI, Argyris A, et al. Blood pressure variability within a single visit and all-cause mortality. Neth J Med. 2020;78:175–82.
Grassi G, Seravalle G, Maloberti A, Facchetti R, Cuspidi C, Bombelli M, et al. Within-visit BP variability, cardiovascular risk factors, and BP control in central and eastern Europe: findings from the BP-CARE study. J Hypertens. 2015;33:2250–6.
Wilson MG, Bone JN, Mistry HD, Slade LJ, Singer J, von Dadelszen P, et al. Blood pressure and heart rate variability and the impact on pregnancy outcomes: a systematic review. J Am Heart Assoc. 2024;13:e032636.
Piani F, Degli Esposti D, Agnoletti D, Borghi C. Does a multidisciplinary team involving internists specialized in hypertension and obstetric medicine improve pregnancy outcomes? Eur J Intern Med. 2023 (e-pub ahead of print 2023/08/23; https://doi.org/10.1016/j.ejim.2023.08.017).
Hameed AB, Tarsa M, Graves CR, Grodzinsky A, Thiel De Bocanegra H, Wolfe DS. Universal cardiovascular disease risk assessment in pregnancy: call to action. JACC Adv Expert Panel JACC Adv 2024;3:101055.
Acknowledgements
The authors are grateful to all the Study participants. Authors gratefully acknowledge the University of Bologna for providing part of the equipment essential for completing this work.
Funding
F.P. was supported by the International Grant “Alberto Zanchetti” of the Italian Society of Hypertension (SIIA). The study was also supported by the Swedish Research Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest related to this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jälmby, M., Edvinsson, C., Lykou, D. et al. Long-term microvascular and blood pressure dysregulation after Preeclampsia. Hypertens Res 48, 1972–1982 (2025). https://doi.org/10.1038/s41440-025-02176-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02176-1
Keywords
This article is cited by
-
Response to Habibi et al. on ‘Long-term blood pressure dysregulation after preeclampsia’: toward integrated vascular profiling
Hypertension Research (2025)
-
Are all vessels the same? Rethinking vascular heterogeneity across vessel types and sizes
Hypertension Research (2025)
-
Long-term blood pressure dysregulation after preeclampsia
Hypertension Research (2025)
-
Vascular injury as a driver of heterogeneous hypertensive nephrosclerosis: insights from preeclampsia
Hypertension Research (2025)
-
Vessel-size specific endothelial glycocalyx damage and renal microvasculature: implications from preeclampsia follow-up studies
Hypertension Research (2025)