Abstract
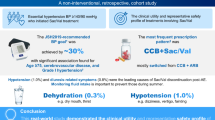
Although renin-angiotensin system (RAS) inhibitors and calcium channel blockers are widely used to treat hypertension in Japan, <10% of patients use thiazides. This study aimed to evaluate differences in the efficacy and safety of sacubitril/valsartan and thiazide diuretics. Patients with poor blood pressure (BP) control, despite combination treatment with RAS inhibitors and calcium channel blockers, were included in the study. Patients treated with thiazides (THZ group, n = 306) and those who switched from RAS inhibitors to sacubitril/valsartan (SacVal group, n = 433) were compared. Propensity score analysis with inverse probability weighting was performed. A significantly higher target BP achievement rate was observed in the SacVal group than in the THZ group (4 months, 37% vs. 26%, p < 0.001). In a general linear mixed model, significant decreases in office and home BP were observed in both groups (p < 0.001); however, no significant interaction effects were observed between the drug type and time course. Discontinuation of the treatment by adverse events was significantly more frequent in THZ group (10%) than in SacVal group (3%), with a hazard ratio [95% confidence interval] of 3.47 [1.78, 6.76] (p < 0.001). In the model using the propensity score, compared with THZ group, significantly lower levels of office and home systolic BP, uric acid, glycated hemoglobin A1c, and higher levels of eGFR were observed in SacVal group (p = 0.04, 0.002, <0.001, 0.01, and 0.02, respectively). In conclusion, comparable BP reduction and positive effects on metabolic parameters were observed with sacubitril/valsartan treatment, with better treatment tolerability than thiazide diuretics.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available from the Review Board of Kanagawa Medical Association, Kanagawa Prefecture to investigators bound by confidential agreements. Contact details: Kazuo Kobayashi Kazuo Kobayashi, M.D., Ph.D, Committee of Hypertension and Kidney disease, Kanagawa Physicians Association, Yokohama, Kanagawa Prefecture, Japan, E-mail: k-taishi@xc4.so-net.ne.jp.
References
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Zhou B, Danaei G, Stevens GA, Bixby H, Taddei C, Carrillo-Larco RM, et al. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639–51.
Hatori N, Sato K, Miyakawa M, Mitani K, Miyajima M, Yuasa S, et al. The current status of blood pressure control among patients with hypertension: a survey of actual clinical practice. J Nippon Med Sch. 2012;79:69–78.
Hatori N, Sakai H, Sato K, Mitani K, Miyajima M, Yuasa S, et al. Changes in blood-pressure control among patients with hypertension from 2008 through 2011: surveys of actual clinical practice. J Nippon Med Sch. 2014;81:258–63.
Hatori N, Sakai H, Sato K, Miyajima M, Yuasa S, Kuboshima S, et al. A survey of actual clinical practice concerning blood pressure control among patients with hypertension in Kanagawa 2014. J Nippon Med Sch. 2016;83:188–95.
Kobayashi KCK, Hatori N, Furuki T, Sakai H, Miyakawa M, Asayama K, et al. Cross-sectional survey of hypertension management in clinical practice in Japan: The Kanagawa Hypertension Study 2021 conducted in collaboration with Japan Medical Association Database of Clinical Medicine. Hypertens Res. 2023;46:2447–59.
Ministry of Health LaW. The National Health and Nutrition Survey in Japan, 2018. 2020; https://www.mhlw.go.jp/content/001066884.pdf:45.
McMurray JJV, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381:1609–20.
Bauersachs J. Heart failure drug treatment: the fantastic four. Eur Heart J. 2021;42:681–3.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Sumida K, Nadkarni GN, Grams ME, Sang Y, Ballew SH, Coresh J, et al. Conversion of urine protein-creatinine ratio or urine dipstick protein to urine albumin-creatinine ratio for use in chronic kidney disease screening and prognosis: an individual participant-based meta-analysis. Ann Intern Med. 2020;173:426–35.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons; 1987.
Rakugi H, Kario K, Yamaguchi M, Sasajima T, Gotou H, Zhang J. Efficacy of sacubitril/valsartan versus olmesartan in Japanese patients with essential hypertension: a randomized, double-blind, multicenter study. Hypertens Res. 2022;45:824–33.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. Hypertension. 2008;51:1403–19.
Group AOaCftACR. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–97.
Rahman M, Ford CE, Cutler JA, Davis BR, Piller LB, Whelton PK, et al. Long-term renal and cardiovascular outcomes in Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) participants by baseline estimated GFR. Clin J Am Soc Nephrol. 2012;7:989–1002.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
Group PC. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41.
Group TSR. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Mitsuno R, Uchiyama K, Nakayama T, Takahashi R, Yoshimoto N, Yamaguchi S, et al. Comparison of the effects of angiotensin receptor-neprilysin inhibitors and thiazide diuretic/renin-angiotensin system inhibitor combination therapy in hypertensive patients: a retrospective cohort study. J Hum Hypertens. 2023;37:1049–55.
Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427.
Bozkurt B, Nair AP, Misra A, Scott CZ, Mahar JH, Fedson S. Neprilysin Inhibitors in Heart Failure. JACC Basic Transl Sci. 2023;8:88–105.
Seferovic JP, Claggett B, Seidelmann SB, Seely EW, Packer M, Zile MR, et al. Effect of sacubitril/valsartan versus enalapril on glycaemic control in patients with heart failure and diabetes: a post-hoc analysis from the PARADIGM-HF trial. Lancet Diab Endocrinol. 2017;5:333–40.
Wijkman MO, Claggett B, Vaduganathan M, Cunningham JW, Rørth R, Jackson A, et al. Effects of sacubitril/valsartan on glycemia in patients with diabetes and heart failure: the PARAGON-HF and PARADIGM-HF trials. Cardiovasc Diabetol. 2022;21:110.
Esser N, Zraika S. Neprilysin inhibition: a new therapeutic option for type 2 diabetes? Diabetologia. 2019;62:1113–22.
Packer M, Claggett B, Lefkowitz MP, McMurray JJV, Rouleau JL, Solomon SD, et al. Effect of neprilysin inhibition on renal function in patients with type 2 diabetes and chronic heart failure who are receiving target doses of inhibitors of the renin-angiotensin system: a secondary analysis of the PARADIGM-HF trial. Lancet Diab Endocrinol. 2018;6:547–54.
Voors AA, Gori M, Liu LCY, Claggett B, Zile MR, Pieske B, et al. Renal effects of the angiotensin receptor neprilysin inhibitor LCZ696 in patients with heart failure and preserved ejection fraction. Eur J Heart Fail. 2015;17:510–7.
Kimura K, Hirata Y, Nanba S, Tojo A, Matsuoka H, Sugimoto T. Effects of atrial natriuretic peptide on renal arterioles: morphometric analysis using microvascular casts. Am J Physiol. 1990;259:F936–944.
Appel RG, Wang J, Simonson MS, Dunn MJ. A mechanism by which atrial natriuretic factor mediates its glomerular actions. Am J Physiol. 1986;251:F1036–1042.
Pieske B, Wachter R, Shah SJ, Baldridge A, Szeczoedy P, Ibram G, et al. Effect of sacubitril/valsartan vs standard medical therapies on plasma NT-proBNP concentration and submaximal exercise capacity in patients with heart failure and preserved ejection fraction: the PARALLAX randomized clinical trial. JAMA. 2021;326:1919–29.
Blacklock CL, Hirst JA, Taylor KS, Stevens RJ, Roberts NW, Farmer AJ. Evidence for a dose effect of renin-angiotensin system inhibition on progression of microalbuminuria in Type 2 diabetes: a meta-analysis. Diabet Med. 2011;28:1182–7.
Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-head comparisons of hydrochlorothiazide with indapamide and chlorthalidone. Hypertension. 2015;65:1041–6.
Dorsch MP, Gillespie BW, Erickson SR, Bleske BE, Weder AB. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57:689–94.
Ishani A, Cushman WC, Leatherman SM, Lew RA, Woods P, Glassman PA, et al. Chlorthalidone vs. hydrochlorothiazide for hypertension–cardiovascular events. N Engl J Med. 2022;387:2401–10.
Kario K, Rakugi H, Yarimizu D, Morita Y, Eguchi S, Iekushi K. Twenty‐four‐hour blood pressure‐lowering efficacy of sacubitril/valsartan versus olmesartan in Japanese patients with essential hypertension based on nocturnal blood pressure dipping status: a post hoc analysis of data from a randomized, double‐blind mult. J Am Heart Assoc. 2023;12:e027612.
Madley-Dowd P, Hughes R, Tilling K, Heron J. The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol. 2019;110:63–73.
Acknowledgements
We are grateful to all participants and acknowledge the support of the members of the Kanagawa Physicians Association, especially Noriyuki Asaba, Motohiko Okabe, Masashi Otsuka, and Kazuyoshi Sato, who contributed considerably to data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HW has received research supports from AstraZeneca, Otsuka Pharmaceutical, and Kaneka Corporation, and honoraria from AstraZeneca, Otsuka Pharmaceutical, Kaneka Corporation, Kyowa Kirin, Sanwa Kagaku, Chugai Pharma, Kowa, Otsuka Pharmaceutical, Novartes, Mitsubishi-Tanabe Pharma, Bayer, and Daiichi-Sankyo Pharma. MT received lecture fees from Boehringer Ingelheim, Eli Lilly, Novo Nordisk, Sumitomo, and Mitsubishi Tanabe and received subsidies from Super Light Water, TAKAGI, Roche DC, and LifeScan. KT has received honoraria/lecture fee from AstraZeneca, Novartes, Bayer, Otsuka Pharmaceutical, Boehringer Ingelheim, Fuji Pharma, Kyowa Kirin, Ono Pharmaceutical, Sanwa Kagaku, Mochida Pharmaceutical, Kowa, Eli Lilly, Novo Nordisk, commissioned clinical trials, contract research and joint research funding: AstraZeneca, Bayer, Novartis, Chinook, Otsuka Medical Devices, Novo Nordisk, Terumo, Variatris, and Kowa, and, Scholarship donations: Otsuka Pharmaceutical, Bayer, Mochida Pharmaceutical, and Boehringer Ingelheim.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kobayashi, K., Sotozawa, M., Chin, K. et al. Comparison between sacubitril/valsartan and thiazide diuretics among patients with uncontrolled hypertension in Japan. Hypertens Res 48, 2058–2071 (2025). https://doi.org/10.1038/s41440-025-02236-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02236-6
Keywords
This article is cited by
-
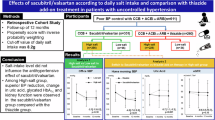
Effects of sacubitril/valsartan according to daily salt intake and comparison with thiazide add-on treatment in patients with uncontrolled hypertension
Hypertension Research (2025)
-
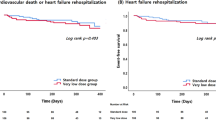
Comparison of renal effects between sacubitril/valsartan and thiazide diuretics among patients with uncontrolled hypertension and chronic kidney disease in Japan
Clinical and Experimental Nephrology (2025)