Abstract
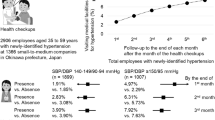
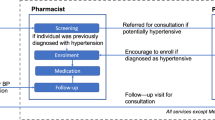
This longitudinal study investigated whether a worksite healthcare policy of making time for medical visits (exposure factor) facilitated attendance (outcome) at these visits for treatment of newly identified hypertension after a health checkup. The study included employees at small-to-medium companies in Okinawa, Japan, who had a systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg, no history of hypertension in the last year, and were not taking antihypertensive medication. Pre-existing data on worksite characteristics, employees’ health checkups, and health insurance claims were collected. A multilevel logistic regression model was used to calculate the odds ratio for the worksite group providing time to attend the medical visit, with the worksite group not providing this time acting as the reference. In the 2906 participants with newly identified hypertension employed at 1366 worksites, the cumulative incidence of interest increased gradually with longer follow-up in both groups, although the incidence was higher in the group providing time for the visit. After adjustment for potential confounding factors, the odds ratios (95% confidence interval) for visits by the end of the 4th, 5th, and 6th months after the health checkup in the group with time for a medical visit were 1.80 (1.13–2.86), 1.72 (1.10–2.70), and 1.55 (0.99–2.45), respectively. Similar patterns were observed for every stratum of company size, business category, and healthcare administrator status. These results indicate that a worksite making time for a visit to a medical facility was associated with increased visits by employees with newly identified hypertension at a health checkup.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Asia Pacific Cohort Studies Collaboration. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003;21:707–16.
Fujiyoshi A, Ohkubo T, Miura K, Murakami Y, Nagasawa SY, Okamura T, et al. Observational Cohorts in Japan (EPOCH-JAPAN) Research Group. Blood pressure categories and long-term risk of cardiovascular disease according to age group in Japanese men and women. Hypertens Res. 2012;35:947–53.
Lawes CM, Vander Hoorn S, Rodgers A. International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Kuriyama A, Takahashi Y, Tsujimura Y, Miyazaki K, Satoh T, Ikeda S, et al. Predicting failure to follow-up screened high blood pressure in Japan: a cohort study. J Public Health. 2015;37:498–505.
Fukuma S, Ikenoue T, Saito Y, Yamada Y, Saigusa Y, Misumi T, et al. Lack of a bridge between screening and medical management for hypertension: health screening cohort in Japan. BMC Public Health. 2020;20:1419.
Kudaka S, Sakima A, Nakamura K. Healthcare administrators and hypertension at small-to-medium worksites in Okinawa, Japan. Hypertens Res. 2025;48:168–79.
Oshio T, Sugiyama K, Ashida T. Effect of social activities on health checkups and recommended doctor visits: a fixed-effects analysis in Japan. Ind Health. 2023;61:446–54.
Cheng SY, Li MC, Chia SL, Huang KC, Chiu TY, Chan DC, et al. Factors affecting compliance with confirmatory colonoscopy after a positive fecal immunochemical test in a national colorectal screening program. Cancer. 2018;124:907–15.
Aono Y, Aisaka A, Gohno M, Hida T, Shimizu T. Visiting a doctor by individuals who need medical diagnosis after screening and kinds of screening. Occup Health J. 2000;23:43–9. (in Japanese)
Okamura T, Sugiyama D, Tanaka T, Dohi S. Worksite wellness for the primary and secondary prevention of cardiovascular disease in Japan: the current delivery system and future directions. Prog Cardiovasc Dis. 2014;56:515–21.
Tsuda K, Tsutsumi A, Kawakami N. Work-related factors associated with visiting a doctor for a medical diagnosis after a worksite screening for diabetes mellitus in Japanese male employees. J Occup Health. 2004;46:374–81.
Goto E, Ishikawa H, Okuhara T, Kato M, Okada M, Kiuchi T. Factors associated with adherence to recommendations to visit a physician after annual health checkups among Japanese employees: a cross-sectional observational study. Ind Health. 2018;56:155–9.
Kadota A, Okuda N, Ohkubo T, Okamura T, Nishi N, Ueshima H, et al. The National Integrated Project for Prospective Observation of Non-communicable Disease and its Trends in the Aged 2010 (NIPPON DATA2010): objectives, design, and population characteristics. J Epidemiol. 2018;28:S2–S9.
Ministry of Health, Labour and Welfare of Japan. An outline of the Japanese Medical System. https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01_eng.pdf. Accessed 1 Feb 2025.
Kohro T, Furui Y, Mitsutake N, Fujii R, Morita H, Oku S, et al. The Japanese national health screening and intervention program aimed at preventing worsening of the metabolic syndrome. Int Heart J. 2008;49:193–203.
Matsuzawa Y, Funahashi T, Nakamura T. The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism. J Atheroscler Thromb. 2011;18:629–39.
Ministry of Health, Labour and Welfare of Japan. The standard classification of business category for employees’ health insurance and employees’ pension insurance. https://www.mhlw.go.jp/web/t_doc?dataId=00tc6845&dataType=1&pageNo=1 (in Japanese). Accessed 1 Feb 2025.
Ministry of Health, Labour and Welfare of Japan. The Basic Guideline for Health Checkups and Healthcare Advice with a Particular Focus on the Metabolic Syndrome (edition of year 2018). https://www.mhlw.go.jp/content/10900000/000496784.pdf (in Japanese). Accessed 1 Feb 2025.
Tanno K, Okamura T, Ohsawa M, Onoda T, Itai K, Sakata K, et al. Comparison of low-density lipoprotein cholesterol concentrations measured by a direct homogeneous assay and by the Friedewald formula in a large community population. Clin Chim Acta. 2010;411:1774–80.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). https://icd.who.int/browse10/2019/en. Accessed 1 Feb 2025.
Yamaguchi N, Ohkubo T, Funatani F, Yamamura J, Takahashi K, Nakamura R. A prospective study of access to medical services following a community-based screening program. Jpn J Public Health. 1990;37:281–7. (in Japanese)
Goto E, Ishikawa H, Okuhara T, Okada H, Tsunezumi A, Kagawa Y, et al. Factors associated with adherence to recommendations for medical visits following annual health checkups among Japanese employees: A prospective cohort study. Prev Med Rep. 2023;37:102565.
Lusk SL, Raymond DM 3rd. Impacting health through the worksite. Nurs Clin North Am. 2002;37:247–56.
Morioka I, Terashita H, Miyashita K, Ikuta Z, Takeshita T, Fujiyoshi A, et al. Support for a balance between work schedules and treatment regimens among workers with illness: a questionnaire survey focusing on company size in Wakayama Prefecture, Japan. Sangyo Eiseigaku Zasshi. 2023;65:28–40. (in Japanese)
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80. (Errata: Lancet 2022;399:520)
The Japan Institute for Labour Policy and Training. Databook of International Labour Statistics 2024. https://www.jil.go.jp/kokunai/statistics/databook/2024/documents/Databook2024.pdf (in Japanese; but tables are available in English). Accessed 1 Feb 2025.
Ogami A. Current status of health examinations for workers in East Asia. Health Eval Promot. 2020;47:323–8. (in Japanese)
Acknowledgements
This study was commissioned by the Okinawa Branch of the Japan Health Insurance Association without financial support. We express special gratitude to the Okinawa Branch that provided the study data.
Author information
Authors and Affiliations
Contributions
KN and SK were involved in the fundamental design of the study and data acquisition, while KN conceived the concept of the current report and performed the statistical analysis. All the authors interpreted the results. KN drafted the manuscript, and SK and AS made critical revisions to the manuscript. KN supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakamura, K., Kudaka, S. & Sakima, A. Making time at a worksite increased medical visits by employees with hypertension at small-to-medium worksites in Okinawa, Japan. Hypertens Res 48, 2584–2594 (2025). https://doi.org/10.1038/s41440-025-02316-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02316-7