Abstract
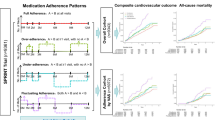
Non-adherence to antihypertensive therapy remains a major barrier to blood pressure (BP) control globally. The behavioural distinction between intentional (INA) and unintentional non-adherence (UNA) is underexplored in low- and middle-income countries. We aimed to validate the Spanish MMAS-8, identify adherence–complexity phenotypes, and assess the mediating role of adherence between regimen complexity and BP control. In this multicenter, cross-sectional study (2022–2024), 1144 hypertensive patients from Argentina were evaluated. Adherence was assessed using the Spanish MMAS-8. Psychometric validation included Cronbach’s alpha and principal component analysis. INA and UNA were classified by domain-based response patterns. K-means clustering was applied to MMAS-8 items and regimen complexity (number of drugs, daily doses). Mediation analysis tested the indirect effect of adherence. The MMAS-8 showed acceptable reliability (α = 0.78) and a unidimensional structure. Full adherence was observed in 41.1%. Among non-adherent patients, 38.5% were INA, 33.6% UNA, and 27.9% mixed. Four phenotypes were identified: (1) high adherence/low complexity; (2) very low adherence/simple regimens; (3) moderate adherence/intermediate complexity; (4) low adherence/high complexity. Adherence significantly mediated the effect of complexity on BP control (β = 0.004; p < 0.001), while the direct effect was non-significant. Compared with phenotype 1, phenotype 2 showed 58% lower odds of control (OR 0.42; 95% CI 0.29–0.61) and phenotype 4 showed 32% lower odds (OR 0.68; 95% CI 0.49–0.94). The Spanish MMAS-8 is valid for this population. Adherence–complexity phenotypes reflect structural and behavioural barriers. Tailored interventions should address INA and UNA using adherence profiling, fixed-dose combinations, and social support.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Risk NCD. Factor Collaboration (NCD‑RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis. Lancet. 2021;398:957–80.
Gagliardi J, Miranda N, Calandrelli M, Nasca R, Giorgi M, Gutierrez L, et al. Prevalence, awareness, treatment and control of hypertension in Argentina: results of the RENATA‑2 study. J Hum Hypertens. 2018;32:773–80.
Delucchi AM, Majul CR, Vicario A, Cerezo GH, Fábregues G, Marín MJ, et al. National Registry of Hypertension (RENATA‑1): epidemiological characteristics of hypertension in Argentina. Rev Argent Cardiol. 2017;85:340–6.
Ordúñez P, Campbell N, Giraldo G, Angell S, Lombardi C, Brettler J, et al. Effective approaches to hypertension control in Latin America and the Caribbean, 2014-20: a review. Rev Panam Salud Publica. 2022;46:e75.
Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis of 42 trials. Am J Med. 2009;122:290–300.
Salam A, Kanukula R, Atkins E, Wang X, Islam S, Kishore SP, et al. Efficacy and safety of dual or multiple fixed‑dose combination therapies for hypertension. JAMA. 2019;322:2211–9.
Thom S, Poulter N, Field J, Patel A, Burnier M, Prabhakaran D, et al. Effects of a fixed‑dose combination strategy on adherence and blood pressure: the UMPIRE study. Lancet. 2013;381:1413–22.
Peixoto AJ, Krieger EM, Marín MJ, Alfie J, Gutierrez L, Fábregues G, et al. Joint consensus on fixed‑dose combinations in hypertension. Rev Fed Arg Cardiol. 2021;50:155–9.
Rojas C, Toledo A, Martín‑Sánchez G, Espeche W, Salazar MR, Aizpurúa M, et al. Evaluación de acceso a medicamentos antihipertensivos en Argentina. Salud Colectiva. 2022;18:e3895.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–54.
Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66.
Romero C, Marín MJ, Alfie J, Gutierrez L, Acevedo M, Fábregues G, et al. Validación de escalas de adherencia en pacientes hipertensos: revisión sistemática. Hipertens Riesgo Vasc. 2022;39:20–28.
Renna N, Salazar MR, Martín-Sánchez G, Toledo A, Gagliardi J, Bendersky M, et al. Adherencia, combinaciones fijas y factores socioeconómicos en hipertensión: hallazgos del estudio VATAHTA. Rev Fed Arg Cardiol. 2024;51:18–25.
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharm. 2012;73:691–705.
Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9:11–23.
Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: a review from the patient's perspective. Ther Clin Risk Manag. 2008;4:269–86.
Cooper C, Booth A, Gill P, Lacey T. A taxonomy of adherence interventions: a systematic review and synthesis of meta-analyses. Patient Educ Couns. 2021;104:2990–3002.
World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: WHO; 2003.
Castellano JM, Sanz G, Peñalvo JL, Bansilal S, Fernández-Ortiz A, Alvarez L, et al. A polypill strategy to improve adherence: results from the FOCUS trial. J Am Coll Cardiol. 2014;64:2071–82.
Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124:1124–40.
Kronish IM, Ye S. Adherence to cardiovascular medications: lessons learned and future directions. Prog Cardiovasc Dis. 2013;55:590–600.
Chow CK, Redfern J, Hillis GS, Thakkar J, Santo K, Hackett ML, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314:1255–63.
Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296:2563–71.
Marcolino MS, Oliveira JAQ, Ribeiro ALP, Alkmim MBM, Aquino EC, Côrtes MF, et al. Telemedicine application in the care of diabetes patients: systematic review and meta-analysis. PLoS One. 2013;8:e79246.
Ihm SH, Kim KI, Kim CH, Cho EJ, Kim M, Yoo B, et al. Blood pressure control and medication adherence among patients with hypertension and cognitive impairment in Korea. Hypertens Res. 2019;42:1545–53.
Al-Ghurair SA, Hughes CA, Simpson SH, Guirguis LM. A systematic review of patient self-reported barriers of adherence to antihypertensive medications. Curr Hypertens Rep. 2012;14:431–41.
Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;2014:CD000011.
Menckeberg TT, Bouvy ML, Bracke M, Kaptein AA, Leufkens HG, Raaijmakers JA, et al. Beliefs about medicines predict refill adherence to inhaled corticosteroids. J Psychosom Res. 2008;64:47–54.
Poon EG, Keohane CA, Yoon CS, Ditmore M, Bane A, Levtzion-Korach O, et al. Effect of bar-code technology on the safety of medication administration. N Engl J Med. 2010;362:1698–707.
Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190–6.
Patel P, Ordunez P, DiPette D, Escobar MC, Hassell T, Wyss R, et al. Improved blood pressure control to reduce cardiovascular disease morbidity and mortality: the Standardized Hypertension Treatment and Prevention Project. J Clin Hypertens. 2016;18:1284–94.
Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8:e016982.
Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. 2014;20:58–65.
Omboni S, Caserini M. Telemedicine and M-health in hypertension management: technologies. Appl Clin Evid High Blood Press Cardiovasc Prev. 2019;26:359–66.
Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Ross H, Easty A, et al. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension. 2012;60:51–57.
Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended versus attended blood pressure measurement: implications for clinical practice. Curr Hypertens Rep. 2014;16:508.
Redon J, Olsen MH, Cooper RS, Zurriaga O, Martinez-Beneito MA, Laurent S, et al. Hypertension in patients with diabetes: global perspectives and current management. Cardiovasc Diabetol. 2006;5:26.
Ribeiro AG, Ribeiro SM, Dias CM, Franceschini SD, Priore SE, Peluzio MCG. Nonadherence to antihypertensive medication: validation of a new tool in a Brazilian population. Arq Bras Cardiol. 2014;103:389–98.
Wald DS, Morris JK, Wald NJ. Randomized polypill crossover trial in people aged 50 and over. PLoS One. 2012;7:e41297.
Horne R, Weinman J, Barber N, Elliott RA, Morgan M. Concordance, adherence and compliance in medicine taking. London: NCCSDO; 2005.
Bailey SC, Oramasionwu CU, Wolf MS. Rethinking adherence: a health literacy–informed model of medication self-management. J Health Commun. 2013;18:20–30.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis. J Hypertens. 2014;32:1921–34.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–50.
Kronish IM, Rieckmann N, Halm EA, Shimbo D. Chronic disease self-management and adherence to antihypertensive medication in older adults: a population-based survey. Med Care. 2009;47:521–6.
Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: response to authors. J Clin Epidemiol. 2011;64:255–7.
Niiranen TJ, Johansson JK, Reunanen A, Jula AM. Optimal threshold for diagnosing hypertension with ambulatory blood pressure monitoring: predictive value for cardiovascular events. Hypertension. 2013;62:698–703.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Morisky Medication Adherence Scale (MMAS) is copyrighted by Adherence, which licenses its use for research and commercial purposes. PM oversees the implementation and licensing of the scale. Any fees collected support the advancement of adherence research and patient-centred interventions. This financial interest has been disclosed and managed in accordance with institutional guidelines. The authors affirm that these relationships have not influenced the design, conduct, or reporting of this study, and that the scientific integrity of the work remains uncompromised.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Renna, N.F., Ramirez, J.M., Arrupe, M.F. et al. Intentional and unintentional non-adherence in hypertension: psychometric validation, adherence–complexity phenotyping and causal mediation analysis from the VATAHTA Study. Hypertens Res (2025). https://doi.org/10.1038/s41440-025-02427-1
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41440-025-02427-1