Abstract
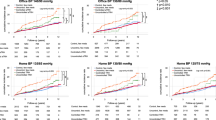
Chronic kidney disease (CKD) is a major risk factor for cardiovascular events, and controlling blood pressure (BP) is essential for reducing this risk in CKD patients. Although office BP is the standard for BP control in CKD, home BP monitoring more precisely predicts cardiovascular outcomes, especially across Kidney Disease: Improving Global Outcomes (KDIGO) risk categories. This study evaluated the differential impact of office and home BP control on cardiovascular event rates across KDIGO risk levels. Data from 4264 participants in the Japan Morning Surge-Home Blood Pressure study were analyzed. Participants were stratified by KDIGO risk and classified by BP control using office (<140/90 mmHg) and home (<135/85 mmHg) thresholds. The primary outcome was a composite of cardiovascular events, including myocardial infarction, stroke, heart failure hospitalization, and cardiovascular death. Cox proportional hazards models evaluated associations between BP control and cardiovascular risk within KDIGO strata. Over a median 6.2-year follow-up, 262 cardiovascular events occurred. In the high/very high KDIGO group, controlled home BP was associated with a lower event rate (10.3 vs. 31.8 per 1000 person-years; HR = 0.38, 95% CI 0.20–0.70; P < 0.001). The interaction between home BP and KDIGO risk was significant (P = 0.024). Office BP control showed no significant association with cardiovascular outcomes. Subgroup analysis revealed that morning and evening home BP control predicted reduced cardiovascular risk in high-risk individuals. Home BP control, not office BP control, was associated with reduced cardiovascular risk, especially in individuals with high KDIGO risk. These findings support integrating home BP monitoring into CKD-related hypertension care.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–81.
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJL, Mann JF, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382:339–52.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150.
Xu Y, Li M, Qin G, Lu J, Yan L, Xu M, et al. Cardiovascular risk based on ASCVD and KDIGO categories in Chinese adults: a nationwide, population-based, prospective cohort study. J Am Soc Nephrol. 2021;32:927–37.
Maruyama S, Tanaka T, Akiyama H, Hoshino M, Inokuchi S, Kaneko S, et al. Cardiovascular, renal and mortality risk by the KDIGO heatmap in Japan. Clin Kidney J. 2024;17:sfae228. https://doi.org/10.1093/ckj/sfae228.
Matsushita K, Coresh J, Sang Y, Chalmers J, Fox C, Guallar E, et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 2015;3:514–25.
Tada K, Fujiwara A, Sugano N, Hayashi K, Sakima A, Takami Y, et al. Evaluating blood pressure targets in chronic kidney disease: a systematic review and meta-analysis. Hypertens Res. 2025;48:2358–67.
Nagata D, Hishida E. Elucidating the complex interplay between chronic kidney disease and hypertension. Hypertens Res. 2024;47:3409–22.
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2021;99:1–87.
Ku E, Lee BJ, Wei J, Weir MR. Hypertension in CKD: core curriculum 2019. Am J Kidney Dis. 2019;74:120–31.
Kollias A, Kyriakoulis KG, Komnianou A, Stathopoulou P, Stergiou GS. Prognostic value of home versus ambulatory blood pressure monitoring: a systematic review and meta-analysis of outcome studies. J Hypertens. 2024;42:385–92.
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan Morning Surge-Home blood pressure Study. Hypertension. 2016;68:54–61.
Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, et al. Japanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res. 2003;26:771–82.
Kario K, Kanegae H, Okawara Y, Tomitani N, Hoshide S. Home blood pressure variability risk prediction score for cardiovascular disease using data from the J-HOP Study. Hypertension. 2024;81:2173–80.
Narita K, Hoshide S, Kario K. Difference between morning and evening home blood pressure and cardiovascular events: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Hypertens Res. 2021;44:1597–605.
Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension. 2010;55:1346–51.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30:449–56.
Bobrie G, Genes N, Vaur L, et al. Masked hypertension: a systematic review. J Hypertens. 2008;26:1715–20.
Burnier M, Damianaki A. Hypertension as cardiovascular risk factor in chronic kidney disease. Circ Res. 2023;132:1050–63.
Wu S, Li M, Lu J, Tang X, Wang G, Zheng R, et al. Blood pressure levels, cardiovascular events, and renal outcomes in chronic kidney disease without antihypertensive therapy: a nationwide population-based cohort study. Hypertension. 2023;80:640–9.
Ninomiya T, Perkovic V, Turnbull F, Neal B, Barzi F, Cass A, et al. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ. 2013;347:f5680.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Perkovic V, Ninomiya T, Arima H, Gallagher M, Jardine M, Cass A, et al. Chronic kidney disease, cardiovascular events, and the effects of perindopril-based blood pressure lowering: data from the PROGRESS study. J Am Soc Nephrol. 2007;18:2766–72.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Zullig LL, Melnyk SD, Goldstein K, Shaw RJ, Bosworth HB. The role of home blood pressure telemonitoring in managing hypertensive populations. Curr Hypertens Rep. 2013;15:346–55.
Willis HA, Neblett EW. Developing culturally-adapted mobile mental health interventions: a mixed methods approach. Mhealth. 2023;9:1 https://doi.org/10.21037/mhealth-22-19.
Sarkar A, Nwokocha C, Nash SG, Grigoryan L. Empowering low-income patients with home blood pressure monitors to improve hypertension control. J Am Board Fam Med. 2024;37:187–95.
Sánchez-Ospina D, Mas-Fontao S, Martin Palencia M, Hijazi Prieto B, Gómez Sánchez C, Paredes Carcedo S, et al. Impact of albuminuria screening in primary care on the detection and management of chronic kidney disease: findings from the ONDAAS study. Clin Kidney J. 2025;18:sfaf123. https://doi.org/10.1093/ckj/sfaf123.
Zhang DY, An DW, Yu YL, Melgarejo JD, Boggia J, Martens DS, et al. Ambulatory blood pressure monitoring, European guideline targets, and cardiovascular outcomes: an individual patient data meta-analysis. Eur Heart J. 2025. https://doi.org/10.1093/eurheartj/ehaf220.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hayakawa, M., Hoshide, S., Kanegae, H. et al. Impact of office and home blood pressure control on cardiovascular events in relation to KDIGO risk categories: findings from the J-HOP study. Hypertens Res 49, 350–359 (2026). https://doi.org/10.1038/s41440-025-02429-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02429-z