Abstract
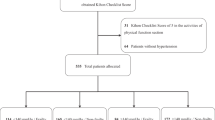
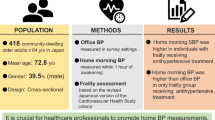
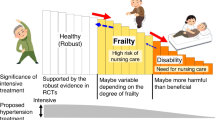
Studies on the effects of blood pressure (BP) control satisfaction and adherence to antihypertensive medication on frailty in older patients with hypertension are limited. We aimed to evaluate the effects of BP control satisfaction and antihypertensive medication adherence on frailty transitions. We obtained routinely collected data from the National Essential Public Health Service Package, involving community-dwelling older patients with hypertension from an administrative district in Shenzhen, China, from 2018 to 2022. BP control satisfaction and antihypertensive medication adherence scores were based on follow-up clinical assessments. The frailty index (FI) was evaluated by annual questionnaires and health examinations. Multi-state models were utilized to estimate the associations between BP control satisfaction and antihypertensive medication adherence scores with frailty transitions. The median age of the 10,391 patients was 70 years (interquartile range: 67–73) at baseline: 5062 (48.7%) were non-frail, 4726 (45.5%) were pre-frail, and 603 (5.8%) were frail. Over a median follow-up of 1.63 years, 5782 transitions were observed, with 2840 (49%) forward and 2942 (51%) backward transitions. High BP control satisfaction was associated with a lower likelihood of transitioning from a non-frail to a pre-frail or frail state. High antihypertensive medication adherence was associated with an increased risk of transitioning from a non-frail to a pre-frail state and impeded frailty reversion from the frail to the pre-frail state. Effective BP control has protective effects against the development of frailty, while antihypertensive medication adherence might have detrimental effects in community-dwelling older patients with hypertension; however, further studies are required to determine this effect.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Hua Q, Fan L, Wang ZW, Li J. 2023 Guideline for the management of hypertension in the elderly population in China. J Geriatr Cardiol. 2024;21:589–630.
Chen X. May Measurement Month 2017-2023 in China. J Hypertens. 2024;42 Suppl 1:e85.
Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019;124:1045–60.
Li X, Lu J, Hu S, Cheng KK, De Maeseneer J, Meng Q, et al. The primary health-care system in China. Lancet. 2017;390:2584–94.
Qin J, Zhang Y, Fridman M, Sweeny K, Zhang L, Lin C, et al. The role of the Basic Public Health Service program in the control of hypertension in China: results from a cross-sectional health service interview survey. PLoS ONE. 2021;16:e0217185.
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–7.
Ho LYW, Cheung DSK, Kwan RYC, Wong ASW, Lai CKY. Factors associated with frailty transition at different follow-up intervals: a scoping review. Geriatr Nurs. 2021;42:555–65.
Liu H, Zhou W, Liu Q, Yu J, Wang C. Global prevalence and factors associated with frailty among community-dwelling older adults with hypertension: a systematic review and meta-analysis. J Nutr Health Aging. 2023;27:1238–47.
Vetrano DL, Palmer KM, Galluzzo L, Giampaoli S, Marengoni A, Bernabei R, et al. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8:e024406.
Anker D, Carmeli C, Zwahlen M, Rodondi N, Santschi V, Henchoz Y, et al. How blood pressure predicts frailty transitions in older adults in a population-based cohort study: a multi-state transition model. Int J Epidemiol. 2022;51:1167–77.
Tian G, Zhou R, Guo X, Li R. Causal effects of blood pressure and the risk of frailty: a bi-directional two-sample Mendelian randomization study. J Hum Hypertens. 2024;38:329–35.
Shen F, Chen J, Yang R, Yang J, Li H. Association between control status of blood pressure and frailty among middle-aged and older adults with hypertension in China: a longitudinal study. BMJ Open. 2022;12:e056395.
Wang Z, Du X, Hua C, Li W, Zhang H, Liu X, et al. The effect of frailty on the efficacy and safety of intensive blood pressure control: a post hoc analysis of the SPRINT trial. Circulation. 2023;148:565–74.
Poulter NR, Borghi C, Parati G, Pathak A, Toli D, Williams B, et al. Medication adherence in hypertension. J Hypertens. 2020;38:579–87.
Baker-Goering MM, Howard DH, Will JC, Beeler Asay GR, Roy K. Association between self-reported hypertension and antihypertensive medication use and cardiovascular disease-related events and expenditures among patients diagnosed with hypertension. Public Health Rep. 2019;134:493–501.
Silva LM, Souza AC, Fhon JRS, Rodrigues RAP. Treatment adherence and frailty syndrome in hypertensive older adults. Rev Esc Enferm USP. 2020;54:e03590.
Jankowska-Polańska B, Dudek K, Szymanska-Chabowska A, Uchmanowicz I. The influence of frailty syndrome on medication adherence among elderly patients with hypertension. Clin Interv Aging. 2016;11:1781–90.
Wang A, Wan J, Zhu L, Chang W, Wen L, Tao X, et al. Frailty and medication adherence among older adult patients with hypertension: a moderated mediation model. Front Public Health. 2023;11:1283416.
Rockwood K, Mitnitski A. Limits to deficit accumulation in elderly people. Mech Ageing Dev. 2006;127:494–6.
Theou O, Haviva C, Wallace L, Searle SD, Rockwood K. How to construct a frailty index from an existing dataset in 10 steps. Age Ageing. 2023;52:afad221.
Pajewski NM, Lenoir K, Wells BJ, Williamson JD, Callahan KE. Frailty screening using the electronic health record within a Medicare accountable care organization. J Gerontol A Biol Sci Med Sci. 2019;74:1771–7.
McKenzie F, Biessy C, Ferrari P, Freisling H, Rinaldi S, Chajès V, et al. Healthy lifestyle and risk of cancer in the European Prospective Investigation Into Cancer and Nutrition Cohort Study. Medicine. 2016;95:e2850.
Jing L, Care TNEPHSPOfMoHiPH, Diseases NCfC, Care NCoHMiPH. National Guidelines for the Prevention, Treatment and Management of Hypertension at the Primary Level (2020 Edition). China Circ Mag. 2021;36:209–20.
Zanchetti A, Thomopoulos C, Parati G. Randomized controlled trials of blood pressure lowering in hypertension: a critical reappraisal. Circ Res. 2015;116:1058–73.
Kang MG, Kim SW, Yoon SJ, Choi JY, Kim KI, Kim CH. Association between Frailty and hypertension prevalence, treatment, and control in the elderly Korean population. Sci Rep. 2017;7:7542.
Yu BY, Hu XM, Matala R, Mo YH, Liu JL, Jin JG, et al. Association between trajectories of systolic blood pressure and frailty outcome in middle-aged and older adults. J Nutr Health Aging. 2024;28:100202.
Carey RM, Moran AE, Whelton PK. Treatment of hypertension: a review. JAMA. 2022;328:1849–61.
Ferrucci L, Cavazzini C, Corsi A, Bartali B, Russo CR, Lauretani F, et al. Biomarkers of frailty in older persons. J Endocrinol Investig. 2002;25:10–5.
Chae CU, Lee RT, Rifai N, Ridker PM. Blood pressure and inflammation in apparently healthy men. Hypertension. 2001;38:399–403.
Hu K, Zhou G, Jiang M, Wei X, Yu J, Liu L, et al. Hypertension treatment in frail older adults: a systematic review and appraisal of guidelines. Drugs Aging. 2023;40:881–93.
Sheppard JP, Koshiaris C, Stevens R, Lay-Flurrie S, Banerjee A, Bellows BK, et al. The association between antihypertensive treatment and serious adverse events by age and frailty: a cohort study. PLoS Med. 2023;20:e1004223.
Rouch L, Rolland Y, Hanon O, Vidal JS, Cestac P, Sallerin B, et al. Blood pressure, antihypertensive drugs, and incident frailty: the Multidomain Alzheimer Preventive Trial (MAPT). Maturitas. 2022;162:8–14.
Nicholson K, Liu W, Fitzpatrick D, Hardacre KA, Roberts S, Salerno J, et al. Prevalence of multimorbidity and polypharmacy among adults and older adults: a systematic review. Lancet Healthy Longev. 2024;5:e287–96.
Inoue T, Matsuoka M, Shinjo T, Tamashiro M, Oba K, Kakazu M, et al. Blood pressure, frailty status, and all-cause mortality in elderly hypertensives; The Nambu Cohort Study. Hypertens Res. 2022;45:146–54.
Pajewski NM, Williamson JD, Applegate WB, Berlowitz DR, Bolin LP, Chertow GM, et al. Characterizing frailty status in the systolic blood pressure intervention trial. J Gerontol A Biol Sci Med Sci. 2016;71:649–55.
Kraut R, Lundby C, Babenko O, Kamal A, Sadowski CA. Antihypertensive medication in frail older adults: a narrative review through a deprescribing lens. Am Heart J Plus Cardiol Res Pract. 2022;17:100166.
Basile G, Catalano A, Mandraffino G, Maltese G, Alibrandi A, Ciancio G, et al. Relationship between blood pressure and frailty in older hypertensive outpatients. Aging Clin Exp Res. 2017;29:1049–53.
Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166:418–23.
Fairhall N, Langron C, Sherrington C, Lord SR, Kurrle SE, Lockwood K, et al. Treating frailty—a practical guide. BMC Med. 2011;9:83.
Acknowledgements
The authors thank the patients who joined the hypertension health service of the NEPHSP and the staff working in the primary healthcare centers who collected the data.
Funding
The work was supported by the Guangdong Basic and Applied Basic Research Foundation, China (grant no. 2022A1515110747, 2024A1515010973), the Shenzhen Medical Research Fund (B2303004), and the Sanming Project of Medicine in Shenzhen, China (SZSM202311001). The founders had no role in the design, analysis, or writing of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, G., Ren, Z., Zhao, J. et al. Blood pressure satisfaction and antihypertensive medication adherence effects frailty transitions in older hypertensive patients. Hypertens Res (2026). https://doi.org/10.1038/s41440-025-02530-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41440-025-02530-3