Abstract
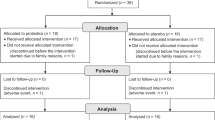
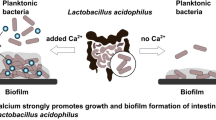
Aging is accompanied by low-grade intestinal inflammation, shifts in gut microbiota, and impaired oxidative balance. Probiotic supplementation has been proposed to mitigate these processes, yet evidence in elderly populations remains limited. In this pilot trial, older adults received oral Lactiplantibacillus plantarum OL3246 or placebo, with assessments including fecal calprotectin and zonulin as markers of intestinal inflammation, systemic oxidative stress parameters, self-reported quality of life and mood, and gut microbiome composition analyzed by sequencing and functional profiling. L. plantarum OL3246 supplementation was well tolerated and associated with consistent improvements across clinical, biochemical, and microbial measures. Participants reported enhanced quality of life and mood, while fecal calprotectin levels declined, indicating reduced intestinal inflammation. Moreover, oxidative stress markers improved with lower AOPP, stabilization of SOD, and restoration of redox balance. Microbiome analyses showed greater diversity and enrichment of health-associated taxa. These findings indicate that Lactiplantibacillus plantarum OL3246 may support healthy aging.
Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study contain sensitive medical information. In accordance with patient confidentiality, GDPR regulations, and the requirements of the local ethics committee, these data cannot be made publicly available. Importantly, the data have been presented in the manuscript in the form of dot plots, ensuring transparency and allowing independent assessment of the findings without access to raw medical records. For ethically justified and scientifically sound requests, limited access to anonymized datasets may be considered upon reasonable request to the corresponding author (J.M.), under conditions that guarantee data protection and confidentiality.
References
Williams, G.A., Cylus, J. & Roubal. T. Sustainable Health Financing with an Ageing Population (European Observatory on Health Systems and Policies, 2019).
Aiyar, S. & Ebeke, C. H. The Impact of Workforce Aging on European Productivity (International Monetary Fund, 2017).
Kalfoss, M. H., Reidunsdatter, R. J., Klöckner, C. A. & Nilsen, M. Validation of the WHOQOL-Bref: psychometric properties and normative data for the Norwegian general population. Health Qual. Life Outcomes 19, 13 (2021).
Mosaad Ali, M., Kamel Mosbah, S. & Mahmoud Abo El-Fadl, N. Factors affecting quality of life and work productivity among patients with gout. Am. J. Nurs. Res. 7, 128–135 (2019).
Gonzalez, L. A. D. et al. Health-related quality of life, financial toxicity, productivity loss and catastrophic health expenditures after lung cancer diagnosis in Argentina. arXiv [econ.GN] https://doi.org/10.21203/rs.3.rs-2365239/v1 (2022).
Yoshino, O., Takahashi, N. & Suzukamo, Y. Menstrual symptoms, health-related quality of life, and work productivity in Japanese women with dysmenorrhea receiving different treatments: prospective observational study. Adv. Ther. 39, 2562–2577 (2022).
López-Otín, C., Blasco, M. A., Partridge, L., Serrano, M. & Kroemer, G. Hallmarks of aging: an expanding universe. Cell 186, 243–278 (2023).
Kaeberlein, M. Longevity and aging. F1000Prime Rep. 5, 5 (2013).
Guo, J. et al. Aging and aging-related diseases: from molecular mechanisms to interventions and treatments. Signal Transduct. Target. Ther. 7, 391 (2022).
Petersen, C. & Round, J. L. Defining dysbiosis and its influence on host immunity and disease. Cell. Microbiol. 16, 1024–1033 (2014).
Conway, J. & A Duggal, N. Ageing of the gut microbiome: potential influences on immune senescence and inflammageing. Ageing Res. Rev. 68, 101323 (2021).
Golshany, H. et al. The gut microbiome across the lifespan: how diet modulates our microbial ecosystem from infancy to the elderly. Int. J. Food Sci. Nutr. 76, 95–121 (2025).
Tavella, T. et al. Elevated gut microbiome abundance of Christensenellaceae, Porphyromonadaceae and Rikenellaceae is associated with reduced visceral adipose tissue and healthier metabolic profile in Italian elderly. Gut Microbes 13, 1–19 (2021).
Boopathi, S. et al. Gut Enterobacteriaceae and uraemic toxins—perpetrators for ageing. Exp. Gerontol. 173, 112088 (2023).
Iwaniak, P., Owe-Larsson, M. & Urbańska, E. M. Microbiota, tryptophan and aryl hydrocarbon receptors as the target triad in Parkinson’s disease—a narrative review. Int. J. Mol. Sci. 25, 2915 (2024).
Marć, M. A., Jastrząb, R. & Mytych, J. Does the gut microbial metabolome really matter? The connection between GUT metabolome and neurological disorders. Nutrients 14, 3967 (2022).
Kadyan, S. et al. Resistant starches from dietary pulses improve neurocognitive health via gut–microbiome–brain axis in aged mice. Front. Nutr. 11, 1322201 (2024).
World Report on Ageing and Health https://www.who.int/publications/i/item/9789241565042 (2015).
Capuron, L. & Miller, A. H. Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol. Ther. 130, 226–238 (2011).
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W. & Kelley, K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9, 46–56 (2008).
Lee, J. W. et al. Higher patient activation is associated with lower odds of functional limitation in older adults with chronic diseases. Geriatr. Nurs. 61, 157–161 (2025).
Religioni, U., Barrios-Rodríguez, R., Requena, P., Borowska, M. & Ostrowski, J. Enhancing therapy adherence: impact on clinical outcomes, healthcare costs, and patient quality of life. Medicina (Kaunas) 61, 153 (2025).
Moskalev, A., Stambler, I. & Caruso, C. Innate and adaptive immunity in aging and longevity: the foundation of resilience. Aging Dis 11, 1363–1373 (2020).
Zhang, W., Xiao, D., Mao, Q. & Xia, H. Role of neuroinflammation in neurodegeneration development. Signal Transduct. Target. Ther. 8, 267 (2023).
Jastrząb, R. et al. The strain-dependent cytostatic activity of Lactococcus lactis on CRC cell lines is mediated through the release of arginine deiminase. Microb. Cell Fact. 23, 82 (2024).
Snigdha, S. et al. Probiotics: potential novel therapeutics for microbiota–gut–brain axis dysfunction across gender and lifespan. Pharmacol. Ther. 231, 107978 (2022).
Kumar, A. et al. Probiotics as modulators of gut–brain axis for cognitive development. Front. Pharmacol. 15, 1348297 (2024).
Ojha, S., Patil, N., Jain, M., Kole, C. & Kaushik, P. Probiotics for neurodegenerative diseases: a systematic review. Microorganisms 11, 1083 (2023).
Castelli, V. et al. The emerging role of probiotics in neurodegenerative diseases: new hope for Parkinson’s disease?. Neural Regen. Res. 16, 628–634 (2021).
Hutchinson, A. N. et al. The effect of probiotics on health outcomes in the elderly: a systematic review of randomized, placebo-controlled studies. Microorganisms 9, 1344 (2021).
Östlund-Lagerström, L. et al. Probiotic administration among free-living older adults: a double blinded, randomized, placebo-controlled clinical trial. Nutr. J. 15, 80 (2016).
Nyangale, E. P. et al. Bacillus coagulans GBI-30, 6086 modulates Faecalibacterium prausnitzii in older men and women. J. Nutr. 145, 1446–1452 (2015).
Kim, C.-S. et al. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: a randomized, double-blind, placebo-controlled, multicenter trial. J. Gerontol. A Biol. Sci. Med. Sci. 76, 32–40 (2021).
Tylka, J. & Piotrowicz, R. Quality of life questionnaire SF-36—Polish version. Kardiol. Pol. 67, 1166–1169 (2009).
Aalto, A.-M., Elovainio, M., Kivimäki, M., Uutela, A. & Pirkola, S. The Beck Depression Inventory and General Health Questionnaire as measures of depression in the general population: a validation study using the Composite International Diagnostic Interview as the gold standard. Psychiatry Res. 197, 163–171 (2012).
Suija, K. et al. Validation of the Whooley questions and the Beck Depression Inventory in older adults. Scand. J. Prim. Health Care 30, 259–264 (2012).
Segal, D. L., Coolidge, F. L., Cahill, B. S. & O’Riley, A. A. Psychometric properties of the Beck Depression Inventory II (BDI-II) among community-dwelling older adults. Behav. Modif. 32, 3–20 (2008).
Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 37, 852–857 (2019).
Callahan, B. J. et al. DADA2: high-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
Quast, C. et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2013).
Lozupone, C. & Knight, R. UniFrac: a new phylogenetic method for comparing microbial communities. Appl. Environ. Microbiol. 71, 8228–8235 (2005).
Anderson, M. J. A new method for non-parametric multivariate analysis of variance. Austral Ecol. 26, 32–46 (2001).
Lin, H. & Peddada, S. D. Analysis of compositions of microbiomes with bias correction. Nat. Commun. 11, 3514 (2020).
Douglas, G. M. et al. PICRUSt2 for prediction of metagenome functions. Nat. Biotechnol. 38, 685–688 (2020).
Fan, Z. et al. Lactobacillus casei CCFM1074 alleviates collagen-induced arthritis in rats via balancing Treg/Th17 and modulating the metabolites and gut microbiota. Front. Immunol. 12, 680073 (2021).
Zabolotneva, A. A. et al. The obesogenic gut microbiota as a crucial factor defining the depletion of predicted enzyme abundance for vitamin B12 synthesis in the mouse intestine. Biomedicines 12, 1280 (2024).
Mihailović, M. et al. Beneficial effects of probiotic Lactobacillus paraplantarum BGCG11 on pancreatic and duodenum function in diabetic rats. Int. J. Mol. Sci. 25, 7697 (2024).
Zhou, H., He, K., Chen, J. & Zhang, X. LinDA: linear models for differential abundance analysis of microbiome compositional data. Genome Biol 23, 95 (2022).
Wickham, H. Ggplot2 (Springer International Publishing, 2016).
Knight, R. et al. Best practices for analysing microbiomes. Nat. Rev. Microbiol. 16, 410–422 (2018).
Hussenoeder, F. S. et al. Depression and quality of life in old age: a closer look. Eur. J. Ageing 18, 75–83 (2021).
Jomova, K. et al. Reactive oxygen species, toxicity, oxidative stress, and antioxidants: chronic diseases and aging. Arch. Toxicol. 97, 2499–2574 (2023).
Rahman, M. A. et al. Oxidative stress in DNA damage and neurodegenerative diseases: unveiling the mechanisms and therapeutic opportunities. Cell Biochem. Biophys. https://doi.org/10.1007/s12013-025-01845-9 (2025).
Ahmad Fadzuli, N. I. et al. Faecal intestinal permeability and intestinal inflammatory markers in older adults with age-related disorders: a systematic review and meta-analysis. Ageing Res. Rev. 101, 102506 (2024).
Padhi, P. et al. Mechanistic insights into gut microbiome dysbiosis-mediated neuroimmune dysregulation and protein misfolding and clearance in the pathogenesis of chronic neurodegenerative disorders. Front. Neurosci. 16, 836605 (2022).
Zhou, H., Tang, L., Fenton, K. A. & Song, X. Exploring and evaluating microbiome resilience in the gut. FEMS Microbiol. Ecol. 101, fiaf046 (2025).
Kossowska, M. et al. The interplay between gut microbiota and cognitive functioning in the healthy aging population: a systematic review. Nutrients 16, 852 (2024).
Foster, J. A. & McVey Neufeld, K.-A. Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 36, 305–312 (2013).
Le Morvan de Sequeira, C., Kaeber, M., Cekin, S. E., Enck, P. & Mack, I. The effect of probiotics on quality of life, depression and anxiety in patients with irritable bowel syndrome: a systematic review and meta-analysis. J. Clin. Med. 10, 3497 (2021).
van der Waal, M. B. et al. Probiotics for improving quality of life in ulcerative colitis: exploring the patient perspective. PharmaNutrition 7, 100139 (2019).
Recharla, N., Choi, J., Puligundla, P., Park, S.-J. & Lee, H.-J. Impact of probiotics on cognition and constipation in the elderly: a meta-analysis. Heliyon 9, e18306 (2023).
Moludi, J. et al. The efficacy of probiotics supplementation on the quality of life of patients with gastrointestinal disease: a systematic review of clinical studies. Prev. Nutr. Food Sci. 29, 237–255 (2024).
Button, K. S. et al. Minimal clinically important difference on the Beck Depression Inventory-II according to the patient’s perspective. Psychol. Med. 45, 3269–3279 (2015).
Wang, C. et al. Effectiveness of psychological interventions among community-dwelling older adults with subthreshold depression: a systematic review and meta-analysis. J. Affect. Disord. 354, 368–375 (2024).
Brody, D. J. & Hughes, J. P. Depression prevalence in adolescents and adults: United States, August 2021–August 2023. NCHS Data Brief 1, (2025).
Melo, D. et al. Prevalence and determinants of depressive symptoms in older adults across Europe: evidence from SHARE Wave 9. J. Clin. Med. 14, 5340 (2025).
Zenebe, Y., Akele, B., W/Selassie, M. & Necho, M. Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Ann. Gen. Psychiatry 20, 55 (2021).
Jalali, A. et al. Global prevalence of depression, anxiety, and stress in the elderly population: a systematic review and meta-analysis. BMC Geriatr. 24, 809 (2024).
Wang, B. et al. Global, regional, and national burden and attributable risk factors of depressive disorders among older adults, 1990–2021. Int. Psychogeriatr. 37, 100069 (2025).
Rahmannia, M. et al. Strain-specific effects of probiotics on depression and anxiety: a meta-analysis. Gut Pathog. 16, 46 (2024).
Saccarello, A. et al. Oral administration of S-adenosylmethionine (SAMe) and Lactobacillus plantarum HEAL9 improves the mild-to-moderate symptoms of depression: a randomized, double-blind, placebo-controlled study. Prim. Care Companion CNS Disord. 22, 19m02578 (2020).
Ho, Y.-T., Tsai, Y.-C., Kuo, T. B. J. & Yang, C. C. H. Effects of Lactobacillus plantarum PS128 on depressive symptoms and sleep quality in self-reported insomniacs: a randomized, double-blind, placebo-controlled pilot trial. Nutrients 13, 2820 (2021).
Godzien, J. et al. Probiotic Lactobacillus plantarum 299v supplementation in patients with major depression in a double-blind, randomized, placebo-controlled trial: a metabolomics study. J. Affect. Disord. 368, 180–190 (2025).
Rudzki, L. et al. Probiotic Lactobacillus plantarum 299v decreases kynurenine concentration and improves cognitive functions in patients with major depression: a double-blind, randomized, placebo controlled study. Psychoneuroendocrinology 100, 213–222 (2019).
Milajerdi, A. et al. The effect of probiotics on inflammatory biomarkers: a meta-analysis of randomized clinical trials. Eur. J. Nutr. 59, 633–649 (2020).
Cristofori, F. et al. Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: a door to the body. Front. Immunol. 12, 578386 (2021).
Abdi, A., Oroojzadeh, P., Valivand, N., Sambrani, R. & Lotfi, H. Immunological aspects of probiotics for improving skin diseases: influence on the gut–brain–skin axis. Biochem. Biophys. Res. Commun. 702, 149632 (2024).
Zeng, L. et al. Safety and efficacy of probiotic supplementation in 8 types of inflammatory arthritis: a systematic review and meta-analysis of 34 randomized controlled trials. Front. Immunol. 13, 961325 (2022).
Pavlidou, E., Fasoulas, A., Mantzorou, M. & Giaginis, C. Clinical evidence on the potential beneficial effects of probiotics and prebiotics in cardiovascular disease. Int. J. Mol. Sci. 23, 15898 (2022).
Chatsirisakul, O. et al. Strain-specific therapeutic potential of Lactiplantibacillus plantarum: a systematic scoping review. Nutrients 17, 1165 (2025).
Han, K. J., Lee, J.-E., Lee, N.-K. & Paik, H.-D. Antioxidant and anti-inflammatory effect of probiotic Lactobacillus plantarum KU15149 derived from Korean homemade diced-radish Kimchi. J. Microbiol. Biotechnol. 30, 591–598 (2020).
Luan, X., Feng, M. & Sun, J. Effect of Lactobacillus plantarum on antioxidant activity in fermented sausage. Food Res. Int. 144, 110351 (2021).
DÜz, M., DoĞan, Y. N. & DoĞan İ. Antioxidant activitiy of Lactobacillus plantarum, Lactobacillus sake and Lactobacillus curvatus strains isolated from fermented Turkish Sucuk. An. Acad. Bras. Cienc. 92, e20200105 (2020).
Wang, J. et al. Lactobacillus plantarum exhibits antioxidant and cytoprotective activities in porcine intestinal epithelial cells exposed to hydrogen peroxide. Oxidative Med. Cell. Longev. 2021, 8936907 (2021).
Ge, Q. et al. Antioxidant activity of Lactobacillus plantarum NJAU-01 in an animal model of aging. BMC Microbiol. 21, 182 (2021).
Lazou-Ahrén, I. et al. Probiotic-reduced inflammaging in older adults: a randomized, double-blind, placebo-controlled trial. Probiotics Antimicrob. Proteins https://doi.org/10.1007/s12602-024-10310-7 (2024).
Dzięgielewska-Gęsiak, S., Wysocka, E., Fatyga, E. & Muc-Wierzgoń, M. Relationship of SOD-1 activity in metabolic syndrome and/or frailty in elderly individuals. Metabolites 14, 514 (2024).
Silva, L. A. D., Malfatti, C. R. M., Soares, K. C. N., Silva, M. C. D. & Brasil, M. R. Unraveling the interplay of oxidative stress, aging, and skeletal muscle: insights and interventions for optimal muscle function in the elderly. J. Adv. Med. Med. Res. 35, 21–27 (2023).
Zelko, I. N., Mariani, T. J. & Folz, R. J. Superoxide dismutase multigene family: a comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Radic. Biol. Med. 33, 337–349 (2002).
Landis, G. N. & Tower, J. Superoxide dismutase evolution and life span regulation. Mech. Ageing Dev. 126, 365–379 (2005).
Conti, G. et al. Association of higher advanced oxidation protein products (AOPPs) levels in patients with diabetic and hypertensive nephropathy. Medicina (Kaunas) 55, 675 (2019).
Villalpando-Sánchez, D. C. et al. Advanced oxidative protein products had a diagnostic accuracy for identifying chronic Kidney Disease in adult population. Metabolites 14, 37 (2024).
Koike, A. et al. Thiol groups as a biomarker for the diagnosis and prognosis of prostate cancer. Sci. Rep. 10, 9093 (2020).
Napiórkowska-Mastalerz, M. et al. A preliminary evaluation of advanced oxidation protein products (AOPPs) as a potential approach to evaluating prognosis in early-stage breast cancer patients and its implication in tumour angiogenesis: a 7-year single-centre study. Cancers (Basel) 16, 1068 (2024).
Skvarilová, M., Bulava, A., Stejskal, D., Adamovská, S. & Bartek, J. Increased level of advanced oxidation products (AOPP) as a marker of oxidative stress in patients with acute coronary syndrome. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc Czech Repub. 149, 83–87 (2005).
Gonzalez, E. et al. An increase of plasma advanced oxidation protein products levels is associated with cardiovascular risk in incident peritoneal dialysis patients: a pilot study. Oxidative Med. Cell. Longev. 2015, 1–6 (2015).
Lou, A. et al. Advanced oxidation protein products induce inflammatory responses and invasive behaviour in fibroblast-like synoviocytes via the RAGE–NF-κB pathway. Bone Jt. Res. 10, 259–268 (2021).
Maciejczyk, M., Nesterowicz, M., Szulimowska, J. & Zalewska, A. Oxidation, glycation, and carbamylation of salivary biomolecules in healthy children, adults, and the elderly: can saliva be used in the assessment of aging? J. Inflamm. Res. 15, 2051–2073 (2022).
Baraibar, M. A., Liu, L., Ahmed, E. K. & Friguet, B. Protein oxidative damage at the crossroads of cellular senescence, aging, and age-related diseases. Oxid. Med. Cell. Longev. 2012, 919832 (2012).
Demirbilek, M. E., Kilic, N., Komurcu, H. F. & Akin, K. O. Advanced oxidation protein products in aged with dementia. Am. J. Immunol. 3, 52–55 (2007).
Saez, I. Cologne Excellence Cluster for Cellular Stress Responses in Aging-Associated Diseases (CECAD), University of Cologne, Joseph Stelzmann Strasse 26, 50931 Cologne, Germany & Vilchez, D. Protein clearance mechanisms and their demise in age-related neurodegenerative diseases. AIMS Mol. Sci. 2, 1–21 (2015).
Lin, K.-J. et al. The overcrowded crossroads: mitochondria, alpha-synuclein, and the endo-lysosomal system interaction in Parkinson’s disease. Int. J. Mol. Sci. 20, 5312 (2019).
Bougea, A. et al. Plasma alpha-synuclein levels in patients with Parkinson’s disease: a systematic review and meta-analysis. Neurol. Sci. 40, 929–938 (2019).
Noori, M. et al. The effect of probiotic-fortified kefir on depression, appetite, oxidative stress, and inflammatory parameters in Iranian overweight and obese elderly: a randomized, double-blind, placebo-controlled clinical trial. J. Health Popul. Nutr. 44, 30 (2025).
Hsu, Y.-C. et al. Efficacy of probiotic supplements on brain-derived neurotrophic factor, inflammatory biomarkers, oxidative stress and cognitive function in patients with Alzheimer’s dementia: a 12-week randomized, double-blind active-controlled study. Nutrients 16, 16 (2023).
Ma, T. et al. Targeting gut microbiota and metabolism as the major probiotic mechanism—an evidence-based review. Trends Food Sci. Technol. 138, 178–198 (2023).
Nourizadeh, R. et al. (Eds.). Impact of probiotics in modulation of gut microbiome. In Microbiome–Gut–Brain Axis 401–409 (Springer Nature, 2022).
Brookes, M. J., Whitehead, S., Gaya, D. R. & Hawthorne, A. B. Practical guidance on the use of faecal calprotectin. Frontline Gastroenterol. 9, 87–91 (2018).
Joshi, S., Lewis, S. J., Creanor, S. & Ayling, R. M. Age-related faecal calprotectin, lactoferrin and tumour M2-PK concentrations in healthy volunteers. Ann. Clin. Biochem. 47, 259–263 (2010).
Mulak, A., Koszewicz, M., Panek-Jeziorna, M., Koziorowska-Gawron, E. & Budrewicz, S. Fecal calprotectin as a marker of the gut immune system activation is elevated in Parkinson’s disease. Front. Neurosci. 13, 992 (2019).
Dumitrescu, L. et al. Serum and fecal markers of intestinal inflammation and intestinal barrier permeability are elevated in Parkinson’s disease. Front. Neurosci. 15, 689723 (2021).
Gallo, A. et al. Diagnostic accuracy of fecal calprotectin in discriminating organic-inflammatory gastrointestinal diseases and functional gastrointestinal disorders in older patients. J. Pers. Med. 14, 227 (2024).
Heinzel, S. et al. Elevated fecal calprotectin is associated with gut microbial dysbiosis, altered serum markers and clinical outcomes in older individuals. Sci. Rep. 14, 13513 (2024).
Seethaler, B. et al. Biomarkers for assessment of intestinal permeability in clinical practice. Am. J. Physiol. Gastrointest. Liver Physiol. 321, G11–G17 (2021).
Aquilani, R. et al. Effects of a metabolic mixture on gut inflammation and permeability in elderly patients with Chronic Kidney Disease: a proof-of-concept study. Metabolites 12, 987 (2022).
Malíčková, K. et al. Fecal zonulin is elevated in Crohn’s disease and in cigarette smokers. Pract. Lab. Med. 9, 39–44 (2017).
Qi, Y. et al. Intestinal permeability biomarker zonulin is elevated in healthy aging. J. Am. Med. Dir. Assoc. 18, 810.e1–810.e4 (2017).
Mörkl, S. et al. Gut microbiota, dietary intakes and intestinal permeability reflected by serum zonulin in women. Eur. J. Nutr. 57, 2985–2997 (2018).
Heidt, C. et al. Assessment of intestinal permeability and inflammation bio-markers in patients with rheumatoid arthritis. Nutrients 15, 2386 (2023).
Moreno-Navarrete, J. M., Sabater, M., Ortega, F., Ricart, W. & Fernández-Real, J. M. Circulating zonulin, a marker of intestinal permeability, is increased in association with obesity-associated insulin resistance. PLoS ONE 7, e37160 (2012).
Sokol, H. et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. USA 105, 16731–16736 (2008).
Machiels, K. et al. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut 63, 1275–1283 (2014).
Salvi, P. S. & Cowles, R. A. Butyrate and the intestinal epithelium: modulation of proliferation and inflammation in homeostasis and disease. Cells 10, 1775 (2021).
Canani, R. B. et al. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J. Gastroenterol. 17, 1519–1528 (2011).
Hodgkinson, K. et al. Butyrate’s role in human health and the current progress towards its clinical application to treat gastrointestinal disease. Clin. Nutr. 42, 61–75 (2023).
Formiga, R. & Sokol, H. Faecalibacterium prausnitzii: one species with multiple potential implications in cancer research. Gut 74, 1038–1039 (2025).
Navab-Moghadam, F. et al. The association of type II diabetes with gut microbiota composition. Microb. Pathog. 110, 630–636 (2017).
Zhang, Y. et al. Faecalibacterium prausnitzii prevents age-related heart failure by suppressing ferroptosis in cardiomyocytes through butyrate-mediated LCN2 regulation. Gut Microbes 17, 2505119 (2025).
Yin, Q. et al. Ecological dynamics of Enterobacteriaceae in the human gut microbiome across global populations. Nat. Microbiol. 10, 541–553 (2025).
Biagi, E. et al. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS ONE 5, e10667 (2010).
Ma, T. et al. Probiotic consumption relieved human stress and anxiety symptoms possibly via modulating the neuroactive potential of the gut microbiota. Neurobiol. Stress 14, 100294 (2021).
Kamil, R. Z., Murdiati, A., Juffrie, M. & Rahayu, E. S. Gut microbiota modulation of moderate undernutrition in infants through gummy Lactobacillus plantarum Dad-13 consumption: a randomized double-blind controlled trial. Nutrients 14, 1049 (2022).
Baxter, N. T. et al. Dynamics of human gut microbiota and short-chain fatty acids in response to dietary interventions with three fermentable fibers. MBio 10, e02566–18 (2019).
Soto-Martin, E. C. et al. Vitamin biosynthesis by human gut butyrate-producing bacteria and cross-feeding in synthetic microbial communities. MBio 11, e00886-20 (2020).
Park, J. et al. Dietary vitamin B1 intake influences gut microbial community and the consequent production of short-chain fatty acids. Nutrients 14, 2078 (2022).
Pham, V. T., Dold, S., Rehman, A., Bird, J. K. & Steinert, R. E. Vitamins, the gut microbiome and gastrointestinal health in humans. Nutr. Res. 95, 35–53 (2021).
Tarracchini, C. et al. Exploring the vitamin biosynthesis landscape of the human gut microbiota. mSystems 9, e0092924 (2024).
Culp, E. J. & Goodman, A. L. Cross-feeding in the gut microbiome: ecology and mechanisms. Cell Host Microbe 31, 485–499 (2023).
Marcelino, V. R. et al. Disease-specific loss of microbial cross-feeding interactions in the human gut. Nat. Commun. 14, 6546 (2023).
Acknowledgements
This research was funded by the National Centre for Research and Development (NCBiR, Poland), under the grant number POIR.01.01.01-00-0985/17.
Author information
Authors and Affiliations
Contributions
R.J.: writing—review and editing, writing—original draft, software, data curation, visualization, formal analysis, conceptualization, and funding acquisition; A.M.: methodology, investigation, and data curation; E.K.M.: methodology, investigation, and data curation; A.G.: methodology, investigation, and data curation; B.K.: resources, methodology, and investigation; K.K.: methodology and investigation; J.W.-K.: methodology and investigation; D.W.: methodology, investigation, and data curation; K.M. methodology, investigation, and data curation; M.N.-Ch.: methodology, investigation, and data curation; D.L.: methodology, investigation, and data curation; K.G.: methodology, investigation, and data curation; M.G.: methodology, investigation, and data curation; N.P.: methodology, investigation, and data curation; G.P.: methodology, investigation, and data curation; G.K.: methodology, investigation, and data curation; J.M.: supervision, writing—review and editing, resources, project administration, and conceptualization. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
This study was sponsored by Olimp Laboratories Sp. z o.o., which received a public research grant from the National Centre for Research and Development (NCBiR, Poland). The funding agency had no role in the study design, data analysis, interpretation, or the decision to submit the article for publication. The study was conceptually designed by investigators from the Academy of Physical Education, Katowice, Poland, and Medical University of Silesia, Katowice, Poland, in cooperation with the R&D department of Olimp Laboratories Sp. z o.o., and subsequently approved by the sponsor. The investigational product was developed and manufactured in-house at Olimp Laboratories Sp. z o.o. by company employees who are also co-authors of this paper. The sponsor had no role in data analysis, interpretation of results, manuscript writing, or the decision to submit for publication. These details are now explicitly stated in the revised manuscript to ensure full transparency. All aspects of patient recruitment, data collection, data management, and preliminary statistical analysis were performed independently by the Academy of Physical Education, Katowice, Poland and Medical University of Silesia, Katowice, Poland research teams. The final statistical analyses were conducted by the first author and independently cross-checked by the Academy of Physical Education, Katowice, Poland and Medical University of Silesia, Katowice, Poland co-authors to ensure accuracy. JM, RJ, BK, KK, JW-K, DW, and KM are employees of Olimp Laboratories Sp. z o.o. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jastrząb, R., Małecki, A., Kmiecik-Małecka, E. et al. Probiotic Lactiplantibacillus plantarum OL3246 supports healthy aging by enhancing quality of life, reducing inflammation, and modulating gut microbiota: a pilot study. npj Aging (2026). https://doi.org/10.1038/s41514-026-00338-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41514-026-00338-0