Abstract
Sex is a significant determinant of cancer incidence and outcome. The effects of sexual differentiation on normal and cancer biology underly this epidemiology. The resultant sex differences in therapeutic target pathways and processes provide a foundation for developing more personalized cancer treatments. However, our efforts at personalization cannot stop there. Humans also have gender, and sex and gender are highly interactive in individuation. Thus, we will also need to consider how gender–sex interactions (GSI) affect cancer biology and clinical parameters such as the timing of diagnoses, clinical trial enrolment, and the completeness of efficacy and toxicity data. Ignoring the effects of GSI can compromise the quality of basic biological and clinical data and the conclusions drawn from them. This is not to say that GSI will always have a significant effect or any effect at all in every cancer study. Rather, it is to say that we know enough about GSI and human cancer to anticipate measurable differences when GSI are considered in research, enabling us to experimentally determine whether their effects are significant. Here, I delve deeply into GSI and cancer, as this approach to treatment personalization holds great promise to benefit all patients with cancer.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ashley, D. J. A male-female differential in tumour incidence. Br. J. Cancer 23, 21–25 (1969).
Jackson, S. S. et al. Sex disparities in the incidence of 21 cancer types: quantification of the contribution of risk factors. Cancer 128, 3531–3540 (2022).
Goodenough, U. & Heitman, J. Origins of eukaryotic sexual reproduction. Cold Spring Harb. Perspect. Biol. 6, https://doi.org/10.1101/cshperspect.a016154 (2014).
Hosken, D. J., Archer, C. R. & Mank, J. E. Sexual conflict. Curr. Biol. 29, R451–R455 (2019).
Cliquet, R. The relevance of sociobiological theory for emancipatory feminism. J. Hum. Evol. 13, 117–127 (1984).
Rubin, J. B. The spectrum of sex differences in cancer. Trends Cancer 8, 303–315 (2022).
Rubin, J. B. et al. Sex differences in cancer mechanisms. Biol. Sex Differ. 11, 17 (2020).
Lonsdorf, E. V. et al. Sex differences in wild chimpanzee behavior emerge during infancy. PLoS One 9, e99099 (2014).
Nattrass, S. et al. Postreproductive killer whale grandmothers improve the survival of their grandoffspring. Proc. Natl Acad. Sci. USA 116, 26669–26673 (2019).
Seltmann, M. W., Helle, S., Htut, W. & Lahdenpera, M. Males have more aggressive and less sociable personalities than females in semi-captive Asian elephants. Sci. Rep. 9, 2668 (2019).
Bouzy, J., Brunelle, J., Cohen, D. & Condat, A. Transidentities and autism spectrum disorder: a systematic review. Psychiatry Res. 323, 115176 (2023).
Cooper, K., Smith, L. G. E. & Russell, A. J. Gender identity in autism: sex differences in social affiliation with gender groups. J. Autism Dev. Disord. 48, 3995–4006 (2018).
Mograbi, D. C., Rodrigues, R., Bienemann, B. & Huntley, J. Brain networks, neurotransmitters and psychedelics: towards a neurochemistry of self-awareness. Curr. Neurol. Neurosci. Rep. 24, 323–340 (2024).
Strang, J. F. et al. The autism spectrum among transgender youth: default mode functional connectivity. Cereb. Cortex 33, 6633–6647 (2023).
Franconi, F., Campesi, I., Colombo, D. & Antonini, P. Sex-gender variable: methodological recommendations for increasing scientific value of clinical studies. Cells 8, 476 (2019).
Kennedy, B. et al. Loss of a parent and the risk of cancer in early life: a nationwide cohort study. Cancer Causes Control 25, 499–506 (2014).
Chida, Y., Hamer, M., Wardle, J. & Steptoe, A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat. Clin. Pract. Oncol. 5, 466–475 (2008).
Yang, T. et al. Work stress and the risk of cancer: a meta-analysis of observational studies. Int. J. Cancer 144, 2390–2400 (2019).
Schoemaker, M. J. et al. Psychological stress, adverse life events and breast cancer incidence: a cohort investigation in 106,000 women in the United Kingdom. Breast Cancer Res. 18, 72 (2016).
Butow, P. et al. Does stress increase risk of breast cancer? A 15-year prospective study. Psychooncology 27, 1908–1914 (2018).
Choi, Y., Kim, J. K. & Yoo, J. Y. NFκB and STAT3 synergistically activate the expression of FAT10, a gene counteracting the tumor suppressor p53. Mol. Oncol. 8, 642–655 (2014).
Gonzalez-Aponte, M. F. et al. Daily glucocorticoids promote glioblastoma growth and circadian synchrony to the host. Cancer Cell 43, 144–160.e7 (2025).
Schwarzlmueller, P. et al. Steroid hormones as modulators of anti-tumoural immunity. Nat. Rev. Endocrinol. https://doi.org/10.1038/s41574-025-01102-2 (2025).
Oyola, M. G. & Handa, R. J. Hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes: sex differences in regulation of stress responsivity. Stress 20, 476–494 (2017).
Le Mevel, J. C., Abitbol, S., Beraud, G. & Maniey, J. Temporal changes in plasma adrenocorticotropin concentration after repeated neurotropic stress in male and female rats. Endocrinology 105, 812–817 (1979).
Young, E. A. Sex differences in response to exogenous corticosterone: a rat model of hypercortisolemia. Mol. Psychiatry 1, 313–319 (1996).
Verma, R., Balhara, Y. P. & Gupta, C. S. Gender differences in stress response: role of developmental and biological determinants. Ind. Psychiatry J. 20, 4–10 (2011).
Handa, R. J., Burgess, L. H., Kerr, J. E. & O’Keefe, J. A. Gonadal steroid hormone receptors and sex differences in the hypothalamo-pituitary-adrenal axis. Horm. Behav. 28, 464–476 (1994).
Khadka, S., Druffner, S. R., Duncan, B. C. & Busada, J. T. Glucocorticoid regulation of cancer development and progression. Front. Endocrinol. 14, 1161768 (2023).
Ruiz, A. M. et al. An integrative literature review and critical reflection of intersectionality theory. Nurs. Inq. 28, e12414 (2021).
Lu, J. et al. An egg-adult association, gender, and reproduction in pterosaurs. Science 331, 321–324 (2011).
Suvorov, A. Modalities of aging in organisms with different strategies of resource allocation. Ageing Res. Rev. 82, 101770 (2022).
Fisher, D. O., Dickman, C. R., Jones, M. E. & Blomberg, S. P. Sperm competition drives the evolution of suicidal reproduction in mammals. Proc. Natl Acad. Sci. USA 110, 17910–17914 (2013).
Gutierrez-Adan, A. et al. Developmental consequences of sexual dimorphism during pre-implantation embryonic development. Reprod. Domest. Anim. 41, 54–62 (2006).
Ray, P. F., Conaghan, J., Winston, R. M. & Handyside, A. H. Increased number of cells and metabolic activity in male human preimplantation embryos following in vitro fertilization. J. Reprod. Fertil. 104, 165–171 (1995).
Tsunoda, Y., Tokunaga, T. & Sugie, T. Altered sex ratio of live young after transfer of fast- and slow-developing mouse embryos. Mol. Rep. Dev. 12, 301–304 (1985).
Darwin, C. Origin of the Species (Macmillan Collector’s Library, 2017).
Rubin, J. B. et al. Epigenetic developmental mechanisms underlying sex differences in cancer. J. Clin. Invest. 134, https://doi.org/10.1172/JCI180071 (2024).
Tiffin, G. J., Rieger, D., Betteridge, K. J., Yadav, B. R. & King, W. A. Glucose and glutamine metabolism in pre-attachment cattle embryos in relation to sex and stage of development. J. Reprod. Fertil. 93, 125–132 (1991).
Hunter, S. K. & Senefeld, J. W. Sex differences in human performance. J. Physiol. 602, 4129–4156 (2024).
Stanyon, R. & Bigoni, F. Sexual selection and the evolution of behavior, morphology, neuroanatomy and genes in humans and other primates. Neurosci. Biobehav. Rev. 46P4, 579–590 (2014).
Lenz, K. M., Nugent, B. M., Haliyur, R. & McCarthy, M. M. Microglia are essential to masculinization of brain and behavior. J. Neurosci. 33, 2761–2772 (2013).
Caulin, A. F. & Maley, C. C. Peto’s Paradox: evolution’s prescription for cancer prevention. Trends Ecol. Evol. 26, 175–182 (2011).
Smith, G. D., Shipley, M. & Leon, D. A. Height and mortality from cancer among men: prospective observational study. BMJ 317, 1351–1352 (1998).
Green, J. et al. Height and cancer incidence in the million women study: prospective cohort, and meta-analysis of prospective studies of height and total cancer risk. Lancet Oncol. 12, 785–794 (2011).
Tomasetti, C. et al. Role of stem-cell divisions in cancer risk. Nature 548, E13–E14 (2017).
Frankel, S., Gunnell, D. J., Peters, T. J., Maynard, M. & Smith, G. D. Childhood energy intake and adult mortality from cancer: the Boyd Orr cohort study. BMJ 316, 499–504 (1998).
Estrella, C. A. S. et al. Asymmetric growth-limiting development of the female conceptus. Front. Endocrinol. 14, 1306513 (2023).
Centers for Disease Control and Prevention, National Center for Health Statistics. WHO Growth Standards Are Recommended for Use in the U.S. for Infants and Children 0 to 2 Years of Age https://www.cdc.gov/growthcharts/who_charts.htm (2010).
Nunney, L. Size matters: height, cell number and a person’s risk of cancer. Proc. Biol. Sci. 285, https://doi.org/10.1098/rspb.2018.1743 (2018).
Lemaitre, J. F. et al. The influence of early-life allocation to antlers on male performance during adulthood: evidence from contrasted populations of a large herbivore. J. Anim. Ecol. 87, 921–932 (2018).
Lemaitre, J. F. et al. Sex differences in adult lifespan and aging rates of mortality across wild mammals. Proc. Natl Acad. Sci. USA 117, 8546–8553 (2020).
Tombak, K. J., Hex, S. & Rubenstein, D. I. New estimates indicate that males are not larger than females in most mammal species. Nat. Commun. 15, 1872 (2024).
Lahdenpera, M., Mar, K. U. & Lummaa, V. Nearby grandmother enhances calf survival and reproduction in Asian elephants. Sci. Rep. 6, 27213 (2016).
Martinez de Toda, I. et al. Sex differences in markers of oxidation and inflammation. Implications for ageing. Mech. Ageing Dev. 211, 111797 (2023).
Podolskiy, D. I., Lobanov, A. V., Kryukov, G. V. & Gladyshev, V. N. Analysis of cancer genomes reveals basic features of human aging and its role in cancer development. Nat. Commun. 7, 12157 (2016).
Tiberi, J. et al. Sex differences in antioxidant defence and the regulation of redox homeostasis in physiology and pathology. Mech. Ageing Dev. 211, 111802 (2023).
Knewtson, K. E., Ohl, N. R. & Robinson, J. L. Estrogen signaling dictates musculoskeletal stem cell behavior: sex differences in tissue repair. Tissue Eng. Part B Rev. 28, 789–812 (2022).
Shi, Y. et al. Sex difference in human diseases: mechanistic insights and clinical implications. Signal Transduct. Target. Ther. 9, 238 (2024).
Broestl, L. et al. Gonadal sex patterns p21-induced cellular senescence in mouse and human glioblastoma. Commun. Biol. 5, 781 (2022).
Yang, W. et al. Sex differences in GBM revealed by analysis of patient imaging, transcriptome, and survival data. Sci. Transl. Med. 11, https://doi.org/10.1126/scitranslmed.aao5253 (2019).
Chhabra, Y. et al. Sex-dependent effects in the aged melanoma tumor microenvironment influence invasion and resistance to targeted therapy. Cell 187, 6016–6034.e25 (2024).
Forma, E., Jozwiak, P., Brys, M. & Krzeslak, A. The potential role of O-GlcNAc modification in cancer epigenetics. Cell. Mol. Biol. Lett. 19, 438–460 (2014).
Ji, J., Zoller, B., Sundquist, J. & Sundquist, K. Risk of solid tumors and hematological malignancy in persons with Turner and Klinefelter syndromes: a national cohort study. Int. J. Cancer 139, 754–758 (2016).
Popotas, A., Casimir, G. J., Corazza, F. & Lefevre, N. Sex-related immunity: could Toll-like receptors be the answer in acute inflammatory response? Front. Immunol. 15, 1379754 (2024).
Haupt, S. et al. Identification of cancer sex-disparity in the functional integrity of p53 and its X chromosome network. Nat. Commun. 10, 5385 (2019).
Chen, X. et al. Sex difference in neural tube defects in p53-null mice is caused by differences in the complement of X not Y genes. Dev. Neurobiol. 68, 265–273 (2008).
Zhang, D. et al. Inactivation of KDM6A promotes the progression of colorectal cancer by enhancing the glycolysis. Eur. J. Med. Res. 29, 310 (2024).
Tran, N., Broun, A. & Ge, K. Lysine demethylase KDM6A in differentiation, development, and cancer. Mol. Cell. Biol. 40, https://doi.org/10.1128/MCB.00341-20 (2020).
Kaneko, S. & Li, X. X chromosome protects against bladder cancer in females via a KDM6A-dependent epigenetic mechanism. Sci. Adv. 4, eaar5598 (2018).
Shen, L. et al. DDX3 acts as a tumor suppressor in colorectal cancer as loss of DDX3 in advanced cancer promotes tumor progression by activating the MAPK pathway. Int. J. Biol. Sci. 18, 3918–3933 (2022).
Patmore, D. M. et al. DDX3X suppresses the susceptibility of hindbrain lineages to medulloblastoma. Dev. Cell 54, 455–470.e5 (2020).
Dunford, A. et al. Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias. Nat. Genet. 49, 10–16 (2017).
Pierre, R. V. & Hoagland, H. C. Age-associated aneuploidy: loss of Y chromosome from human bone marrow cells with aging. Cancer 30, 889–894 (1972).
Ly, P. et al. Selective Y centromere inactivation triggers chromosome shattering in micronuclei and repair by non-homologous end joining. Nat. Cell Biol. 19, 68–75 (2017).
Mitchell, E. et al. Clonal dynamics of haematopoiesis across the human lifespan. Nature 606, 343–350 (2022).
Forsberg, L. A. et al. Mosaic loss of chromosome Y in peripheral blood is associated with shorter survival and higher risk of cancer. Nat. Genet. 46, 624–628 (2014).
Abdel-Hafiz, H. A. et al. Y chromosome loss in cancer drives growth by evasion of adaptive immunity. Nature 619, 624–631 (2023).
Mattisson, J. et al. Loss of chromosome Y in regulatory T cells. BMC Genomics 25, 243 (2024).
Li, J. et al. Histone demethylase KDM5D upregulation drives sex differences in colon cancer. Nature 619, 632–639 (2023).
Li, Y., Zhang, D. J., Qiu, Y., Kido, T. & Lau, Y. C. The Y-located proto-oncogene TSPY exacerbates and its X-homologue TSPX inhibits transactivation functions of androgen receptor and its constitutively active variants. Hum. Mol. Genet. 26, 901–912 (2017).
Dhanoa, J. K., Mukhopadhyay, C. S. & Arora, J. S. Y-chromosomal genes affecting male fertility: a review. Vet. World 9, 783–791 (2016).
Balaresque, P. et al. Y-chromosome descent clusters and male differential reproductive success: young lineage expansions dominate Asian pastoral nomadic populations. Eur. J. Hum. Genet. 23, 1413–1422 (2015).
Zerjal, T. et al. The genetic legacy of the mongols. Am. J. Hum. Genet. 72, 717–721 (2003).
Frank, S. A. & Hurst, L. D. Mitochondria and male disease. Nature 383, 224 (1996).
Radzvilavicius, A., Layh, S., Hall, M. D., Dowling, D. K. & Johnston, I. G. Sexually antagonistic evolution of mitochondrial and nuclear linkage. J. Evol. Biol. 34, 757–766 (2021).
Mauvais-Jarvis, F. Sex differences in energy metabolism: natural selection, mechanisms and consequences. Nat. Rev. Nephrol. 20, 56–69 (2024).
Wallace, D. C. Genetics: mitochondrial DNA in evolution and disease. Nature 535, 498–500 (2016).
Gebert, C. et al. DNA methylation in the IGF2 intragenic DMR is re-established in a sex-specific manner in bovine blastocysts after somatic cloning. Genomics 94, 63–69 (2009).
Lumey, L. H., Stein, A. D., Kahn, H. S. & Romijn, J. A. Lipid profiles in middle-aged men and women after famine exposure during gestation: the Dutch hunger winter families study. Am. J. Clin. Nutr. 89, 1737–1743 (2009).
Ravelli, A. C., van Der Meulen, J. H., Osmond, C., Barker, D. J. & Bleker, O. P. Obesity at the age of 50 y in men and women exposed to famine prenatally. Am. J. Clin. Nutr. 70, 811–816 (1999).
Veenendaal, M. V. et al. Transgenerational effects of prenatal exposure to the 1944-45 Dutch famine. BJOG 120, 548–553 (2013).
Vagero, D., Pinger, P. R., Aronsson, V. & van den Berg, G. J. Paternal grandfather’s access to food predicts all-cause and cancer mortality in grandsons. Nat. Commun. 9, 5124 (2018).
Bygren, L. O. et al. Change in paternal grandmothers’ early food supply influenced cardiovascular mortality of the female grandchildren. BMC Genet. 15, 12 (2014).
van den Berg, G. J. & Pinger, P. R. Transgenerational effects of childhood conditions on third generation health and education outcomes. Econ. Hum. Biol. 23, 103–120 (2016).
Maher, E. R. & Reik, W. Beckwith-Wiedemann syndrome: imprinting in clusters revisited. J. Clin. Invest. 105, 247–252 (2000).
Harvey, M. B. & Kaye, P. L. IGF-2 stimulates growth and metabolism of early mouse embryos. Mech. Dev. 38, 169–173 (1992).
Azzi, S. et al. Multilocus methylation analysis in a large cohort of 11p15-related foetal growth disorders (Russell Silver and Beckwith Wiedemann syndromes) reveals simultaneous loss of methylation at paternal and maternal imprinted loci. Hum. Mol. Genet. 18, 4724–4733 (2009).
Latos, P. A. et al. Airn transcriptional overlap, but not its lncRNA products, induces imprinted Igf2r silencing. Science 338, 1469–1472 (2012).
Ferguson-Smith, A. C. & Surani, M. A. Imprinting and the epigenetic asymmetry between parental genomes. Science 293, 1086–1089 (2001).
Peters, J. The role of genomic imprinting in biology and disease: an expanding view. Nat. Rev. Genet. 15, 517–530 (2014).
Faisal, M., Kim, H. & Kim, J. Sexual differences of imprinted genes’ expression levels. Gene 533, 434–438 (2014).
Tan, Q. et al. Age patterns of intra-pair DNA methylation discordance in twins: sex difference in epigenomic instability and implication on survival. Aging Cell 20, e13460 (2021).
Grant, O. A., Wang, Y., Kumari, M., Zabet, N. R. & Schalkwyk, L. Characterising sex differences of autosomal DNA methylation in whole blood using the Illumina EPIC array. Clin. Epigenetics 14, 62 (2022).
Terao, M. et al. Turnover of mammal sex chromosomes in the Sry-deficient Amami spiny rat is due to male-specific upregulation of Sox9. Proc. Natl Acad. Sci. USA 119, e2211574119 (2022).
Koopman, P., Gubbay, J., Vivian, N., Goodfellow, P. & Lovell-Badge, R. Male development of chromosomally female mice transgenic for Sry. Nature 351, 117–121 (1991).
De Vries, G. J. et al. A model system for study of sex chromosome effects on sexually dimorphic neural and behavioral traits. J. Neurosci. 22, 9005–9014 (2002).
Arnold, A. P. & Chen, X. What does the “four core genotypes” mouse model tell us about sex differences in the brain and other tissues? Front. Neuroendocrinol. 30, 1–9 (2009).
Guo, X., Puttabyatappa, M., Domino, S. E. & Padmanabhan, V. Developmental programming: prenatal testosterone-induced changes in epigenetic modulators and gene expression in metabolic tissues of female sheep. Mol. Cell. Endocrinol. 514, 110913 (2020).
Matsuda, K. I. et al. Histone deacetylation during brain development is essential for permanent masculinization of sexual behavior. Endocrinology 152, 2760–2767 (2011).
Nugent, B. M. et al. Brain feminization requires active repression of masculinization via DNA methylation. Nat. Neurosci. 18, 690–697 (2015).
Johansen, M. L. et al. Gliomas display distinct sex-based differential methylation patterns based on molecular subtype. Neurooncol. Adv. 2, vdaa002 (2020).
Ren, Y. et al. Gender specificity improves the early-stage detection of clear cell renal cell carcinoma based on methylomic biomarkers. Biomark. Med. 12, 607–618 (2018).
Lin, S. et al. Sex-related DNA methylation differences in B cell chronic lymphocytic leukemia. Biol. Sex Differ. 10, 2 (2019).
Kundakovic, M. & Tickerhoof, M. Epigenetic mechanisms underlying sex differences in the brain and behavior. Trends Neurosci. 47, 18–35 (2024).
Yoh, K., Ikeda, K., Horie, K. & Inoue, S. Roles of estrogen, estrogen receptors, and estrogen-related receptors in skeletal muscle: regulation of mitochondrial function. Int. J. Mol. Sci. 24, https://doi.org/10.3390/ijms24031853 (2023).
Spoletini, I., Vitale, C., Malorni, W. & Rosano, G. M. Sex differences in drug effects: interaction with sex hormones in adult life. Handb. Exp. Pharmacol. 214, 91–105 (2012).
Ucciferri, C. C. & Dunn, S. E. Effect of puberty on the immune system: relevance to multiple sclerosis. Front. Pediatr. 10, 1059083 (2022).
Deamer, W. C. Stimulation of growth in boys by sublingual testosterone therapy. Am. J. Dis. Child. 75, 850–859 (1948).
Fujita, K. Cytochrome P450 and anticancer drugs. Curr. Drug. Metab. 7, 23–37 (2006).
Naqvi, S. et al. Conservation, acquisition, and functional impact of sex-biased gene expression in mammals. Science 365, https://doi.org/10.1126/science.aaw7317 (2019).
Berner, A. M. & Atkinson, S. E. The implications of hormone treatment for cancer risk, screening and treatment in transgender individuals. Best Pract. Res. Clin. Endocrinol. Metab. 38, 101909 (2024).
Pott, P. Chirurgical Observations Relative to the Cataract, the Polypus of the Nose, and Cancer of the Scrotum (1775).
Dijksterhuis, W. P. M. et al. Gender differences in treatment allocation and survival of advanced gastroesophageal cancer: a population-based study. J. Natl Cancer Inst. 113, 1551–1560 (2021).
Sarasqueta, C. et al. Gender differences in stage at diagnosis and preoperative radiotherapy in patients with rectal cancer. BMC Cancer 20, 759 (2020).
Din, N. U. et al. Age and gender variations in cancer diagnostic intervals in 15 cancers: analysis of data from the UK clinical practice research datalink. PLoS One 10, e0127717 (2015).
Kalathoor, S. et al. Representation of women in clinical trials supporting FDA-approval of contemporary cancer therapies. Int. J. Cancer 155, 1958–1968 (2024).
Pala, L., De Pas, T. & Conforti, F. Under-representation of women in randomized clinical trials testing anticancer immunotherapy may undermine female patients care. a call to action. Semin. Oncol. 49, 400–404 (2022).
Bierer, B. E., Meloney, L. G., Ahmed, H. R. & White, S. A. Advancing the inclusion of underrepresented women in clinical research. Cell Rep. Med. 3, 100553 (2022).
Widdowson, E. M. The response of the sexes to nutritional stress. Proc. Nutr. Soc. 35, 175–180 (1976).
Grayson, D. Differential mortality and the donner party disaster. Evol. Anthropol. 2, 151–150 (1993).
Zarulli, V. et al. Women live longer than men even during severe famines and epidemics. Proc. Natl Acad. Sci. USA 115, E832–E840 (2018).
Krumsiek, J. et al. Gender-specific pathway differences in the human serum metabolome. Metabolomics 11, 1815–1833 (2015).
Sponagel, J. et al. Sex differences in brain tumor glutamine metabolism reveal sex-specific vulnerabilities to treatment. Med 3, 792–811.e12 (2022).
Ippolito, J. E., Yim, A. K., Luo, J., Chinnaiyan, P. & Rubin, J. B. Sexual dimorphism in glioma glycolysis underlies sex differences in survival. JCI Insight 2, https://doi.org/10.1172/jci.insight.92142 (2017).
Menezo, Y. J., Chouteau, J., Torello, J., Girard, A. & Veiga, A. Birth weight and sex ratio after transfer at the blastocyst stage in humans. Fertil. Steril. 72, 221–224 (1999).
Prochazkova, M. et al. Vegan diet is associated with favorable effects on the metabolic performance of intestinal microbiota: a cross-sectional multi-omics study. Front. Nutr. 8, 783302 (2021).
Connolly-Schoonen, J. et al. A pilot controlled feeding trial modifying protein intake in healthy subjects to assess adherence and the metabolome. Nutr. Cancer 75, 1499–1510 (2023).
Santangelo, C. et al. Dietary habits, physical activity and body mass index in transgender and gender diverse adults in Italy: a voluntary sampling observational study. Nutrients 16, https://doi.org/10.3390/nu16183139 (2024).
Lyu, W., Yu, L. & Lv, H. Gender wage gap and child malnutrition in Ethiopia: a probit instrumental variable method. Heliyon 10, e37000 (2024).
Ahmed, F. et al. Political economy of maternal child malnutrition: experiences about water, food, and nutrition policies in Pakistan. Nutrients 16, https://doi.org/10.3390/nu16162642 (2024).
Yang, W. & Rubin, J. B. Treating sex and gender differences as a continuous variable can improve precision cancer treatments. Biol. Sex Differ. 15, 35 (2024).
Conforti, F. et al. Sex-based heterogeneity in response to lung cancer immunotherapy: a systematic review and meta-analysis. J. Natl Cancer Inst. 111, 772–781 (2019).
Conforti, F. et al. Sex-based dimorphism of anticancer immune response and molecular mechanisms of immune evasion. Clin. Cancer Res. 27, 4311–4324 (2021).
Conforti, F. et al. Sex-based differences in response to anti-PD-1 or PD-L1 treatment in patients with non-small-cell lung cancer expressing high PD-L1 levels. A systematic review and meta-analysis of randomized clinical trials. ESMO Open 6, 100251 (2021).
Santoni, M. et al. The impact of gender on the efficacy of immune checkpoint inhibitors in cancer patients: the MOUSEION-01 study. Crit. Rev. Oncol. Hematol. 170, 103596 (2022).
Chakrabarty, A., Chakraborty, S., Nandi, D. & Basu, A. Multivariate genetic architecture reveals testosterone-driven sexual antagonism in contemporary humans. Proc. Natl Acad. Sci. USA 121, e2404364121 (2024).
Bland, H. T. et al. Conducting inclusive research in genetics for transgender, gender-diverse, and sex-diverse individuals: case analyses and recommendations from a clinical genomics study. J. Genet. Couns. 33, 772–785 (2024).
Hanson, K. et al. Understanding the intersection of identity and cancer experience among racially, ethnically, gender and sexual minoritized adolescents and young adults with cancer. Psychooncology 33, e70000 (2024).
Martinez, A., Delpierre, C., Grosclaude, P. & Lamy, S. Integrating gender into cancer research. Lancet 403, 1631 (2024).
Gehrels, A. M. et al. Gender differences in tumor characteristics, treatment allocation and survival in stage I-III pancreatic cancer: a nationwide study. Eur. J. Cancer 206, 114117 (2024).
Stenzel, A. E. et al. Discrimination in the medical setting among LGBTQ+ adults and associations with cancer screening. Cancer Causes Control https://doi.org/10.1007/s10552-024-01927-8 (2024).
Kfoury, N. et al. Brd4-bound enhancers drive cell-intrinsic sex differences in glioblastoma. Proc. Natl Acad. Sci. USA 118, https://doi.org/10.1073/pnas.2017148118 (2021).
Kfoury, N. et al. Cooperative p16 and p21 action protects female astrocytes from transformation. Acta Neuropathol. Commun. 6, 12 (2018).
Klein, S. L. & Flanagan, K. L. Sex differences in immune responses. Nat. Rev. Immunol. 16, 626–638 (2016).
Figtree, G. A., Noonan, J. E., Bhindi, R. & Collins, P. Estrogen receptor polymorphisms: significance to human physiology, disease and therapy. Recent. Pat. DNA Gene Seq. 3, 164–171 (2009).
Giovannucci, E. et al. The CAG repeat within the androgen receptor gene and its relationship to prostate cancer. Proc. Natl Acad. Sci. USA 94, 3320–3323 (1997).
Han, G. et al. The AIB1 gene polyglutamine repeat length polymorphism contributes to risk of epithelial ovarian cancer risk: a case-control study. Tumour Biol. 36, 371–374 (2015).
Wang, Q., Udayakumar, T. S., Vasaitis, T. S., Brodie, A. M. & Fondell, J. D. Mechanistic relationship between androgen receptor polyglutamine tract truncation and androgen-dependent transcriptional hyperactivity in prostate cancer cells. J. Biol. Chem. 279, 17319–17328 (2004).
He, Y. et al. Androgen receptor with short polyglutamine tract preferably enhances Wnt/β-catenin-mediated prostatic tumorigenesis. Oncogene 39, 3276–3291 (2020).
Perret, M. Litter sex composition affects first reproduction in female grey mouse lemurs (Microcebus murinus). Physiol. Behav. 208, 112575 (2019).
Monclus, R. & Blumstein, D. T. Litter sex composition affects life-history traits in yellow-bellied marmots. J. Anim. Ecol. 81, 80–86 (2012).
Yang, W., Wong, J. & Rubin, J. Sex and Gender: Transforming Scientific Practice Vol. 36 (Springer-Nature, 2025).
Mauvais-Jarvis, F. et al. Sex- and gender-based pharmacological response to drugs. Pharmacol. Rev. 73, 730–762 (2021).
Patwardhan, V. et al. Differences across the lifespan between females and males in the top 20 causes of disease burden globally: a systematic analysis of the global burden of disease study 2021. Lancet Public Health 9, e282–e294 (2024).
Vera, R., Juan-Vidal, O., Safont-Aguilera, M. J., de la Pena, F. A. & Del Alba, A. G. Sex differences in the diagnosis, treatment and prognosis of cancer: the rationale for an individualised approach. Clin. Transl. Oncol. 25, 2069–2076 (2023).
Whitmire, P. et al. Sex-specific impact of patterns of imageable tumor growth on survival of primary glioblastoma patients. BMC Cancer 20, 447 (2020).
Rakshith, H. T., Lohita, S., Rebello, A. P., Goudanavar, P. S. & Raghavendra Naveen, N. Sex differences in drug effects and/or toxicity in oncology. Curr. Res. Pharmacol. Drug Discov. 4, 100152 (2023).
Dong, M. et al. Sex differences in cancer incidence and survival: a pan-cancer analysis. Cancer Epidemiol. Biomark. Prev. 29, 1389–1397 (2020).
Goh, R. et al. Resuscitation orders demonstrate differences by gender, stroke type and intervention. J. Stroke Cerebrovasc. Dis. 33, 107881 (2024).
Cathcart-Rake, E. J. et al. Sexual orientation and gender identity data collection in cancer care: a nationwide landscape assessment update. JCO Oncol. Pract. 20, 1272–1279 (2024).
Triplette, M. et al. A multistakeholder qualitative study to inform sexual orientation and gender identity data collection in the cancer care setting. LGBT Health https://doi.org/10.1089/lgbt.2024.0065 (2024).
Wheldon, C. W., Sklarz, T. & Frosch, Z. A. K. Advancing equity in cancer care: the critical role of sexual orientation and gender identity data collection. JCO Oncol. Pract. 20, 1146–1148 (2024).
Hunt, L., Nielsen, M. W. & Schiebinger, L. A framework for sex, gender, and diversity analysis in research. Science 377, 1492–1495 (2022).
Rajendran, A. et al. Sex-specific differences in cardiovascular risk factors and implications for cardiovascular disease prevention in women. Atherosclerosis 384, 117269 (2023).
Stamellou, E. et al. Sex-specific differences in kidney function and blood pressure regulation. Int. J. Mol. Sci. 25, https://doi.org/10.3390/ijms25168637 (2024).
Cherubini, A., Della Torre, S., Pelusi, S. & Valenti, L. Sexual dimorphism of metabolic dysfunction-associated steatotic liver disease. Trends Mol Med. https://doi.org/10.1016/j.molmed.2024.05.013 (2024).
Gardner, D. K. & Leese, H. J. Assessment of embryo viability prior to transfer by the noninvasive measurement of glucose uptake. J. Exp. Zool. 242, 103–105 (1987).
Gardner, D. K., Wale, P. L., Collins, R. & Lane, M. Glucose consumption of single post-compaction human embryos is predictive of embryo sex and live birth outcome. Hum. Reprod. 26, 1981–1986 (2011).
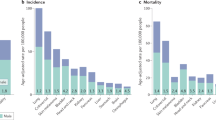
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. DietaryGuidelines.gov (2020).
Batheja, D., Goel, S. & Charani, E. Understanding gender inequities in antimicrobial resistance: role of biology, behaviour and gender norms. BMJ Glob. Health 10, https://doi.org/10.1136/bmjgh-2024-016711 (2025).
Gibbs, D. L. et al. Robust cluster prediction across data types validates association of sex and therapy response in GBM. Cancers 17, https://doi.org/10.3390/cancers17030445 (2025).
Mauvais-Jarvis, F. et al. Sex and gender: modifiers of health, disease, and medicine. Lancet 396, 565–582 (2020).
Funer, F. Admitting the heterogeneity of social inequalities: intersectionality as a (self-)critical framework and tool within mental health care. Philos. Ethics Humanit. Med. 18, 21 (2023).
Enaifoghe, A. The influence of culture and gender differences in communication: society’s perception. Res. Bus. Soc. Sci. 12, 460–468 (2023).
Acknowledgements
I would like to acknowledge all the people who have discussed these topics with me over the years. Work on sex differences in the Rubin lab is supported by R01 CA174737-07, NIH PO1 CA245705, Joshua’s Great Things and The St Louis Children’s Hospital Foundation.
Author information
Authors and Affiliations
Contributions
The author handled all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Peer review
Peer review information
Nature Reviews Cancer thanks Xue Li, who co-reviewed with Singha Biplab and Gian-Paolo Dotto, who co-reviewed with Jovan Isma, for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Dietary guidelines of the U.S. Department of Agriculture and U.S. Department of Health and Human Services: DietaryGuidelines.gov: https://www.fns.usda.gov/cnpp/dietary-guidelines-americans
Electronic Human Relations Area Files (eHRAF): https://ehrafworldcultures.yale.edu/
Glossary
- Anabolism
-
The process of building complex molecules from simple ones.
- Anthropomorphic
-
Attribution of human traits to animals.
- Bayesian statistical approach
-
Bayesian statistics are distinct as they incorporate prior knowledge into prior probability distributions allowing for each new piece of data to be incorporated into prior knowledge such that prior probability distributions for each iteration of an experiment can change.
- Consomic Y model
-
Consomic strains of inbred mice possess single chromosomes, like a Y chromosome, derived from another strain through a series of backcrosses.
- Darwinopterus
-
Darwinopterus is a pterosaur, named after Charles Darwin, that lived between 150 and 170 million years ago.
- Default mode network
-
A large-scale functional brain network that is most active when an individual is not interacting with the outside world, such as when they are resting, daydreaming, thinking about themselves and others, remembering or planning.
- DNA imprints
-
An epigenetic phenomenon involving DNA methylation in gametes that results in genes being expressed or not as a function of whether they were maternally or paternally inherited.
- Gender
-
Human traits and behaviours that derive from self-identity interacting with social and cultural expectations about what it means to be a man, a woman or non-binary.
- Gender–sex interaction
-
(GSI). The complex ways in which gender and sex interact to determine an individual’s phenotype and life experience.
- Hominidae
-
The taxonomic primate family, also known as the great apes, that includes orangutans, gorillas, chimpanzees and humans.
- Hypothalamic–pituitary–adrenal axis
-
A brain–body system for the regulation of endocrinological responses to stress.
- Intersectionality
-
A sociological paradigm for integrating the multiple unique contributions of systematized privilege and discrimination to an individual’s life.
- Marsupial
-
Marsupials are mammals that are distinguished by having both placentae for early gestational development and an external pouch in which the completion of gestation takes place.
- Meiotic crossing-over
-
Chromosomal crossover occurs during meiosis between two homologous chromosomes to produce new recombinant chromosomes.
- Mode
-
A statistical term meaning the most common value in a dataset.
- Polymorphic variation
-
The condition of there being more than one allele of the same gene that differs in DNA sequence within a population.
- Sex
-
The shared reproductive biology between humans and other sexually reproducing mammals.
- Transcriptomic index approach
-
A Bayesian-based analysis of cancer transcriptomes that supports deeper phenotyping of patients for treatment stratification based on their similarity to other patients of the same sex.
- Wilms tumour
-
A rare kidney cancer that most commonly affects young children.
- Y allele
-
Variation in the sequences of Y-encoded genes within a population.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rubin, J.B. Gender and sex interactions are intrinsic components of cancer phenotypes. Nat Rev Cancer 25, 634–648 (2025). https://doi.org/10.1038/s41568-025-00829-4
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41568-025-00829-4
This article is cited by
-
Checking assumptions: advancing the analysis of sex and gender in health sciences
Biology of Sex Differences (2026)