Abstract
Left ventricular ejection fraction (EF) remains the major parameter for diagnosis, phenotyping, prognosis and treatment decisions in heart failure. The 2016 ESC heart failure guidelines introduced a third EF category for an EF of 40–49%, defined as heart failure with mid-range EF (HFmrEF). This category has been largely unexplored compared with heart failure with reduced EF (HFrEF; defined as EF <40% in this Review) and heart failure with preserved EF (HFpEF; defined as EF ≥50%). The prevalence of HFmrEF within the overall population of patients with HF is 10–25%. HFmrEF seems to be an intermediate clinical entity between HFrEF and HFpEF in some respects, but more similar to HFrEF in others, in particular with regard to the high prevalence of ischaemic heart disease in these patients. HFmrEF is milder than HFrEF, and the risk of cardiovascular events is lower in patients with HFmrEF or HFpEF than in those with HFrEF. By contrast, the risk of non-cardiovascular adverse events is similar or greater in patients with HFmrEF or HFpEF than in those with HFrEF. Evidence from post hoc and subgroup analyses of randomized clinical trials and a trial of an SGLT1–SGLT2 inhibitor suggests that drugs that are effective in patients with HFrEF might also be effective in patients with HFmrEF. Although the EF is a continuous measure with considerable variability, in this comprehensive Review we suggest that HFmrEF is a useful categorization of patients with HF and shares the most important clinical features with HFrEF, which supports the renaming of HFmrEF to HF with mildly reduced EF.
Key points
-
Heart failure (HF) with mildly reduced ejection fraction (EF) (HFmrEF) has been extensively studied, generally using an EF of 40–49%, and accounts for up to 25% of patients with HF.
-
On the basis of contemporary trials and definitions, HFmrEF might be defined as an EF of 41–49%.
-
HFmrEF is an intermediate HF type between HF with preserved EF (HFpEF) and HF with reduced EF (HFrEF) for some characteristics but is more similar to HFrEF for others, especially for the high prevalence of ischaemic heart disease.
-
HFmrEF and HFpEF are milder forms of HF than HFrEF and are associated with a lower risk of cardiovascular and HF events but with a similar or greater risk of non-cardiovascular adverse events.
-
Clinical trials on therapies for HFpEF enrolled patients with an ejection fraction of >40% or ≥45% and did not demonstrate a clear treatment effect; however, subgroup and post hoc analyses suggest that some therapies for HFrEF might also be effective in HFmrEF.
-
These arguments support the current redefinition of HFmrEF as HF with mildly reduced EF instead of HF with mid-range EF.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Conrad, N. et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 391, 572–580 (2018).
Jernberg, T. et al. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA 305, 1677–1684 (2011).
van Riet, E. E. et al. Epidemiology of heart failure: the prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur. J. Heart Fail. 18, 242–252 (2016).
Taylor, C. J. et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000–2017: population based cohort study. BMJ 364, l223 (2019).
Yancy, C. W. et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 136, e137–e161 (2017).
Ponikowski, P. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37, 2129–2200 (2016).
Virani, S. S. et al. Heart disease and stroke statistics — 2021 update: a report from the American Heart Association. Circulation 143, e254–e743 (2021).
Thorvaldsen, T., Benson, L., Dahlstrom, U., Edner, M. & Lund, L. H. Use of evidence-based therapy and survival in heart failure in Sweden 2003–2012. Eur. J. Heart Fail. 18, 503–511 (2016).
Ambrosy, A. P. et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J. Am. Coll. Cardiol. 63, 1123–1133 (2014).
Lund, L. H., Benson, L., Dahlstrom, U. & Edner, M. Association between use of renin–angiotensin system antagonists and mortality in patients with heart failure and preserved ejection fraction. JAMA 308, 2108–2117 (2012).
Lund, L. H. et al. Association between enrolment in a heart failure quality registry and subsequent mortality — a nationwide cohort study. Eur. J. Heart Fail. 19,1107–1116 (2017).
Crespo-Leiro, M. G. et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 20, 1505–1535 (2018).
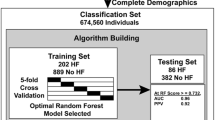
Ahmad, T. et al. Machine learning methods improve prognostication, identify clinically distinct phenotypes, and detect heterogeneity in response to therapy in a large cohort of heart failure patients. J. Am. Heart Assoc. 7, e008081 (2018).
Lund, L. H. Heart failure with “mid-range” ejection fraction — new opportunities. J. Card. Fail. 22, 769–771 (2016).
Lund, L. H., Vedin, O. & Savarese, G. Is ejection fraction in heart failure a limitation or an opportunity? Eur. J. Heart Fail. 20, 431–432 (2018).
Marwick, T. H. Ejection fraction pros and cons: JACC state-of-the-art review. J. Am. Coll. Cardiol. 72, 2360–2379 (2018).
Bhatt, D. L. et al. Sotagliflozin in patients with diabetes and recent worsening heart Failure. N. Engl. J. Med. 384, 117–128 (2020).
Lam, C. S. & Solomon, S. D. The middle child in heart failure: heart failure with mid-range ejection fraction (40–50%). Eur. J. Heart Fail. 16, 1049–1055 (2014).
Bozkurt, B. et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by Canadian Heart Failure Society, Heart Failure Association of India, the Cardiac Society of Australia and New Zealand, and the Chinese Heart Failure Association. Eur. J. Heart Fail. 23, 352–380 (2021).
Lam, C. S. P., Voors, A. A., Piotr, P., McMurray, J. J. V. & Solomon, S. D. Time to rename the middle child of heart failure: heart failure with mildly reduced ejection fraction. Eur. Heart J. 41, 2353–2355 (2020).
Kou, S. et al. Echocardiographic reference ranges for normal cardiac chamber size: results from the NORRE study. Eur. Heart J. Cardiovasc. Imaging 15, 680–690 (2014).
Borlaug, B. A. & Redfield, M. M. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation 123, 2006–2013; discussion 2014 (2011).
Dunlay, S. M., Roger, V. L., Weston, S. A., Jiang, R. & Redfield, M. M. Longitudinal changes in ejection fraction in heart failure patients with preserved and reduced ejection fraction. Circ. Heart Fail. 5, 720–726 (2012).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16, 233–270 (2015).
Galderisi, M. et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 18, 1301–1310 (2017).
Solomon, S. D. et al. Sacubitril/valsartan across the spectrum of ejection fraction in heart failure. Circulation 141, 352–361 (2020).
Dougherty, A. H., Naccarelli, G. V., Gray, E. L., Hicks, C. H. & Goldstein, R. A. Congestive heart failure with normal systolic function. Am. J. Cardiol. 54, 778–782 (1984).
Soufer, R. et al. Intact systolic left ventricular function in clinical congestive heart failure. Am. J. Cardiol. 55, 1032–1036 (1985).
Armstrong, P. W. et al. Vericiguat in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 382, 1883–1893 (2020).
Cohn, J. N. & Tognoni, G., Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N. Engl. J. Med. 345, 1667–1675 (2001).
No Authors Listed. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 353, 2001–2007 (1999).
Young, J. B. et al. Mortality and morbidity reduction with candesartan in patients with chronic heart failure and left ventricular systolic dysfunction: results of the CHARM low-left ventricular ejection fraction trials. Circulation 110, 2618–2626 (2004).
No Authors Listed. A randomized trial of beta-blockade in heart failure. The Cardiac Insufficiency Bisoprolol Study (CIBIS). CIBIS Investigators and Committees. Circulation 90, 1765–1773 (1994).
McMurray, J. J. et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 371, 993–1004 (2014).
McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381, 1995–2008 (2019).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424 (2020).
Zannad, F. et al. Eplerenone in patients with systolic heart failure and mild symptoms. N. Engl. J. Med. 364, 11–21 (2011).
Pitt, B. et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N. Engl. J. Med. 341, 709–717 (1999).
Investigators, S. et al. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N. Engl. J. Med. 325, 293–302 (1991).
Bardy, G. H. et al. Amiodarone or an implantable cardioverter–defibrillator for congestive heart failure. N. Engl. J. Med. 352, 225–237 (2005).
Bristow, M. R. et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N. Engl. J. Med. 350, 2140–2150 (2004).
Teerlink, J. R. et al. Cardiac myosin activation with omecamtiv mecarbil in systolic heart failure. N. Engl. J. Med. (2020).
Moss, A. J. et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N. Engl. J. Med. 346, 877–883 (2002).
Moss, A. J. et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 361, 1329–1338 (2009).
Packer, M. et al. Effect of carvedilol on survival in severe chronic heart failure. N. Engl. J. Med. 344, 1651–1658 (2001).
Savarese, G. et al. Utilizing NT-proBNP for eligibility and enrichment in trials in HFpEF, HFmrEF, and HFrEF. JACC Heart Fail. 6, 246–256 (2018).
Meta-analysis Global Group in Chronic Heart Failure. The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur. Heart J. 33, 1750–1757 (2012).
Koh, A. S. et al. A comprehensive population-based characterization of heart failure with mid-range ejection fraction. Eur. J. Heart Fail. 19, 1624–1634 (2017).
Wehner, G. J. et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur. Heart J. 41, 1249–1257 (2020).
Toma, M. et al. The relationship between left ventricular ejection fraction and mortality in patients with acute heart failure: insights from the ASCEND-HF Trial. Eur. J. Heart Fail. 16, 334–341 (2014).
Yusuf, S. et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 362, 777–781 (2003).
Anker, S. D. et al. Evaluation of the effects of sodium–glucose co-transporter 2 inhibition with empagliflozin on morbidity and mortality in patients with chronic heart failure and a preserved ejection fraction: rationale for and design of the EMPEROR-Preserved trial. Eur. J. Heart Fail. 21, 1279–1287 (2019).
US National Library of Medicine. ClinicalTrials.gov http://clinicaltrials.gov/ct2/show/NCT03619213 (2021).
EU Clinical Trials Register https://www.clinicaltrialsregister.eu/ctr-search/search?query=2017-000697-11 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02901184 (2021).
Lund, L. H., Oldgren, J. & James, S. Registry-based pragmatic trials in heart failure: current experience and future directions. Curr. Heart Fail. Rep. 14, 59–70 (2017).
Pitt, B. et al. Spironolactone for heart failure with preserved ejection fraction. N. Engl. J. Med. 370, 1383–1392 (2014).
Massie, B. M. et al. Irbesartan in patients with heart failure and preserved ejection fraction. N. Engl. J. Med. 359, 2456–2467 (2008).
Solomon, S. D. et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N. Engl. J. Med. 381, 1609–1620 (2019).
Bhatt, D. L. et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N. Engl. J. Med. 384, 117–128 (2021).
Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128, 1810–1852 (2013).
Savarese, G. & Lund, L. H. Global public health burden of heart failure. Card. Fail. Rev. 3, 7–11 (2017).
Groenewegen, A., Rutten, F. H., Mosterd, A. & Hoes, A. W. Epidemiology of heart failure. Eur. J. Heart Fail. 22, 1342–1356 (2020).
Bhambhani, V. et al. Predictors and outcomes of heart failure with mid-range ejection fraction. Eur. J. Heart Fail. 20, 651–659 (2018).
Chioncel, O. et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC heart failure long-term registry. Eur. J. Heart Fail. 19, 1574–1585 (2017).
Douglas, P. S. et al. Echocardiographic imaging in clinical trials: American Society of Echocardiography Standards for echocardiography core laboratories: endorsed by the American College of Cardiology Foundation. J. Am. Soc. Echocardiogr. 22, 755–765 (2009).
Kapoor, J. R. et al. Precipitating clinical factors, heart failure characterization, and outcomes in patients hospitalized with heart failure with reduced, borderline, and preserved ejection fraction. JACC Heart Fail. 4, 464–472 (2016).
Lam, C. S. P. et al. Mortality associated with heart failure with preserved vs. reduced ejection fraction in a prospective international multi-ethnic cohort study. Eur. Heart J. 39, 1770–1780 (2018).
Rickenbacher, P. et al. Heart failure with mid-range ejection fraction: a distinct clinical entity? Insights from the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF). Eur. J. Heart Fail. 19, 1586–1596 (2017).
Tsuji, K. et al. Characterization of heart failure patients with mid-range left ventricular ejection fraction-a report from the CHART-2 Study. Eur. J. Heart Fail. 19, 1258–1269 (2017).
Steinberg, B. A. et al. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation 126, 65–75 (2012).
Lund, L. H. et al. Heart failure with mid-range ejection fraction in CHARM: characteristics, outcomes and effect of candesartan across the entire ejection fraction spectrum. Eur. J. Heart Fail. 20, 1230–1239 (2018).
Srivastava, P. K., Hsu, J. J., Ziaeian, B. & Fonarow, G. C. Heart failure with mid-range ejection fraction. Curr. Heart Fail. Rep. 17, 1–8 (2020).
Fonarow, G. C. et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF registry. J. Am. Coll. Cardiol. 50, 768–777 (2007).
Shah, K. S. et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J. Am. Coll. Cardiol. 70, 2476–2486 (2017).
Sweitzer, N. K., Lopatin, M., Yancy, C. W., Mills, R. M. & Stevenson, L. W. Comparison of clinical features and outcomes of patients hospitalized with heart failure and normal ejection fraction (> or =55%) versus those with mildly reduced (40% to 55%) and moderately to severely reduced (<40%) fractions. Am. J. Cardiol. 101, 1151–1156 (2008).
Kalogeropoulos, A. P. et al. Characteristics and outcomes of adult outpatients with heart failure and improved or recovered ejection fraction. JAMA Cardiol. 1, 510–518 (2016).
Vedin, O. et al. Significance of ischemic heart disease in patients with heart failure and preserved, midrange, and reduced ejection fraction: a nationwide cohort study. Circ Heart Fail. 10, e003875 (2017).
Stolfo, D. et al. Sex-based differences in heart failure across the ejection fraction spectrum: phenotyping, and prognostic and therapeutic implications. JACC Heart Fail. 7, 505–515 (2019).
Savarese, G. et al. Associations with and prognostic and discriminatory role of N-terminal pro-b-type natriuretic peptide in heart failure with preserved versus mid-range versus reduced ejection fraction. J. Card. Fail. 24, 365–374 (2018).
Tromp, J. et al. Biomarker profiles of acute heart failure patients with a mid-range ejection fraction. JACC Heart Fail. 5, 507–517 (2017).
Sartipy, U., Dahlstrom, U., Fu, M. & Lund, L. H. Atrial fibrillation in heart failure with preserved, mid-range, and reduced ejection fraction. JACC Heart Fail. 5, 565–574 (2017).
Lofman, I., Szummer, K., Dahlstrom, U., Jernberg, T. & Lund, L. H. Associations with and prognostic impact of chronic kidney disease in heart failure with preserved, mid-range, and reduced ejection fraction. Eur. J. Heart Fail. 19, 1606–1614 (2017).
Lofman, I. et al. Incidence of, associations with and prognostic impact of worsening renal function in heart failure with different ejection fraction categories. Am. J. Cardiol. 124, 1575–1583 (2019).
Savarese, G. et al. Prevalence of, associations with, and prognostic role of anemia in heart failure across the ejection fraction spectrum. Int. J. Cardiol. 298, 59–65 (2020).
Streng, K. W. et al. Non-cardiac comorbidities in heart failure with reduced, mid-range and preserved ejection fraction. Int. J. Cardiol. 271, 132–139 (2018).
Solomon, S. D. et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur. Heart J. 37, 455–462 (2016).
Borlaug, B. A. et al. Effect of inorganic nitrite vs placebo on exercise capacity among patients with heart failure with preserved ejection fraction: the INDIE-HFpEF randomized clinical trial. JAMA 320, 1764–1773 (2018).
Redfield, M. M. et al. Isosorbide mononitrate in heart failure with preserved ejection fraction. N. Engl. J. Med. 373, 2314–2324 (2015).
Savji, N. et al. The association of obesity and cardiometabolic traits with incident HFpEF and HFrEF. JACC Heart Fail. 6, 701–709 (2018).
Pandey, A. et al. Relationship between physical activity, body mass index, and risk of heart failure. J. Am. Coll. Cardiol. 69, 1129–1142 (2017).
Pandey, A. et al. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC Heart Fail. 6, 975–982 (2018).
Rao, V. N. et al. Adiposity and incident heart failure and its subtypes: MESA (Multi-Ethnic Study of Atherosclerosis). JACC Heart Fail. 6, 999–1007 (2018).
Bartko, P. E. et al. Secondary valve regurgitation in patients with heart failure with preserved ejection fraction, heart failure with mid-range ejection fraction, and heart failure with reduced ejection fraction. Eur. Heart J. 41, 2799–2810 (2020).
Ghio, S. et al. Different correlates but similar prognostic implications for right ventricular dysfunction in heart failure patients with reduced or preserved ejection fraction. Eur. J. Heart Fail. 19, 873–879 (2017).
Li, D. L., Quispe, R., Onyekwelu, C., Faillace, R. T. & Taub, C. C. Racial differences of heart failure with midrange ejection fraction (HFmrEF): a large urban centre-based retrospective cohort study in the USA. BMJ Open 9, e026479 (2019).
Jimenez-Marrero, S. et al. Sympathetic activation and outcomes in chronic heart failure: does the neurohormonal hypothesis apply to mid-range and preserved ejection fraction patients? Eur. J. Intern. Med. 81, 60–66 (2020).
Vergaro, G. et al. Sympathetic and renin–angiotensin–aldosterone system activation in heart failure with preserved, mid-range and reduced ejection fraction. Int. J. Cardiol. 296, 91–97 (2019).
Cleland, J. G. F. et al. Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. Eur. Heart J. 39, 26–35 (2018).
Lauritsen, J., Gustafsson, F. & Abdulla, J. Characteristics and long-term prognosis of patients with heart failure and mid-range ejection fraction compared with reduced and preserved ejection fraction: a systematic review and meta-analysis. ESC Heart Fail. 5, 685–694 (2018).
Cheng, R. K. et al. Outcomes in patients with heart failure with preserved, borderline, and reduced ejection fraction in the Medicare population. Am. Heart J. 168, 721–730 (2014).
Pocock, S. J. et al. Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur. Heart J. 34, 1404–1413 (2013).
Levy, W. C. et al. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation 113, 1424–1433 (2006).
Simpson, J. et al. Prognostic models derived in PARADIGM-HF and validated in atmosphere and the swedish heart failure registry to predict mortality and morbidity in chronic heart failure. JAMA Cardiol. 5, 432–441 (2020).
Parikh, M. N., Lund, L. H., Goda, A. & Mancini, D. Usefulness of peak exercise oxygen consumption and the heart failure survival score to predict survival in patients >65 years of age with heart failure. Am. J. Cardiol. 103, 998–1002 (2009).
Sartipy, U., Dahlstrom, U., Edner, M. & Lund, L. H. Predicting survival in heart failure: validation of the MAGGIC heart failure risk score in 51,043 patients from the Swedish heart failure registry. Eur. J. Heart Fail. 16, 173–179 (2014).
Yang, S., Lund, L. H., Li, S., Dahlstrom, U., Sartipy, U. & Levy, V. Validation of the Seattle heart failure model in the Swedish heart failure registry (abstr.). Circulation 140, A9844 (2019).
Goliasch, G. et al. Refining the prognostic impact of functional mitral regurgitation in chronic heart failure. Eur. Heart J. 39, 39–46 (2018).
Priori, S. G. et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 36, 2793–2867 (2015).
Vaduganathan, M. et al. Mode of death in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 69, 556–569 (2017).
Bilchick, K. C., Stukenborg, G. J., Kamath, S. & Cheng, A. Prediction of mortality in clinical practice for medicare patients undergoing defibrillator implantation for primary prevention of sudden cardiac death. J. Am. Coll. Cardiol. 60, 1647–1655 (2012).
Shadman, R. et al. A novel method to predict the proportional risk of sudden cardiac death in heart failure: derivation of the seattle proportional risk model. Heart Rhythm. 12, 2069–2077 (2015).
Bilchick, K. C. et al. Seattle heart failure and proportional risk models predict benefit from implantable cardioverter–defibrillators. J. Am. Coll. Cardiol. 69, 2606–2618 (2017).
Halliday, B. P. et al. Association between midwall late gadolinium enhancement and sudden cardiac death in patients with dilated cardiomyopathy and mild and moderate left ventricular systolic dysfunction. Circulation 135, 2106–2115 (2017).
Lam, C. S. & Teng, T. H. Understanding heart failure with mid-range ejection fraction. JACC Heart Fail. 4, 473–476 (2016).
Greenberg, B. Heart failure preserved ejection fraction with coronary artery disease: time for a new classification? J. Am. Coll. Cardiol. 63, 2828–2830 (2014).
Hwang, S. J., Melenovsky, V. & Borlaug, B. A. Implications of coronary artery disease in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 63, 2817–2827 (2014).
Lupon, J. et al. Heart failure with preserved ejection fraction infrequently evolves toward a reduced phenotype in long-term survivors. Circ. Heart Fail. 12, e005652 (2019).
Rusinaru, D. et al. Coronary artery disease and 10-year outcome after hospital admission for heart failure with preserved and with reduced ejection fraction. Eur. J. Heart Fail. 16, 967–976 (2014).
Savarese, G. et al. Reductions in N-terminal pro-brain natriuretic peptide levels are associated with lower mortality and heart failure hospitalization rates in patients with heart failure with mid-range and preserved ejection fraction. Circ. Heart Fail. 9, e003105 (2016).
Savarese, G. et al. Changes of natriuretic peptides predict hospital admissions in patients with chronic heart failure. A meta-analysis. JACC: Heart Fail. 2, 148–158 (2014).
Savarese, G. et al. Prevalence and prognostic implications of longitudinal ejection fraction change in heart failure. JACC Heart Fail. 7, 306–317 (2019).
Kim, Y. J. & Kim, R. J. The role of cardiac MR in new-onset heart failure. Curr. Cardiol. Rep. 13, 185–193 (2011).
Celutkiene, J. et al. Innovative imaging methods in heart failure: a shifting paradigm in cardiac assessment. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 20, 1615–1633 (2018).
Quarta, G. et al. Cardiac magnetic resonance in heart failure with preserved ejection fraction: myocyte, interstitium, microvascular, and metabolic abnormalities. Eur. J. Heart Fail. 22, 1065–1075 (2020).
Gulati, A. et al. Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309, 896–908 (2013).
Klem, I. et al. Assessment of myocardial scarring improves risk stratification in patients evaluated for cardiac defibrillator implantation. J. Am. Coll. Cardiol. 60, 408–420 (2012).
Potter, E. & Marwick, T. H. Assessment of left ventricular function by echocardiography: the case for routinely adding global longitudinal strain to ejection fraction. JACC Cardiovasc. Imaging 11, 260–274 (2018).
Venkateshvaran, A., Manouras, A., Kjellstrom, B. & Lund, L. H. The additive value of echocardiographic pulmonary to left atrial global strain ratio in the diagnosis of pulmonary hypertension. Int. J. Cardiol. 292, 205–210 (2019).
Kraigher-Krainer, E. et al. Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 63, 447–456 (2014).
Stokke, T. M. et al. Geometry as a confounder when assessing ventricular systolic function: comparison between ejection fraction and strain. J. Am. Coll. Cardiol. 70, 942–954 (2017).
Kalam, K., Otahal, P. & Marwick, T. H. Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart 100, 1673–1680 (2014).
Stanton, T., Leano, R. & Marwick, T. H. Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoring. Circ. Cardiovasc. Imaging 2,356–364 (2009).
Adamo, L. et al. Proteomic signatures of heart failure in relation to left ventricular ejection fraction. J. Am. Coll. Cardiol. 76, 1982–1994 (2020).
Trivieri, M. G. et al. Challenges in cardiac and pulmonary sarcoidosis: JACC state-of-the-art review. J. Am. Coll. Cardiol. 76, 1878–1901 (2020).
Gigli, M. et al. Genetic risk of arrhythmic phenotypes in patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 74, 1480–1490 (2019).
Wahbi, K. et al. Development and validation of a new risk prediction score for life-threatening ventricular tachyarrhythmias in laminopathies. Circulation 140, 293–302 (2019).
Wilcox, J. E., Fang, J. C., Margulies, K. B. & Mann, D. L. Heart failure with recovered left ventricular ejection fraction: JACC scientific expert panel. J. Am. Coll. Cardiol. 76, 719–734 (2020).
Kramer, D. G. et al. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction: a meta-analytic approach. J. Am. Coll. Cardiol. 56, 392–406 (2010).
Ueda, T. et al. Left ventricular ejection fraction (EF) of 55% as cutoff for late transition from heart failure (HF) with preserved EF to HF with mildly reduced EF. Circ. J. 79, 2209–2215 (2015).
Januzzi, J. L. Jr. et al. Association of change in N-terminal pro-B-type natriuretic peptide following initiation of sacubitril-valsartan treatment with cardiac structure and function in patients with heart failure with reduced ejection fraction. JAMA 322, 1085–1095 (2019).
Desai, A. S. et al. Effect of sacubitril–valsartan vs enalapril on aortic stiffness in patients with heart failure and reduced ejection fraction: a randomized clinical trial. JAMA 322, 1077–1084 (2019).
Lupon, J. et al. Recovered heart failure with reduced ejection fraction and outcomes: a prospective study. Eur. J. Heart Fail. 19, 1615–1623 (2017).
Brann, A., Janvanishstaporn, S. & Greenberg, B. Association of prior left ventricular ejection fraction with clinical outcomes in patients with heart failure with midrange ejection fraction. JAMA Cardiol. 5, 1027–1035 (2020).
Lupon, J. et al. Dynamic trajectories of left ventricular ejection fraction in heart failure. J. Am. Coll. Cardiol. 72, 591–601 (2018).
Cleland, J. G. et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur. Heart J. 27, 2338–2345 (2006).
Flather, M. D. et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur. Heart J. 26, 215–225 (2005).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03057951 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03448406 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03877224 (2020).
Lund, L. H., Benson, L., Dahlstrom, U., Edner, M. & Friberg, L. Association between use of beta-blockers and outcomes in patients with heart failure and preserved ejection fraction. JAMA 312, 2008–2018 (2014).
Savarese, G. et al. Comorbidities and cause-specific outcomes in heart failure across the ejection fraction spectrum: A blueprint for clinical trial design. Int. J. Cardiol. 313, 76–82 (2020).
Ibrahim, N. E. et al. Heart failure with mid-range ejection fraction: characterization of patients from the PINNACLE registry(R). ESC. Heart Fail 6, 784–792 (2019).
Halliday, B. P. et al. Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomised trial. Lancet 393, 61–73 (2019).
Rogers, J. K. et al. Analysing recurrent hospitalizations in heart failure: a review of statistical methodology, with application to CHARM-Preserved. Eur. J. Heart Fail. 16, 33–40 (2014).
Alzahrani, T., Tiu, J., Panjrath, G. & Solomon, A. The effect of angiotensin-converting enzyme inhibitors on clinical outcomes in patients with ischemic cardiomyopathy and midrange ejection fraction: a post hoc subgroup analysis from the PEACE trial. Ther. Adv. Cardiovasc. Dis. 12, 351–359 (2018).
Girerd, N., Ferreira, J. P., Rossignol, P. & Zannad, F. A tentative interpretation of the TOPCAT trial based on randomized evidence from the brain natriuretic peptide stratum analysis. Eur. J. Heart Fail. 18, 1411–1414 (2016).
FDA. Final Summary Minutes of the Cardiovascular and Renal Drugs Advisory Committee Meeting December 16, 2020. https://www.fda.gov/media/145548/download (2020).
Abdul-Rahim, A. H. et al. Effect of digoxin in patients with heart failure and mid-range (borderline) left ventricular ejection fraction. Eur. J. Heart Fail. 20, 1139–1145 (2018).
U.S. Food and Drug Administration. Highlights of Prescribing Information – Sacubitril/Valsartan https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/207620s018lbl.pdf (2020).
Seferovic, P. M. et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21, 1169–1186 (2019).
Savarese, G. et al. Non-insulin antihyperglycaemic drugs and heart failure: an overview of current evidence from randomized controlled trials. ESC Heart Fail. 7, 3438–3451 (2020).
Kini, V. et al. Appropriateness of primary prevention implantable cardioverter–defibrillators at the time of generator replacement: are indications still met? J. Am. Coll. Cardiol. 63, 2388–2394 (2014).
Adabag, S. et al. Association of implantable cardioverter defibrillators with survival in patients with and without improved ejection fraction: secondary analysis of the sudden cardiac death in heart failure trial. JAMA Cardiol. 2, 767–774 (2017).
No Authors Listed. Randomised, placebo-controlled trial of carvedilol in patients with congestive heart failure due to ischaemic Heart Disease. Australia/New Zealand Heart Failure Research Collaborative Group. Lancet 349, 375–380 (1997).
Braunwald, E. et al. Angiotensin-converting-enzyme inhibition in stable coronary artery disease. N. Engl. J. Med. 351, 2058–2068 (2004).
Ahmed, A. et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation 114, 397–403 (2006).
Linde, C. et al. Cardiac resynchronization therapy in chronic heart failure with moderately reduced left ventricular ejection fraction: lessons from the Multicenter InSync Randomized Clinical Evaluation MIRACLE EF study. Int. J. Cardiol. 202, 349–355 (2016).
Yamamoto, K., Origasa, H., Hori, M. & Investigators, J. D. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur. J. Heart Fail. 15, 110–118 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03988634 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04435626 (2021).
Pfeffer, M. A. et al. Regional variation in patients and outcomes in the treatment of preserved cardiac function heart failure with an aldosterone antagonist (TOPCAT) trial. Circulation 131, 34–42 (2015).
McGowan, J. H. & Cleland, J. G. Reliability of reporting left ventricular systolic function by echocardiography: a systematic review of 3 methods. Am. Heart J. 146, 388–397 (2003).
Sievers, B. et al. Visual estimation versus quantitative assessment of left ventricular ejection fraction: a comparison by cardiovascular magnetic resonance imaging. Am. Heart J. 150, 737–742 (2005).
Blondheim, D. S. et al. Reliability of visual assessment of global and segmental left ventricular function: a multicenter study by the Israeli Echocardiography Research Group. J. Am. Soc. Echocardiogr. 23, 258–264 (2010).
Lam, C. S. & Solomon, S. D. Fussing over the middle child: heart failure with mid-range ejection fraction. Circulation 135, 1279–1280 (2017).
Pellikka, P. A. et al. Variability in ejection fraction measured by echocardiography, gated single-photon emission computed tomography, and cardiac magnetic resonance in patients with coronary artery disease and left ventricular dysfunction. JAMA Netw. Open 1, e181456 (2018).
Acknowledgements
L.H.L. is supported by the Karolinska Institutet, the Swedish Research Council (grant 523-2014-2336), the Swedish Heart Lung Foundation (grants 20150557, 20190310) and Stockholm County Council (grants 20170112, 20190525).
Author information
Authors and Affiliations
Contributions
G. Savarese, D.S. and L.H.L. researched data for the article, contributed substantially to discussion of the content and wrote the manuscript. All the authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
G. Savarese reports grants and personal fees from AstraZeneca and Vifor; grants and non-financial support from Boehringer Ingelheim; personal fees from Cytokinetics, GENESIS, Medtronic, Radcliffe, Roche, Servier and Società Prodotti Antibiotici; and grants from Boston Scientific, Novartis and Pharmacosmos, unrelated to this Review. D.S. reports personal fees from GlaxoSmithKline, MSD and Novartis. L.H.L. reports personal fees from Abbott, Bayer, Lexicon, Medscape, Merck, Myokardia, Pharmacosmos, Radcliffe Cardiology and Sanofi; grants and personal fees from AstraZeneca, Boehringer Ingelheim, Novartis and Vifor–Fresenius; and grants from Boston Scientific, unrelated to this Review. G. Sinagra declares no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks B. A. Borlaug, W. J. Paulus and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Savarese, G., Stolfo, D., Sinagra, G. et al. Heart failure with mid-range or mildly reduced ejection fraction. Nat Rev Cardiol 19, 100–116 (2022). https://doi.org/10.1038/s41569-021-00605-5
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-021-00605-5
This article is cited by
-
Prognostic significance of right ventricular–pulmonary artery coupling assessed by TAPSE/PASP ratio in patients with HFmrEF
Heart and Vessels (2026)
-
Prevalence and prognosis of multimorbidity in heart failure with mildly reduced ejection fraction
Clinical Research in Cardiology (2026)
-
Advances in natural compounds modulating autophagy for the therapeutic intervention of heart failure
Molecular and Cellular Biochemistry (2026)
-
The global, regional, and National burden of severe heart failure (SHF) due to intracerebral hemorrhage, ischemic heart disease, or stroke, 1990–2021: a systematic analysis for the global burden of disease study 2021
BMC Cardiovascular Disorders (2025)
-
Heart failure types and predictors of 30-day rehospitalisation among patients aged ≥ 60 years with acute heart failure: a multicentre prospective study in Vietnam
BMC Cardiovascular Disorders (2025)