Abstract
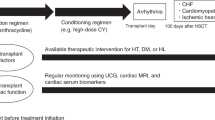
Anthracyclines are the cornerstone of treatment for many malignancies. However, anthracycline cardiotoxicity is a considerable concern given that it can compromise the clinical effectiveness of the treatment and patient survival despite early discontinuation of therapy or dose reduction. Patients with cancer receiving anthracycline treatment can have a reduction in their quality of life and likelihood of survival due to cardiotoxicity, irrespective of their oncological prognosis. Increasing knowledge about anthracycline cardiotoxicity has enabled the identification of patients who are candidates for anthracycline regimens and those who might develop anthracycline-induced cardiomyopathy. Anthracycline cardiotoxicity is a unique and evolving phenomenon that begins with myocardial cell damage, progresses to reduced left ventricular ejection fraction, and culminates in symptomatic heart failure if it is not promptly detected and treated. Early risk stratification can be guided by imaging or biomarkers. In this Review, we present a comprehensive and clinically useful approach to cardiomyopathy related to anthracycline therapy, encompassing its epidemiology, definition, mechanisms, novel classifications, risk factors and patient risk stratification, diagnostic approaches (including imaging and biomarkers), treatment guidelines algorithms, and the role of new cardioprotective drugs that are used for the treatment of heart failure.
Key points
-
Anthracycline cardiotoxicity is a complex phenomenon that evolves over time, involving not only cardiomyocytes but also other components of myocardial tissue.
-
A complete and accurate risk stratification before the initiation of anthracycline therapy, including risk scores, echocardiographic evaluation and cardiac biomarkers, is essential to define the subsequent surveillance and treatment protocol.
-
A multidisciplinary approach actively involving the oncologist and cardiologist is essential to plan a patient’s therapeutic and preventive choices.
-
Although the treatment options for patients who develop heart failure after anthracycline therapy are well defined, the appropriate treatment approaches for primary and secondary prevention in patients who develop subclinical cardiotoxicity are uncertain.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Octavia, Y. et al. Doxorubicin-induced cardiomyopathy: from molecular mechanisms to therapeutic strategies. J. Mol. Cell Cardiol. 52, 1213–1225 (2012).
Henriksen, P. A. Anthracycline cardiotoxicity: an update on mechanisms, monitoring and prevention. Heart 104, 971–977 (2018).
Zamorano, J. L. et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 37, 2768–2801 (2016).
Armenian, S. H. et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 16, e123–e136 (2015).
Lyon, A. R. et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 43, 4229–4361 (2022).
Dimarco, A. et al. ‘Daunomycin’, a new antibiotic of the rhodomycin group. Nature 201, 706–707 (1964).
Dubost, M. et al. A new antibiotic with cytostatic properties: rubidomycin [French]. C. R. Hebd. Seances Acad. Sci. 257, 1813–1815 (1963).
Minotti, G., Menna, P., Salvatorelli, E., Cairo, G. & Gianni, L. Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol. Rev. 56, 185–229 (2004).
Rawat, P. S., Jaiswal, A., Khurana, A., Bhatti, J. S. & Navik, U. Doxorubicin-induced cardiotoxicity: an update on the molecular mechanism and novel therapeutic strategies for effective management. Biomed. Pharmacother. 139, 111708 (2021).
Tan, C., Tasaka, H., Yu, K.-P., Murphy, M. L. & Karnofsky, D. A. Daunomycin, an antitumor antibiotic, in the treatment of neoplastic disease. Clinical evaluation with special reference to childhood leukemia. Cancer 20, 333–353 (1967).
Middleman, E., Luce, J. & Frei, E. Clinical trials with adriamycin. Cancer 28, 844–850 (1971).
Swain, S. M., Whaley, F. S. & Ewer, M. S. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer 97, 2869–2879 (2003).
Arcamone, F. et al. Synthesis and antitumor activity of 4-demethoxydaunorubicin, 4-demethoxy-7,9-diepidaunorubicin, and their beta anomers. Cancer Treat. Rep. 60, 829–834 (1976).
Danesi, R., Fogli, S., Gennari, A., Conte, P. & Del Tacca, M. Pharmacokinetic-pharmacodynamic relationships of the anthracycline anticancer drugs. Clin. Pharmacokinet. 41, 431–444 (2002).
Jain, K. K. et al. A prospective randomized comparison of epirubicin and doxorubicin in patients with advanced breast cancer. J. Clin. Oncol. 3, 818–826 (1985).
Ryberg, M. et al. Epirubicin cardiotoxicity: an analysis of 469 patients with metastatic breast cancer. J. Clin. Oncol. 16, 3502–3508 (1998).
Toffoli, G. et al. Dose-finding and pharmacologic study of chronic oral idarubicin therapy in metastatic breast cancer patients. Clin. Cancer Res. 6, 2279–2287 (2000).
Anderlini, P. et al. Idarubicin cardiotoxicity: a retrospective study in acute myeloid leukemia and myelodysplasia. J. Clin. Oncol. 13, 2827–2834 (1995).
Ichikawa, Y. et al. Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation. J. Clin. Invest. 124, 617–630 (2014).
Marinello, J., Delcuratolo, M. & Capranico, G. Anthracyclines as topoisomerase II poisons: from early studies to new perspectives. IJMS 19, 3480 (2018).
Qiu, Y., Jiang, P. & Huang, Y. Anthracycline-induced cardiotoxicity: mechanisms, monitoring, and prevention. Front. Cardiovasc. Med. 10, 1242596 (2023).
Zhang, S. et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat. Med. 18, 1639–1642 (2012).
Chatterjee, K., Zhang, J., Honbo, N. & Karliner, J. S. Doxorubicin cardiomyopathy. Cardiology 115, 155–162 (2010).
Fang, X. et al. Ferroptosis as a target for protection against cardiomyopathy. Proc. Natl Acad. Sci. USA 116, 2672–2680 (2019).
Amgalan, D. et al. A small-molecule allosteric inhibitor of BAX protects against doxorubicin-induced cardiomyopathy. Nat. Cancer 1, 315–328 (2020).
Li, M. et al. Phosphoinositide 3-kinase gamma inhibition protects from anthracycline cardiotoxicity and reduces tumor growth. Circulation 138, 696–711 (2018).
Cappetta, D. et al. Doxorubicin targets multiple players: a new view of an old problem. Pharmacol. Res. 127, 4–14 (2018).
Cardinale, D., Iacopo, F. & Cipolla, C. M. Cardiotoxicity of anthracyclines. Front. Cardiovasc. Med. 7, 26 (2020).
Cardinale, D., Biasillo, G. & Cipolla, C. M. Curing cancer, saving the heart: a challenge that cardioncology should not miss. Curr. Cardiol. Rep. 18, 51 (2016).
Franco, V. I., Henkel, J. M., Miller, T. L. & Lipshultz, S. E. Cardiovascular effects in childhood cancer survivors treated with anthracyclines. Cardiol. Res. Pract. 2011, 134679 (2011).
Pinder, M. C., Duan, Z., Goodwin, J. S., Hortobagyi, G. N. & Giordano, S. H. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J. Clin. Oncol. 25, 3808–3815 (2007).
Harbeck, N., Ewer, M. S., De Laurentiis, M., Suter, T. M. & Ewer, S. M. Cardiovascular complications of conventional and targeted adjuvant breast cancer therapy. Ann. Oncol. 22, 1250–1258 (2011).
Cardinale, D., Biasillo, G., Salvatici, M., Sandri, M. T. & Cipolla, C. M. Using biomarkers to predict and to prevent cardiotoxicity of cancer therapy. Exp. Rev. Mol. Diagn. 17, 245–256 (2017).
Pocock, S. J. et al. Predictors of mortality and morbidity in patients with chronic heart failure. Eur. Heart J. 27, 65–75 (2006).
Mertens, A. C. et al. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. J. Clin. Oncol. 19, 3163–3172 (2001).
Mulrooney, D. A. et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 339, b4606 (2009).
Reulen, R. C. Long-term cause-specific mortality among survivors of childhood cancer. JAMA 304, 172–179 (2010).
Semeraro, G. C., Lamantia, G., Cipolla, C. M. & Cardinale, D. How to identify anthracycline-induced cardiotoxicity early and reduce its clinical impact in everyday practice. Kardiol. Pol. 79, 114–122 (2021).
Cardinale, D. et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 131, 1981–1988 (2015).
Giantris, A., Abdurrahman, L., Hinkle, A., Asselin, B. & Lipshultz, S. E. Anthracycline-induced cardiotoxicity in children and young adults. Crit. Rev. Oncol. Hematol. 27, 53–68 (1998).
Grenier, M. A. & Lipshultz, S. E. Epidemiology of anthracycline cardiotoxicity in children and adults. Semin. Oncol. 25, 72–85 (1998).
Jain, D., Russell, R. R., Schwartz, R. G., Panjrath, G. S. & Aronow, W. Cardiac complications of cancer therapy: pathophysiology, identification, prevention, treatment, and future directions. Curr. Cardiol. Rep. 19, 36 (2017).
Ferrans, V. J. Overview of cardiac pathology in relation to anthracycline cardiotoxicity. Cancer Treat. Rep. 62, 955–961 (1978).
Cai, F. et al. Anthracycline-induced cardiotoxicity in the chemotherapy treatment of breast cancer: preventive strategies and treatment. Mol. Clin. Oncol. 11, 15–23 (2019).
Berry, G. J. & Jorden, M. Pathology of radiation and anthracycline cardiotoxicity. Pediatr. Blood Cancer 44, 630–637 (2005).
Cardinale, D. et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 109, 2749–2754 (2004).
McDonagh, T. A. et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42, 3599–3726 (2021).
Rossello, X. et al. Risk prediction tools in cardiovascular disease prevention: a report from the ESC Prevention of CVD Programme led by the European Association of Preventive Cardiology (EAPC) in collaboration with the Acute Cardiovascular Care Association (ACCA) and the Association of Cardiovascular Nursing and Allied Professions (ACNAP). Eur. J. Prev. Cardiol. 26, 1534–1544 (2019).
Lyon, A. R. et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the Cardio‐Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio‐Oncology Society. Eur. J. Heart Fail. 22, 1945–1960 (2020).
Rivero-Santana, B. et al. Anthracycline-induced cardiovascular toxicity: validation of the Heart Failure Association and International Cardio-Oncology Society risk score. Eur. Heart J. 46, 273–284 (2024).
Kaboré, E. G. et al. Risk prediction models for cardiotoxicity of chemotherapy among patients with breast cancer: a systematic review. JAMA Netw. Open. 6, e230569 (2023).
Salz, T. et al. Preexisting cardiovascular risk and subsequent heart failure among non-Hodgkin lymphoma survivors. J. Clin. Oncol. 35, 3837–3843 (2017).
Wang, L. et al. Major cardiac events and the value of echocardiographic evaluation in patients receiving anthracycline-based chemotherapy. Am. J. Cardiol. 116, 442–446 (2015).
Araujo-Gutierrez, R. et al. Baseline global longitudinal strain predictive of anthracycline-induced cardiotoxicity. Cardiooncology 7, 4 (2021).
Charbonnel, C. et al. Assessment of global longitudinal strain at low-dose anthracycline-based chemotherapy, for the prediction of subsequent cardiotoxicity. Eur. Heart J. Cardiovasc. Imaging 18, 392–401 (2017).
Neilan, T. G. et al. Left ventricular mass in patients with a cardiomyopathy after treatment with anthracyclines. Am. J. Cardiol. 110, 1679–1686 (2012).
Garrone, O. et al. Prediction of anthracycline cardiotoxicity after chemotherapy by biomarkers kinetic analysis. Cardiovasc. Toxicol. 12, 135–142 (2012).
Cardinale, D. et al. Left ventricular dysfunction predicted by early troponin I release after high-dose chemotherapy. J. Am. Coll. Cardiol. 36, 517–522 (2000).
Cardinale, D. et al. Myocardial injury revealed by plasma troponin I in breast cancer treated with high-dose chemotherapy. Ann. Oncol. 13, 710–715 (2002).
Ky, B. et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in patients with breast cancer treated with doxorubicin, taxanes, and trastuzumab. J. Am. Coll. Cardiol. 63, 809–816 (2014).
Sandri, M. T. et al. N-terminal pro-B-type natriuretic peptide after high-dose chemotherapy: a marker predictive of cardiac dysfunction? Clin. Chem. 51, 1405–1410 (2005).
Inoue, K. et al. Early detection and prediction of anthracycline-induced cardiotoxicity: a prospective cohort study. Circ. J. 88, 751–759 (2024).
McMurray, J. J. V. et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 33, 1787–1847 (2012).
Plana, J. C., Thavendiranathan, P., Bucciarelli-Ducci, C. & Lancellotti, P. Multi-modality imaging in the assessment of cardiovascular toxicity in the cancer patient. JACC Cardiovasc. Imaging 11, 1173–1186 (2018).
Dobson, R. et al. BSE and BCOS guideline for transthoracic echocardiographic assessment of adult cancer patients receiving anthracyclines and/or trastuzumab. JACC CardioOncol. 3, 1–16 (2021).
Romond, E. H. et al. Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel (ACP) with ACP plus trastuzumab as adjuvant therapy for patients with node-positive, human epidermal growth factor receptor 2–positive breast cancer. J. Clin. Oncol. 30, 3792–3799 (2012).
Zagar, T. M., Cardinale, D. M. & Marks, L. B. Breast cancer therapy-associated cardiovascular disease. Nat. Rev. Clin. Oncol. 13, 172–184 (2016).
Ewer, M. S. & Ewer, S. M. Cardiotoxicity of anticancer treatments. Nat. Rev. Cardiol. 12, 547–558 (2015).
Mousavi, N. et al. Echocardiographic parameters of left ventricular size and function as predictors of symptomatic heart failure in patients with a left ventricular ejection fraction of 50–59% treated with anthracyclines. Eur. Heart J. Cardiovasc. Imaging 16, 977–984 (2015).
Oikonomou, E. K. et al. Assessment of prognostic value of left ventricular global longitudinal strain for early prediction of chemotherapy-induced cardiotoxicity: a systematic review and meta-analysis. JAMA Cardiol. 4, 1007–1018 (2019).
Negishi, T. et al. Cardioprotection using strain-guided management of potentially cardiotoxic cancer therapy. JACC Cardiovasc. Imaging 16, 269–278 (2023).
Laufer-Perl, M. et al. Left atrial strain changes in patients with breast cancer during anthracycline therapy. Int. J. Cardiol. 330, 238–244 (2021).
Emerson, P. et al. Left atrial strain in cardiac surveillance of bone marrow transplant patients with prior anthracycline exposure. Int. J. Cardiol. 354, 68–74 (2022).
Michel, L. et al. Troponins and brain natriuretic peptides for the prediction of cardiotoxicity in cancer patients: a meta‐analysis. Eur. J. Heart Fail. 22, 350–361 (2020).
Fabiani, I. et al. Use of new and emerging cancer drugs: what the cardiologist needs to know. Eur. Heart J. 45, 1971–1987 (2024).
O’Brien, P. J. Cardiac troponin is the most effective translational safety biomarker for myocardial injury in cardiotoxicity. Toxicology 245, 206–218 (2008).
Apple, F. S. & Collinson, P. O. Analytical characteristics of high-sensitivity cardiac troponin assays. Clin. Chem. 58, 54–61 (2012).
Tan, L.-L. & Lyon, A. R. Role of biomarkers in prediction of cardiotoxicity during cancer treatment. Curr. Treat. Options Cardio Med. 20, 55 (2018).
Pudil, R. et al. Role of serum biomarkers in cancer patients receiving cardiotoxic cancer therapies: a position statement from the Cardio‐Oncology Study Group of the Heart Failure Association and the Cardio‐Oncology Council of the European Society of Cardiology. Eur. J. Heart Fail. 22, 1966–1983 (2020).
Sawaya, H. et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ. Cardiovasc. Imaging 5, 596–603 (2012).
Skovgaard, D., Hasbak, P. & Kjaer, A. BNP predicts chemotherapy-related cardiotoxicity and death: comparison with gated equilibrium radionuclide ventriculography. PLoS ONE 9, e96736 (2014).
Fallah-Rad, N. et al. The utility of cardiac biomarkers, tissue velocity and strain imaging, and cardiac magnetic resonance imaging in predicting early left ventricular dysfunction in patients with human epidermal growth factor receptor II-positive breast cancer treated with adjuvant trastuzumab therapy. J. Am. Coll. Cardiol. 57, 2263–2270 (2011).
Cardinale, D. et al. Anthracycline-induced cardiomyopathy. J. Am. Coll. Cardiol. 55, 213–220 (2010).
Gongora, C. A. et al. Are sodium-glucose cotransporter-2 inhibitors the cherry on top of cardio-oncology care? Cardiovasc. Drugs Ther. https://doi.org/10.1007/s10557-024-07604-x (2024).
Khouri, M. G. & Greene, S. J. Sodium-glucose co-transporter-2 inhibitor therapy during anthracycline treatment. JACC Heart Fail. 10, 568–570 (2022).
Camilli, M. et al. Sodium–glucose cotransporter 2 inhibitors and the cancer patient: from diabetes to cardioprotection and beyond. Basic. Res. Cardiol. https://doi.org/10.1007/s00395-024-01059-9 (2024).
Giangiacomi, F. et al. Case report: sodium-glucose cotransporter 2 inhibitors induce left ventricular reverse remodeling in anthracycline-related cardiac dysfunction – a case series. Front. Cardiovasc. Med. 10, 1250185 (2023).
López-Sendón, J. et al. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: the CARDIOTOX registry. Eur. Heart J. 41, 1720–1729 (2020).
Ferdinandy, P. et al. Definition of hidden drug cardiotoxicity: paradigm change in cardiac safety testing and its clinical implications. Eur. Heart J. 40, 1771–1777 (2019).
Hensley, M. L. et al. American Society of Clinical Oncology 2008 clinical practice guideline update: use of chemotherapy and radiation therapy protectants. J. Clin. Oncol. 27, 127–145 (2009).
Swain, S. M. et al. Cardioprotection with dexrazoxane for doxorubicin-containing therapy in advanced breast cancer. J. Clin. Oncol. 15, 1318–1332 (1997).
Tebbi, C. K. et al. Dexrazoxane-associated risk for acute myeloid leukemia/myelodysplastic syndrome and other secondary malignancies in pediatric Hodgkin’s disease. J. Clin. Oncol. 25, 493–500 (2007).
Van Dalen, E. C., Caron, H. N., Dickinson, H. O. & Kremer, L. C. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst. Rev. 2011, CD003917 (2011).
Vejpongsa, P. & Yeh, E. T. H. Prevention of anthracycline-induced cardiotoxicity. J. Am. Coll. Cardiol. 64, 938–945 (2014).
Zheng, H. & Zhan, H. Preventing anthracycline-associated heart failure: what is the role of dexrazoxane?: JACC: CardioOncology Controversies in Cardio-Oncology. JACC CardioOncol. 6, 318–321 (2024).
De Baat, E. C. et al. Dexrazoxane for preventing or reducing cardiotoxicity in adults and children with cancer receiving anthracyclines. Cochrane Database Syst. Rev. 9, CD014638 (2022).
Omland, T., Heck, S. L. & Gulati, G. The role of cardioprotection in cancer therapy cardiotoxicity. JACC CardioOncol. 4, 19–37 (2022).
Cardinale, D. et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation 114, 2474–2481 (2006).
Bosch, X. et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies. J. Am. Coll. Cardiol. 61, 2355–2362 (2013).
Georgakopoulos, P. et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin‐treated lymphoma patients: a prospective, parallel‐group, randomized, controlled study with 36‐month follow‐up. Am. J. Hematol. 85, 894–896 (2010).
Kalay, N. et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J. Am. Coll. Cardiol. 48, 2258–2262 (2006).
Gulati, G. et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur. Heart J. 37, 1671–1680 (2016).
Avila, M. S. et al. Carvedilol for prevention of chemotherapy-related cardiotoxicity: the CECCY trial. J. Am. Coll. Cardiol. 71, 2281–2290 (2018).
Cardinale, D. et al. Anthracycline-induced cardiotoxicity: a multicenter randomised trial comparing two strategies for guiding prevention with enalapril: the International CardioOncology Society-one trial. Eur. J. Cancer 94, 126–137 (2018).
Avila, M. S. et al. Renin-angiotensin system antagonists and beta-blockers in prevention of anthracycline cardiotoxicity: a systematic review and meta-analysis. Arq. Bras. Cardiol. 120, e20220298 (2023).
Caspani, F. et al. Prevention of anthracycline-induced cardiotoxicity: a systematic review and meta-analysis. Intern. Emerg. Med. 16, 477–486 (2021).
Neilan, T. G. et al. Atorvastatin for anthracycline-associated cardiac dysfunction: the STOP-CA randomized clinical trial. JAMA 330, 528 (2023).
Hundley, W. G. et al. Statins and left ventricular ejection fraction following doxorubicin treatment. NEJM Evid. https://doi.org/10.1056/evidoa2200097 (2022).
Thavendiranathan, P. et al. Statins to prevent early cardiac dysfunction in cancer patients at increased cardiotoxicity risk receiving anthracyclines. Eur. Heart J. Cardiovasc. Pharmacother. 9, 515–525 (2023).
Anker, S. D. et al. Empagliflozin in heart failure with a preserved ejection fraction. N. Engl. J. Med. 385, 1451–1461 (2021).
Abdel-Qadir, H. et al. The association of sodium–glucose cotransporter 2 inhibitors with cardiovascular outcomes in anthracycline-treated patients with cancer. JACC CardioOncol. 5, 318–328 (2023).
Gongora, C. A. et al. Sodium–glucose co-transporter-2 inhibitors and cardiac outcomes among patients treated with anthracyclines. JACC Heart Fail. 10, 559–567 (2022).
Daniele, A. J., Gregorietti, V., Costa, D. & López – Fernández, T. Use of EMPAgliflozin in the prevention of CARDiotoxicity: the EMPACARD – PILOT trial. Cardiooncology 10, 58 (2024).
Rafiyath, S. M. et al. Comparison of safety and toxicity of liposomal doxorubicin vs. conventional anthracyclines: a meta-analysis. Exp. Hematol. Oncol. 1, 10 (2012).
Harris, L. et al. Liposome‐encapsulated doxorubicin compared with conventional doxorubicin in a randomized multicenter trial as first‐line therapy of metastatic breast carcinoma. Cancer 94, 25–36 (2002).
Gabizon, A., Shmeeda, H. & Barenholz, Y. Pharmacokinetics of pegylated liposomal doxorubicin: review of animal and human studies. Clin. Pharmacokinet. 42, 419–436 (2003).
Berkman, A. M., Hildebrandt, M. A. T. & Landstrom, A. P. The genetic underpinnings of anthracycline‐induced cardiomyopathy predisposition. Clin. Genet. 100, 132–143 (2021).
Leong, S. L., Chaiyakunapruk, N. & Lee, S. W. H. Candidate gene association studies of anthracycline-induced cardiotoxicity: a systematic review and meta-analysis. Sci. Rep. 7, 39 (2017).
Schneider, B. P. et al. Genome-wide association study for anthracycline-induced congestive heart failure. Clin. Cancer Res. 23, 43–51 (2017).
Wang, X. et al. Genome-wide association study identifies ROBO2 as a novel susceptibility gene for anthracycline-related cardiomyopathy in childhood cancer survivors. J. Clin. Oncol. 41, 1758–1769 (2023).
Aminkeng, F. et al. Recommendations for genetic testing to reduce the incidence of anthracycline‐induced cardiotoxicity. Brit J. Clin. Pharmacol. 82, 683–695 (2016).
Liu, J. et al. Circulating hemopexin modulates anthracycline cardiac toxicity in patients and in mice. Sci. Adv. 8, eadc9245 (2022).
Jacobs, J. E. J. et al. Artificial intelligence electrocardiogram as a novel screening tool to detect a newly abnormal left ventricular ejection fraction after anthracycline-based cancer therapy. Eur. J. Prev. Cardiol. 31, 560–566 (2024).
Kwan, J. M., Oikonomou, E. K., Henry, M. L. & Sinusas, A. J. Multimodality advanced cardiovascular and molecular imaging for early detection and monitoring of cancer therapy-associated cardiotoxicity and the role of artificial intelligence and big data. Front. Cardiovasc. Med. 9, 829553 (2022).
Chang, W.-T. et al. An artificial intelligence approach for predicting cardiotoxicity in breast cancer patients receiving anthracycline. Arch. Toxicol. 96, 2731–2737 (2022).
Porter, C. et al. Permissive cardiotoxicity; the clinical crucible of cardio-oncology. JACC CardioOncol. 4, 302–312 (2022).
Liutkauskiene, S. et al. Retrospective analysis of the impact of anthracycline dose reduction and chemotherapy delays on the outcomes of early breast cancer molecular subtypes. BMC Cancer 18, 453 (2018).
Author information
Authors and Affiliations
Contributions
I.F. and M.C. wrote the manuscript. All the authors reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Aarti Asnani, Susan Dent and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fabiani, I., Chianca, M., Cipolla, C.M. et al. Anthracycline-induced cardiomyopathy: risk prediction, prevention and treatment. Nat Rev Cardiol 22, 551–563 (2025). https://doi.org/10.1038/s41569-025-01126-1
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-025-01126-1
This article is cited by
-
Heart failure in patients with acute myeloid leukemia (AML) treated with anthracycline agents during remission induction therapy: a systematic review and meta-analysis
Leukemia (2026)
-
Beyond ejection fraction: cardiac magnetic resonance imaging in anthracycline cardiotoxicity
BMC Medical Imaging (2025)
-
CT-derived myosteatosis for baseline risk stratification of cardiotoxicity in patients with diffuse large B-cell lymphoma receiving anthracyclines
BMC Medical Imaging (2025)
-
Doxorubicin cardiotoxicity is mediated by neutrophil extracellular traps
Nature Cancer (2025)
-
Cardiomyocyte-localized CCDC25 senses NET DNA to promote doxorubicin cardiotoxicity by activating autophagic flux
Nature Cancer (2025)