Abstract
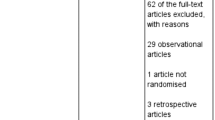
Heart failure is a leading cause of hospitalization worldwide, and congestion is the predominant cause of heart failure symptoms and hospitalization. The primary therapy used to treat and prevent congestion has historically been loop diuretics. However, many patients are discharged from hospital with residual congestion, which is associated with persistent heart failure symptoms, adverse outcomes and hospital readmission. Multiple medical strategies and devices have been and are being investigated with the aim of improving decongestion and subsequent heart failure outcomes. Numerous questions exist about the design of clinical trials to test emerging medical and device therapies, including the magnitude of benefit on congestive, kidney and post-discharge outcomes relative to conventional decongestion practices, and how best to implement novel therapies. In this Review, we discuss emerging medical and device strategies targeting congestion in patients with heart failure.
Key points
-
Various medical and device strategies are under investigation to overcome barriers that limit decongestion in patients with acute decompensated heart failure.
-
Medical strategies that optimize the use of existing diuretic therapies could have immediate, systemic effects on heart failure treatment, with limited risk or cost.
-
Most devices under investigation are designed to improve the diuretic response indirectly by targeting a hypothesized haemodynamic mechanism; however, mechanistic data and clinical trials of drugs indicate that improving haemodynamics might have limited benefit.
-
Barriers to the implementation of invasive devices include increased rates of adverse events from invasive procedures, cost, resource utilization and the requirement for provider expertise, limiting the pool of candidate patients.
-
Randomized, controlled trials are needed to determine whether invasive devices can sufficiently improve decongestion and post-discharge outcomes compared with optimized medical therapy to offset their inherent risks and numerous barriers to widespread implementation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bozkurt, B. et al. Heart failure epidemiology and outcomes statistics: a report of the Heart Failure Society of America. J. Card. Fail. 29, 1412–1451 (2023).
Clark, K. A. A. et al. Trends in heart failure hospitalizations in the US from 2008 to 2018. J. Card. Fail. 28, 171–180 (2022).
Chioncel, O. et al. Acute heart failure congestion and perfusion status — impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA Heart Failure Long-Term Registry. Eur. J. Heart Fail. 21, 1338–1352 (2019).
Hollenberg, S. M. et al. 2019 ACC Expert Consensus Decision Pathway on risk assessment, management, and clinical trajectory of patients hospitalized with heart failure: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 74, 1966–2011 (2019).
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 79, e263–e421 (2022).
Boorsma, E. M. et al. Congestion in heart failure: a contemporary look at physiology, diagnosis and treatment. Nat. Rev. Cardiol. 17, 641–655 (2020).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 24, 4–131 (2022).
Ambrosy, A. P. et al. Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: findings from the EVEREST trial. Eur. Heart J. 34, 835–843 (2013).
Testani, J. M., Chen, J., McCauley, B. D., Kimmel, S. E. & Shannon, R. P. Potential effects of aggressive decongestion during the treatment of decompensated heart failure on renal function and survival. Circulation 122, 265–272 (2010).
Girerd, N. et al. Integrative assessment of congestion in heart failure throughout the patient journey. JACC Heart Fail. 6, 273–285 (2018).
Testani, J. M. et al. Substantial discrepancy between fluid and weight loss during acute decompensated heart failure treatment. Am. J. Med. 128, 776–783.e4 (2015).
Cox, Z. L. & Testani, J. M. Loop diuretic resistance complicating acute heart failure. Heart Fail. Rev. 25, 133–145 (2020).
Felker, G. M., Ellison, D. H., Mullens, W., Cox, Z. L. & Testani, J. M. Diuretic therapy for patients with heart failure: JACC state-of-the-art review. J. Am. Coll. Cardiol. 75, 1178–1195 (2020).
Cox, Z. L. & Lenihan, D. J. Loop diuretic resistance in heart failure: resistance etiology-based strategies to restoring diuretic efficacy. J. Card. Fail. 20, 611–622 (2014).
Greene, S. J. et al. In-hospital therapy for heart failure with reduced ejection fraction in the United States. JACC Heart Fail. 8, 943–953 (2020).
Metra, M. et al. Prognostic significance of creatinine increases during an acute heart failure admission in patients with and without residual congestion: a post hoc analysis of the PROTECT Data. Circ. Heart Fail. 11, e004644 (2018).
Damman, K. et al. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur. Heart J. 35, 455–469 (2014).
Zheng, J. et al. Contemporary decongestion strategies in patients hospitalized for heart failure: a National Community-Based Cohort Study. JACC Heart Fail. 12, 1381–1392 (2024).
Zheng, J. et al. Inpatient use of guideline-directed medical therapy during heart failure hospitalizations among community-based health systems. JACC Heart Fail. 13, 43–54 (2025).
Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA 287, 1531–1540 (2002).
Mebazaa, A. et al. The impact of early standard therapy on dyspnoea in patients with acute heart failure: the URGENT-dyspnoea study. Eur. Heart J. 31, 832–841 (2010).
Mullens, W. et al. The use of diuretics in heart failure with congestion — a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21, 137–155 (2019).
Gheorghiade, M. et al. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur. J. Heart Fail. 12, 423–433 (2010).
Stevenson, L. W. & Perloff, J. K. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA 261, 884–888 (1989).
Drazner, M. H. et al. Value of clinician assessment of hemodynamics in advanced heart failure: the ESCAPE trial. Circ. Heart Fail. 1, 170–177 (2008).
Elder, A., Japp, A. & Verghese, A. How valuable is physical examination of the cardiovascular system? BMJ 354, i3309 (2016).
Chakko, S. et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am. J. Med. 90, 353–359 (1991).
Binanay, C. et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA 294, 1625–1633 (2005).
Stienen, S. et al. NT-proBNP (N-Terminal pro-B-Type Natriuretic Peptide)-guided therapy in acute decompensated heart failure: PRIMA II randomized controlled trial (can NT-ProBNP-guided therapy during hospital admission for acute decompensated heart failure reduce mortality and readmissions?). Circulation 137, 1671–1683 (2018).
Lala, A. et al. Standardized definitions for evaluation of acute decompensated heart failure therapies: HF-ARC expert panel paper. JACC Heart Fail. 12, 1–15 (2024).
Georges, G., Fudim, M., Burkhoff, D., Leon, M. & Genereux, P. Patient selection and end point definitions for decongestion studies in acute decompensated heart failure: part 2. J. Soc. Cardiovasc. Angiogr. Interv. 2, 101059 (2023).
Felker, G. M. et al. Diuretic strategies in patients with acute decompensated heart failure. N. Engl. J. Med. 364, 797–805 (2011).
Bart, B. A. et al. Cardiorenal rescue study in acute decompensated heart failure: rationale and design of CARRESS-HF, for the Heart Failure Clinical Research Network. J. Card. Fail. 18, 176–182 (2012).
Mullens, W. et al. Acetazolamide in acute decompensated heart failure with volume overload. N. Engl. J. Med. 387, 1185–1195 (2022).
Bart, B. A. et al. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N. Engl. J. Med. 367, 2296–2304 (2012).
Ter Maaten, J. M. et al. Natriuresis-guided diuretic therapy in acute heart failure: a pragmatic randomized trial. Nat. Med. 29, 2625–2632 (2023).
Trulls, J. C. et al. Combining loop with thiazide diuretics for decompensated heart failure: the CLOROTIC trial. Eur. Heart J. 44, 411–421 (2023).
Kapur, N. K. et al. Intermittent occlusion of the superior vena cava to improve hemodynamics in patients with acutely decompensated heart failure: the VENUS-HF Early Feasibility Study. Circ. Heart Fail. 15, e008934 (2022).
Zymlinski, R. et al. Safety, feasibility of controllable decrease of vena cava pressure by Doraya catheter in heart failure. JACC Basic Transl. Sci. 8, 394–402 (2023).
Cowger, J. A. et al. Safety and performance of the aortix device in acute decompensated heart failure and cardiorenal syndrome. JACC Heart Fail. 11, 1565–1575 (2023).
Georges, G. et al. First-in-human experience with the ModulHeart device for mechanical circulatory support and renal perfusion. J. Soc. Cardiovasc. Angiogr. Interv. 1, 100449 (2022).
Keeble, T. R. et al. Percutaneous haemodynamic and renal support in patients presenting with decompensated heart failure: a multi-centre efficacy study using the Reitan Catheter Pump (RCP). Int. J. Cardiol. 275, 53–58 (2019).
Galiwango, P. J., McReynolds, A., Ivanov, J., Chan, C. T. & Floras, J. S. Activity with ambulation attenuates diuretic responsiveness in chronic heart failure. J. Card. Fail. 17, 797–803 (2011).
Konstam, M. A. et al. Continuous aortic flow augmentation: a pilot study of hemodynamic and renal responses to a novel percutaneous intervention in decompensated heart failure. Circulation 112, 3107–3114 (2005).
Greenberg, B. et al. Effects of continuous aortic flow augmentation in patients with exacerbation of heart failure inadequately responsive to medical therapy: results of the Multicenter Trial of the Orqis Medical Cancion System for the Enhanced Treatment of Heart Failure Unresponsive to Medical Therapy (MOMENTUM). Circulation 118, 1241–1249 (2008).
Mullens, W. et al. Evaluation of kidney function throughout the heart failure trajectory — a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 22, 584–603 (2020).
Wettersten, N. et al. Decongestion discriminates risk for one-year mortality in patients with improving renal function in acute heart failure. Eur. J. Heart Fail. 23, 1122–1130 (2021).
Brisco, M. A. et al. Relevance of changes in serum creatinine during a heart failure trial of decongestive strategies: insights from the DOSE trial. J. Card. Fail. 22, 753–760 (2016).
Natov, P. S. et al. Improvement in renal function during the treatment of acute decompensated heart failure: relationship with markers of renal tubular injury and prognostic importance. Circ. Heart Fail. 16, e009776 (2023).
Testani, J. M., Kimmel, S. E., Dries, D. L. & Coca, S. G. Prognostic importance of early worsening renal function after initiation of angiotensin-converting enzyme inhibitor therapy in patients with cardiac dysfunction. Circ. Heart Fail. 4, 685–691 (2011).
Wettersten, N. et al. Short-term prognostic implications of serum and urine neutrophil gelatinase-associated lipocalin in acute heart failure: findings from the AKINESIS study. Eur. J. Heart Fail. 22, 251–263 (2020).
Adamson, C. et al. Initial decline (“dip”) in estimated glomerular filtration rate following initiation of dapagliflozin in patients with heart failure and reduced ejection fraction: insights from DAPA-HF. Circulation 146, 438–449 (2022).
Damman, K. et al. Clinical importance of urinary sodium excretion in acute heart failure. Eur. J. Heart Fail. 22, 1438–1447 (2020).
Hodson, D. Z. et al. Natriuretic response is highly variable and associated with 6-month survival: insights from the ROSE-AHF trial. JACC Heart Fail. 7, 383–391 (2019).
Biegus, J. et al. Renal profiling based on estimated glomerular filtration rate and spot urine sodium identifies high-risk acute heart failure patients. Eur. J. Heart Fail. 23, 729–739 (2021).
Martens, P. et al. Assessing intrinsic renal sodium avidity in acute heart failure: implications in predicting and guiding decongestion. Eur. J. Heart Fail. 24, 1978–1987 (2022).
Rao, V. S. et al. Natriuretic equation to predict loop diuretic response in patients with heart failure. J. Am. Coll. Cardiol. 77, 695–708 (2021).
Biegus, J. et al. The blunted loop diuretic response in acute heart failure is driven by reduced tubular responsiveness rather than insufficient tubular delivery. The role of furosemide urine excretion on diuretic and natriuretic response in acute heart failure. Eur. J. Heart Fail. 25, 1323–1333 (2023).
Christensen, S., Shalmi, M. & Petersen, J. S. Lithium clearance as an indicator of proximal tubular sodium handling during furosemide diuresis. J. Pharmacol. Exp. Ther. 246, 753–757 (1988).
Beutler, J. J., Boer, W. H., Koomans, H. A. & Dorhout Mees, E. J. Comparative study of the effects of furosemide, ethacrynic acid and bumetanide on the lithium clearance and diluting segment reabsorption in humans. J. Pharmacol. Exp. Ther. 260, 768–772 (1992).
Rao, V. S. et al. Compensatory distal reabsorption drives diuretic resistance in human heart failure. J. Am. Soc. Nephrol. 28, 3414–3424 (2017).
Cox, Z. L. et al. Compensatory post-diuretic renal sodium reabsorption is not a dominant mechanism of diuretic resistance in acute heart failure. Eur. Heart J. 42, 4468–4477 (2021).
Hollenberg, S. M. et al. 2024 ACC Expert Consensus Decision Pathway on clinical assessment, management, and trajectory of patients hospitalized with heart failure focused update: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 84, 1241–1267 (2024).
Cox, Z. L. et al. Efficacy and safety of dapagliflozin in patients with acute heart failure. J. Am. Coll. Cardiol. 83, 1295–1306 (2024).
Onishi, A. et al. A role for tubular Na+/H+ exchanger NHE3 in the natriuretic effect of the SGLT2 inhibitor empagliflozin. Am. J. Physiol. Ren. Physiol. 319, F712–F728 (2020).
Borges-Junior, F. A. et al. Empagliflozin inhibits proximal tubule NHE3 activity, preserves GFR, and restores euvolemia in nondiabetic rats with induced heart failure. J. Am. Soc. Nephrol. 32, 1616–1629 (2021).
Rao, V. S. et al. Empagliflozin in heart failure: regional nephron sodium handling effects. J. Am. Soc. Nephrol. 35, 189–201 (2024).
Bhatt, D. L. et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N. Engl. J. Med. 384, 117–128 (2021).
Griffin, M. et al. Empagliflozin in heart failure: diuretic and cardiorenal effects. Circulation 142, 1028–1039 (2020).
Doehner, W. et al. Uric acid and sodium-glucose cotransporter-2 inhibition with empagliflozin in heart failure with reduced ejection fraction: the EMPEROR-reduced trial. Eur. Heart J. 43, 3435–3446 (2022).
Felker, G. M. New decongestion strategies in an evolving heart failure landscape. N. Engl. J. Med. 387, 1231–1233 (2022).
Abbo, A. R. et al. Diuresis efficacy in ambulatory congested heart failure patients: intrapatient comparison of 3 diuretic regimens (DEA-HF). JACC Heart Fail. 12, 1396–1405 (2024).
Martens, P. et al. Pre-treatment bicarbonate levels and decongestion by acetazolamide: the ADVOR trial. Eur. Heart J. 44, 1995–2005 (2023).
Van den Eynde, J. et al. Serum chloride and the response to acetazolamide in patients with acute heart failure and volume overload: a post hoc analysis from the ADVOR trial. Circ. Heart Fail. 17, e011749 (2024).
Ter Maaten, J. M. et al. Renal tubular resistance is the primary driver for loop diuretic resistance in acute heart failure. Eur. J. Heart Fail. 19, 1014–1022 (2017).
Subramanya, A. R. & Ellison, D. H. Distal convoluted tubule. Clin. J. Am. Soc. Nephrol. 9, 2147–2163 (2014).
Ellison, D. H., Velazquez, H. & Wright, F. S. Adaptation of the distal convoluted tubule of the rat. Structural and functional effects of dietary salt intake and chronic diuretic infusion. J. Clin. Invest. 83, 113–126 (1989).
Jentzer, J. C., DeWald, T. A. & Hernandez, A. F. Combination of loop diuretics with thiazide-type diuretics in heart failure. J. Am. Coll. Cardiol. 56, 1527–1534 (2010).
Carta, F. & Supuran, C. T. Diuretics with carbonic anhydrase inhibitory action: a patent and literature review (2005 - 2013). Expert Opin. Ther. Pat. 23, 681–691 (2013).
Ern Yeoh, S. et al. Dapagliflozin versus metolazone in heart failure resistant to loop diuretics. Eur. Heart J. 44, 2966–2977 (2023).
Brisco-Bacik, M. A. et al. Outcomes associated with a strategy of adjuvant metolazone or high-dose loop diuretics in acute decompensated heart failure: a propensity analysis. J. Am. Heart Assoc. 7, e009149 (2018).
Pearce, D. et al. Collecting duct principal cell transport processes and their regulation. Clin. J. Am. Soc. Nephrol. 10, 135–146 (2015).
The RALES Investigators. Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study [RALES]). Am. J. Cardiol. 78, 902–907 (1996).
Butler, J. et al. Efficacy and safety of spironolactone in acute heart failure: the ATHENA-HF randomized clinical trial. JAMA Cardiol. 2, 950–958 (2017).
de Denus, S. et al. Spironolactone metabolite concentrations in decompensated heart failure: insights from the ATHENA-HF trial. Eur. J. Heart Fail. 22, 1451–1461 (2020).
Cox, Z. L., Hung, R., Lenihan, D. J. & Testani, J. M. Diuretic strategies for loop diuretic resistance in acute heart failure: the 3T trial. JACC Heart Fail. 8, 157–168 (2020).
Aliti, G. B. et al. Aggressive fluid and sodium restriction in acute decompensated heart failure: a randomized clinical trial. JAMA Intern. Med. 173, 1058–1064 (2013).
Liu, C. et al. Simultaneous use of hypertonic saline and IV furosemide for fluid overload: a systematic review and meta-analysis. Crit. Care Med. 49, e1163–e1175 (2021).
Cobo Marcos, M. et al. Efficacy and safety of hypertonic saline therapy in ambulatory patients with heart failure: the SALT-HF trial. Eur. J. Heart Fail. 26, 2118–2128 (2024).
Dauw, J. et al. Sodium loading in ambulatory patients with heart failure with reduced ejection fraction: mechanistic insights into sodium handling. Eur. J. Heart Fail. 26, 616–624 (2024).
Montgomery, R. A. et al. Oral sodium to preserve renal efficiency in acute heart failure: a randomized, placebo-controlled, double-blind study. J. Card. Fail. 29, 986–996 (2023).
Griffin, M. et al. Real world use of hypertonic saline in refractory acute decompensated heart failure: a U.S. Center’s Experience. JACC Heart Fail. 8, 199–208 (2020).
Mullens, W. et al. Dietary sodium and fluid intake in heart failure. A clinical consensus statement of the Heart Failure Association of the ESC. Eur. J. Heart Fail. 26, 730–741 (2024).
Cogswell, M. E. et al. Estimated 24-hour urinary sodium and potassium excretion in US adults. JAMA 319, 1209–1220 (2018).
Colin-Ramirez, E., Arcand, J. & Ezekowitz, J. A. Estimates of dietary sodium consumption in patients with chronic heart failure. J. Card. Fail. 21, 981–988 (2015).
Kotchen, T. A., Welch, W. J., Lorenz, J. N. & Ott, C. E. Renal tubular chloride and renin release. J. Lab. Clin. Med. 110, 533–540 (1987).
Briggs, J. P. & Schnermann, J. B. Whys and wherefores of juxtaglomerular apparatus function. Kidney Int. 49, 1724–1726 (1996).
Wesson, D. E. Glomerular filtration effects of acute volume expansion: importance of chloride. Kidney Int. 32, 238–245 (1987).
Subramanya, A. R., Yang, C. L., McCormick, J. A. & Ellison, D. H. WNK kinases regulate sodium chloride and potassium transport by the aldosterone-sensitive distal nephron. Kidney Int. 70, 630–634 (2006).
Ponce-Coria, J. et al. Regulation of NKCC2 by a chloride-sensing mechanism involving the WNK3 and SPAK kinases. Proc. Natl Acad. Sci. USA 105, 8458–8463 (2008).
Ter Maaten, J. M. et al. Hypochloremia, diuretic resistance, and outcome in patients with acute heart failure. Circ. Heart Fail. 9, e003109 (2016).
Grodin, J. L. et al. Implications of serum chloride homeostasis in acute heart failure (from ROSE-AHF). Am. J. Cardiol. 119, 78–83 (2017).
Hanberg, J. S. et al. Hypochloremia and diuretic resistance in heart failure: mechanistic insights. Circ. Heart Fail. 9, e003180 (2016).
Cox, Z. L. et al. Randomized controlled trial of urinE chemiStry guided aCute heArt faiLure treATmEnt (ESCALATE): rationale and design. Am. Heart J. 265, 121–131 (2023).
Cox, Z. L. et al. Multi-nephron segment diuretic therapy to overcome diuretic resistance in acute heart failure: a single-center experience. J. Card. Fail. 28, 21–31 (2022).
Ambrosy, A. P. et al. Body weight change during and after hospitalization for acute heart failure: patient characteristics, markers of congestion, and outcomes: findings from the ASCEND-HF trial. JACC Heart Fail. 5, 1–13 (2017).
Nijst, P. et al. The pathophysiological role of interstitial sodium in heart failure. J. Am. Coll. Cardiol. 65, 378–388 (2015).
Brinkley, D. M. Jr. et al. Spot urine sodium as triage for effective diuretic infusion in an ambulatory heart failure unit. J. Card. Fail. 24, 349–354 (2018).
Honda, S. et al. Long-term prognostic significance of urinary sodium concentration in patients with acute heart failure. Int. J. Cardiol. 254, 189–194 (2018).
Collins, S. P. et al. Early urine electrolyte patterns in patients with acute heart failure. ESC Heart Fail. 6, 80–88 (2019).
Luk, A. et al. First spot urine sodium after initial diuretic identifies patients at high risk for adverse outcome after heart failure hospitalization. Am. Heart J. 203, 95–100 (2018).
Biegus, J. et al. Serial assessment of spot urine sodium predicts effectiveness of decongestion and outcome in patients with acute heart failure. Eur. J. Heart Fail. 21, 624–633 (2019).
Dauw, J. et al. Protocolized natriuresis-guided decongestion improves diuretic response: the Multicenter ENACT-HF study. Circ. Heart Fail. 17, e011105 (2024).
Vanhentenrijk, S. et al. Rationale and design of the DECONGEST (Diuretic Treatment in Acute Heart Failure with Volume Overload Guided by Serial Spot Urine Sodium Assessment) study. J. Card. Fail. 31, 651–660 (2025).
Siddiqi, H. K. et al. The utility of urine sodium-guided diuresis during acute decompensated heart failure. Heart Fail. Rev. 29, 1161–1173 (2024).
Testani, J. M. et al. Rapid and highly accurate prediction of poor loop diuretic natriuretic response in patients with heart failure. Circ. Heart Fail. 9, e002370 (2016).
Iwanek, G. et al. Spot urine sodium-to-creatinine ratio surpasses sodium in identifying poor diuretic response in acute heart failure. ESC Heart Fail. 11, 3438–3442 (2024).
Chen, H. H. et al. Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial. JAMA 310, 2533–2543 (2013).
Cuffe, M. S. et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA 287, 1541–1547 (2002).
Gottlieb, S. S. et al. Effects of nesiritide and predictors of urine output in acute decompensated heart failure: results from ASCEND-HF (acute study of clinical effectiveness of nesiritide and decompensated heart failure). J. Am. Coll. Cardiol. 62, 1177–1183 (2013).
Packer, M. et al. Effect of ularitide on cardiovascular mortality in acute heart failure. N. Engl. J. Med. 376, 1956–1964 (2017).
Kozhuharov, N. et al. Effect of a strategy of comprehensive vasodilation vs usual care on mortality and heart failure rehospitalization among patients with acute heart failure: the GALACTIC randomized clinical trial. JAMA 322, 2292–2302 (2019).
Testani, J. M. et al. Loop diuretic efficiency: a metric of diuretic responsiveness with prognostic importance in acute decompensated heart failure. Circ. Heart Fail. 7, 261–270 (2014).
Eder, M. et al. The importance of forward flow and venous congestion in diuretic response in acute heart failure: insights from the ESCAPE trial. Int. J. Cardiol. 381, 57–61 (2023).
Voors, A. A. et al. Diuretic response in patients with acute decompensated heart failure: characteristics and clinical outcome — an analysis from RELAX-AHF. Eur. J. Heart Fail. 16, 1230–1240 (2014).
ter Maaten, J. M. et al. Diuretic response in acute heart failure-an analysis from ASCEND-HF. Am. Heart J. 170, 313–321 (2015).
Pellicori, P. et al. Impact of vasodilators on diuretic response in patients with congestive heart failure: a mechanistic trial of cimlanod (BMS-986231). Eur. J. Heart Fail. 26, 142–151 (2024).
Testani, J. M., Coca, S. G., McCauley, B. D., Shannon, R. P. & Kimmel, S. E. Impact of changes in blood pressure during the treatment of acute decompensated heart failure on renal and clinical outcomes. Eur. J. Heart Fail. 13, 877–884 (2011).
Voors, A. A. et al. Early drop in systolic blood pressure and worsening renal function in acute heart failure: renal results of Pre-RELAX-AHF. Eur. J. Heart Fail. 13, 961–967 (2011).
Dupont, M. et al. Determinants of dynamic changes in serum creatinine in acute decompensated heart failure: the importance of blood pressure reduction during treatment. Eur. J. Heart Fail. 15, 433–440 (2013).
Kula, A. J. et al. Influence of titration of neurohormonal antagonists and blood pressure reduction on renal function and decongestion in decompensated heart failure. Circ. Heart Fail. 9, e002333 (2016).
Testani, J. M. & Damman, K. Venous congestion and renal function in heart failure … it’s complicated. Eur. J. Heart Fail. 15, 599–601 (2013).
Firth, J. D., Raine, A. E. & Ledingham, J. G. Raised venous pressure: a direct cause of renal sodium retention in oedema? Lancet 1, 1033–1035 (1988).
Boorsma, E. M., Ter Maaten, J. M., Voors, A. A. & van Veldhuisen, D. J. Renal compression in heart failure: the renal tamponade hypothesis. JACC Heart Fail. 10, 175–183 (2022).
Dilley, J. R., Corradi, A. & Arendshorst, W. J. Glomerular ultrafiltration dynamics during increased renal venous pressure. Am. J. Physiol. 244, F650–F658 (1983).
Nohria, A. et al. Cardiorenal interactions: insights from the ESCAPE trial. J. Am. Coll. Cardiol. 51, 1268–1274 (2008).
Abraham, W. T. et al. Direct interstitial decongestion in an animal model of acute-on-chronic ischemic heart failure. JACC Basic Transl. Sci. 6, 872–881 (2021).
Itkin, M., Rockson, S. G. & Burkhoff, D. Pathophysiology of the lymphatic system in patients with heart failure: JACC state-of-the-art review. J. Am. Coll. Cardiol. 78, 278–290 (2021).
Costanzo, M. R. Ultrafiltration in acute heart failure. Card. Fail. Rev. 5, 9–18 (2019).
Costanzo, M. R. et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J. Am. Coll. Cardiol. 49, 675–683 (2007).
Costanzo, M. R. et al. Extracorporeal ultrafiltration for fluid overload in heart failure: current status and prospects for further research. J. Am. Coll. Cardiol. 69, 2428–2445 (2017).
Costanzo, M. R. et al. Aquapheresis versus intravenous diuretics and hospitalizations for heart failure. JACC Heart Fail. 4, 95–105 (2016).
Ivey-Miranda, J. B. et al. Reprieve system for the treatment of patients with acute decompensated heart failure. J. Card. Fail. https://doi.org/10.1016/j.cardfail.2025.02.002 (2025).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06362668 (2025).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05174312 (2025).
Rao, V. S. et al. First-in-human experience with peritoneal direct sodium removal using a zero-sodium solution: a new candidate therapy for volume overload. Circulation 141, 1043–1053 (2020).
Rao, V. S. et al. Serial direct sodium removal in patients with heart failure and diuretic resistance. Eur. J. Heart Fail. 26, 1215–1230 (2024).
Panagides, V. et al. Percutaneous lymphatic drainage through the thoracic duct: new paths in heart failure. CJC Open 5, 593–596 (2023).
Franksson, C., Lundgren, G., Magnusson, G. & Ringden, O. Drainage of thoracic duct lymph in renal transplant patients. Transplantation 21, 133–140 (1976).
Aronson, D. et al. Enhancing sweat rate using a novel device for the treatment of congestion in heart failure. Circ. Heart Fail. 16, e009787 (2023).
Miller, L., Cunningham, M., Richardson, A. & Burton, B. Wireless powered and water-proof mechanical circulatory support device for ambulatory class III heart failure. JACC Basic Transl. Sci. 7, 328–329 (2022).
Vanderheyden, M. et al. TRVD therapy in acute HF: proof of concept in animal model and initial clinical experience. J. Am. Coll. Cardiol. 77, 1481–1483 (2021).
Rao, V. S. et al. Renal negative pressure treatment as a novel therapy for heart failure-induced renal dysfunction. Am. J. Physiol. Regul. Integr. Comp. Physiol. 321, R588–R594 (2021).
Georges, G., Fudim, M., Burkhoff, D., Leon, M. & Genereux, P. Patient selection and end point definitions for decongestion studies in acute decompensated heart failure: part 1. J. Soc. Cardiovasc. Angiogr. Interv. 2, 101060 (2023).
Rosenblum, H. et al. Conceptual considerations for device-based therapy in acute decompensated heart failure: DRI2P2S. Circ. Heart Fail. 13, e006731 (2020).
Bradley, S. M., Levy, W. C. & Veenstra, D. L. Cost-consequences of ultrafiltration for acute heart failure: a decision model analysis. Circ. Cardiovasc. Qual. Outcomes 2, 566–573 (2009).
Pham, T. D. et al. Aldosterone regulates pendrin and epithelial sodium channel activity through intercalated cell mineralocorticoid receptor-dependent and -independent mechanisms over a wide range in serum potassium. J. Am. Soc. Nephrol. 31, 483–499 (2020).
Nielsen, J. et al. Sodium transporter abundance profiling in kidney: effect of spironolactone. Am. J. Physiol. Ren. Physiol. 283, F923–F933 (2002).
Leviel, F. et al. The Na+-dependent chloride-bicarbonate exchanger SLC4A8 mediates an electroneutral Na+ reabsorption process in the renal cortical collecting ducts of mice. J. Clin. Invest. 120, 1627–1635 (2010).
Author information
Authors and Affiliations
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
Z.L.C. reports grants from AstraZeneca and personal fees from Abiomed, Kestra Medical Technologies, Lexicon Pharmaceuticals, Reprieve Cardiovascular and Vectorious. K.D. reports speaker and consultancy fees to his employer from Abbott, AstraZeneca, Boehringer Ingelheim, Echosense, FIRE1 and Novartis. J.M.T. reports grants and/or personal fees from 3ive Labs, Abbott, AstraZeneca, Bayer, BD, Bristol Myers Squibb, Cardionomic, Corteria, Edwards Lifesciences, FIRE1, Lexicon Pharmaceuticals, Lilly, MagentaMed, Merck, Novartis, Otsuka, Precardia, Regeneron, Relypsa, Reprieve, Sanofi, Sequana Medical, Windtree Therapeutics and W.L. Gore. J.M.T. has a patent relating to the treatment of diuretic resistance issued to Yale University and Corvidia Therapeutics, a patent relating to methods for measuring renalase issued to Yale University, and a patent relating to the treatment of diuretic resistance pending with Reprieve.
Peer review
Peer review information
Nature Reviews Cardiology thanks Maria Rosa Constanzo, Steven Goldsmith and Frederik Verbrugge for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cox, Z.L., Damman, K. & Testani, J.M. Decongestion in heart failure: medical and device therapies. Nat Rev Cardiol 22, 961–977 (2025). https://doi.org/10.1038/s41569-025-01152-z
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-025-01152-z