Abstract
The aim of cancer screening is to identify pre-malignant conditions, which can be removed or treated, or earlier-stage disease, for which treatment is more likely to be curative, in non-symptomatic individuals. Currently, screening programmes are being consolidated for five cancer types (breast, prostate, cervical, colorectal and lung) and several other cancer types are the focus of specific initiatives. Cancer screening is at a point of potential major transformation owing to technological advances in detection. In this Review, we first recapitulate the general principles of cancer screening. We then provide a timely overview of the current screening practices for breast, cervical, colorectal, prostate and lung cancer, addressing major challenges and potential future changes in practice. We also discuss other malignancies for which screening initiatives might be worth considering. Finally, we highlight technological developments in cancer detection that might hold promise for screening an increasing number of cancers in the future, notably some that reflect unmet needs.
Key points
-
The main aims of cancer screening are to identify precursor states that can be removed or treated, or to detect disease at an early stage when treatment is more likely to be curative.
-
The screening intervention must reduce mortality and/or morbidity from the malignancy targeted.
-
Population screening programmes for breast, prostate, cervical, colorectal and lung cancer are widely implemented worldwide owing to their demonstrated benefits in incidence and/or mortality.
-
For a number of cancers, the evidence is not sufficiently compelling for population screening programmes to be set up; these include some cancers characterized by poor prognosis, such as oesophageal cancer.
-
Cancer screening might undergo major changes in the near future, notably with the advent of artificial intelligence tools for early detection and multicancer early detection tests. The latter are showing some promise for the early detection of some cancers that currently have a poor prognosis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Wald, N. J. Guidance on terminology. J. Med. Screen. 1, 76–76 (1994).
Smith, R. A. et al. Cancer screening in the United States, 2019: a review of current american cancer society guidelines and current issues in cancer screening. CA Cancer J. Clin. 69, 184–210 (2019).
Sasieni, P. et al. Modelled mortality benefits of multi-cancer early detection screening in England. Br. J. Cancer 129, 72–80 (2023).
Smith, R. A. & Oeffinger, K. C. The importance of cancer screening. Med. Clin. 104, 919–938 (2020).
Jansen, E. E. L. et al. Effect of organised cervical cancer screening on cervical cancer mortality in Europe: a systematic review. Eur. J. Cancer 127, 207–223 (2020).
Duffy, S. W. et al. The relative contributions of screen-detected in situ and invasive breast carcinomas in reducing mortality from the disease. Eur. J. Cancer 39, 1755–1760 (2003).
Wilson J. M. G. & Gunner, J. Principles and Practice of Screening for Disease (WHO, 1968).
Abdominal aortic aneurysm (AAA) screening. NHS https://www.nhs.uk/conditions/abdominal-aortic-aneurysm-screening/ (accessed 14 February 2024).
Andermann, A., Blancquaert, I., Beauchamp, S. & Déry, V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull. World Health Organ. 86, 317–319 (2008).
Massat, N. J., Moss, S. M., Halloran, S. P. & Duffy, S. W. Screening and primary prevention of colorectal cancer: a review of sex-specific and site-specific differences. J. Med. Screen. 20, 125–148 (2013).
Campbell, C. et al. Are there ethnic and religious variations in uptake of bowel cancer screening? A retrospective cohort study among 1.7 million people in Scotland. BMJ Open 10, e037011 (2020).
Jack, R. H., Møller, H., Robson, T. & Davies, E. A. Breast cancer screening uptake among women from different ethnic groups in London: a population-based cohort study. BMJ Open 4, e005586 (2014).
Moser, K., Patnick, J. & Beral, V. Inequalities in reported use of breast and cervical screening in Great Britain: analysis of cross sectional survey data. Br. Med. J. 338, b2025 (2009).
Webb, R., Richardson, J., Esmail, A. & Pickles, A. Uptake for cervical screening by ethnicity and place-of-birth: a population-based cross-sectional study. J. Public Health 26, 293–296 (2004).
Aliu, A. E., Kerrison, R. S. & Marcu, A. A systematic review of barriers to breast cancer screening, and of interventions designed to increase participation, among women of Black African and Black caribbean descent in the UK. Psychooncology 34, e70093 (2025).
Marlow, L. A. V., Waller, J. & Wardle, J. Barriers to cervical cancer screening among ethnic minority women: a qualitative study. J. Fam. Plan. Reprod. Health Care 41, 248–254 (2015).
BreastScreen Norway. Norwegian Institute of Public Health https://www.fhi.no/en/cancer/screening/breastscreen/ (accessed 21 October 2025).
Moshina, N. et al. Breast compression and reported pain during mammographic screening. Radiography 26, 133–139 (2020).
Breast screening programme, England, 2022–2023. NHS Digital https://digital.nhs.uk/data-and-information/publications/statistical/breast-screening-programme/england---2022-23 (accessed 27 August 2024).
Marmot, M. G. et al. The benefits and harms of breast cancer screening: an independent review: a report jointly commissioned by cancer research UK and the department of Health (England) October 2012. Br. J. Cancer 108, 2205–2240 (2013).
Duffy, S. W. et al. Long-term benefits of breast screening. Breast Cancer Manag. 1, 31–38 (2012).
Yaffe, M. J., Seely, J. M., Gordon, P. B., Appavoo, S. & Kopans, D. B. The randomized trial of mammography screening that was not — a cautionary tale. J. Med. Screen. 29, 7–11 (2022).
Seely, J. Failed randomization and explanation for the outlier results of the Canadian Breast Cancer Screening Studies. Borealis https://doi.org/10.5683/SP3/2DEY36 (2021).
Maroni, R. et al. A case-control study to evaluate the impact of the breast screening programme on mortality in England. Br. J. Cancer 124, 736–743 (2021).
Kopans, D. B., Biggs, K. W., Pyatt, R. S., Smetherman, D. & Friedberg, E. B. The state of breast cancer screening guidelines: a question and answer summary. J. Am. Coll. Radiol. 17, 629–632 (2020).
Screening for Breast Cancer: Breast Cancer Screening Draft Recommendation Consumer Guide (US Preventive Services Task Force, 2023).
Schünemann, H. J. et al. Breast cancer screening and diagnosis: a synopsis of the European breast guidelines. Ann. Intern. Med. 172, 46–56 (2020).
Giordano, L. et al. Mammographic screening programmes in Europe: organization, coverage and participation. J. Med. Screen. 19, 72–82 (2012).
Lauby-Secretan, B. et al. Breast-cancer screening — viewpoint of the IARC working group. N. Engl. J. Med. 372, 2353–2358 (2015).
Chaltiel, D. & Hill, C. Estimations of overdiagnosis in breast cancer screening vary between 0% and over 50%: why? BMJ Open 11, e046353 (2021).
Blyuss, O. et al. A case–control study to evaluate the impact of the breast screening programme on breast cancer incidence in England. Cancer Med. 12, 1878–1887 (2023).
Njor, S. H. et al. Overdiagnosis in screening mammography in Denmark: population based cohort study. Br. Med. J. 346, f1064 (2013).
Potnis, K. C., Ross, J. S., Aneja, S., Gross, C. P. & Richman, I. B. Artificial intelligence in breast cancer screening: evaluation of FDA device regulation and future recommendations. JAMA Intern. Med. 182, 1306–1312 (2022).
Hill, H. et al. The cost-effectiveness of risk-stratified breast cancer screening in the UK. Br. J. Cancer 129, 1801–1809 (2023).
Hernström, V. et al. Screening performance and characteristics of breast cancer detected in the mammography screening with artificial intelligence trial (MASAI): a randomised, controlled, parallel-group, non-inferiority, single-blinded, screening accuracy study. Lancet Digit. Health 7, e175–e183 (2025).
Sechopoulos, I., Teuwen, J. & Mann, R. Artificial intelligence for breast cancer detection in mammography and digital breast tomosynthesis: state of the art. Semin. Cancer Biol. 72, 214–225 (2021).
Duffy, S. W., de Jonge, L. & Duffy, T. E. Effects on cancer prevention from the COVID-19 pandemic. Annu. Rev. Med. 75, 1–11 (2024).
Dembrower, K., Crippa, A., Colón, E., Eklund, M. & Strand, F. Artificial intelligence for breast cancer detection in screening mammography in Sweden: a prospective, population-based, paired-reader, non-inferiority study. Lancet Digit. Health 5, e703–e711 (2023).
Dembrower, K. E., Crippa, A., Eklund, M. & Strand, F. Human–AI interaction in the screentrustCAD trial: recall proportion and positive predictive value related to screening mammograms flagged by AI CAD versus a human reader. Radiology 314, e242566 (2025).
Lauritzen, A. D. et al. Early indicators of the impact of using AI in mammography screening for breast cancer. Radiology 311, e232479 (2024).
World-leading AI trial to tackle breast cancer launched. National Institute for Health and Care Excellence https://www.nihr.ac.uk/news/world-leading-ai-trial-tackle-breast-cancer-launched (accessed 12 February 2025).
Bennett, R. L., Sellars, S. J. & Moss, S. M. Interval cancers in the NHS breast cancer screening programme in England, Wales and Northern Ireland. Br. J. Cancer 104, 571–577 (2011).
Bevan, R. & Rutter, M. D. Colorectal cancer screening-who, how, and when. Clin. Endosc. 51, 37–49 (2018).
Primm, K. M., Malabay, A. J., Curry, T. & Chang, S. Who, where, when: colorectal cancer disparities by race and ethnicity, subsite, and stage. Cancer Med. 12, 14767–14780 (2023).
Chung, S. W., Hakim, S., Siddiqui, S. & Cash, B. D. Update on flexible sigmoidoscopy, computed tomographic colonography, and capsule colonoscopy. Gastrointest. Endosc. Clin. 30, 569–583 (2020).
Ansa, B. E. et al. Evaluation of colonoscopy and sigmoidoscopy utilization for colorectal cancer screening in Georgia, USA. Curr. Oncol. 29, 8955–8966 (2022).
Davis, M. M. et al. Geographic and population-level disparities in colorectal cancer testing: a multilevel analysis of Medicaid and commercial claims data. Prev. Med. 101, 44–52 (2017).
Schreuders, E. H. et al. Colorectal cancer screening: a global overview of existing programmes. Gut 64, 1637–1649 (2015).
Senore, C. et al. Performance of colorectal cancer screening in the European Union member states: data from the second European screening report. Gut 68, 1232–1244 (2019).
Ola, I., Cardoso, R., Hoffmeister, M. & Brenner, H. Utilization of colorectal cancer screening tests: a systematic review and time trend analysis of nationally representative data. EClinicalMedicine 75, 102783 (2024).
Wooldrage, K., Robbins, E. C., Duffy, S. W. & Cross, A. J. Long-term effects of once-only flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: 21-year follow-up of the UK Flexible Sigmoidoscopy Screening randomised controlled trial. Lancet Gastroenterol. Hepatol. 9, 811–824 (2024).
Holme, Ø et al. Effectiveness of flexible sigmoidoscopy screening in men and women and different age groups: pooled analysis of randomised trials. Br. Med. J. 356, i6673 (2017).
Pinsky, P. F. et al. Number of adenomas removed and colorectal cancers prevented in randomized trials of flexible sigmoidoscopy screening. Gastroenterology 155, 1059–1068 (2018).
Moss, S. et al. Increased uptake and improved outcomes of bowel cancer screening with a faecal immunochemical test: results from a pilot study within the national screening programme in England. Gut 66, 1631–1644 (2017).
Breekveldt, E. C. H. et al. Colorectal cancer incidence, mortality, tumour characteristics, and treatment before and after introduction of the faecal immunochemical testing-based screening programme in the Netherlands: a population-based study. Lancet Gastroenterol. Hepatol. 7, 60–68 (2022).
Imperiale, T. F. et al. Next-generation multitarget stool DNA test for colorectal cancer screening. N. Engl. J. Med. 390, 984–993 (2024).
Imperiale, T. F. et al. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 370, 1287–1297 (2014).
Wisse, P. H. A. et al. The multitarget faecal immunochemical test for improving stool-based colorectal cancer screening programmes: a Dutch population-based, paired-design, intervention study. Lancet Oncol. 25, 326–337 (2024).
de Klaver, W. et al. Clinical validation of a multitarget fecal immunochemical test for colorectal cancer screening : a diagnostic test accuracy study. Ann. Intern. Med. 174, 1224–1231 (2021).
Clark, G. R. C. et al. Interval cancers in a national colorectal screening programme based on faecal immunochemical testing: implications for faecal haemoglobin concentration threshold and sex inequality. J. Med. Screen. 31, 21–27 (2024).
Li, S. J. et al. Impact of changes to the interscreening interval and faecal immunochemical test threshold in the national bowel cancer screening programme in England: results from the FIT pilot study. Br. J. Cancer 127, 1525–1533 (2022).
Li, S. J. et al. Faecal immunochemical testing in bowel cancer screening: estimating outcomes for different diagnostic policies. J. Med. Screen. 28, 277–285 (2021).
Singer, A. 2 Cervical cancer screening: state of the art. Baillière’s Clin. Obstet. Gynaecol. 9, 39–64 (1995).
Basu, P., Nessa, A., Majid, M., Rahman, J. N. & Ahmed, T. Evaluation of the national cervical cancer screening programme of Bangladesh and the formulation of quality assurance guidelines. BMJ Sex. Reprod. Health 36, 131–134 (2010).
Almonte, M. et al. Visual inspection after acetic acid (VIA) is highly heterogeneous in primary cervical screening in Amazonian Peru. PLoS ONE 10, e0115355 (2015).
Simms, K. T. et al. Benefits, harms and cost-effectiveness of cervical screening, triage and treatment strategies for women in the general population. Nat. Med. 29, 3050–3058 (2023).
Fontham, E. T. H. et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J. Clin. 70, 321–346 (2020).
Tainio, K. et al. Clinical course of untreated cervical intraepithelial neoplasia grade 2 under active surveillance: systematic review and meta-analysis. Br. Med. J. 360, k499 (2018).
Sigurdsson, K. The Icelandic and Nordic cervical screening programs, trends in incidence and mortality rates through 1995. Acta Obstet. Gynecol. Scand. 78, 478–485 (1999).
Kyrgiou, M. et al. Cervical screening: ESGO–EFC position paper of the european society of gynaecologic oncology (ESGO) and the European federation of colposcopy (EFC). Br. J. Cancer 123, 510–517 (2020).
Bruni, L. et al. Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: a review and synthetic analysis. Lancet Glob. Health 10, e1115–e1127 (2022).
Sasieni, P., Castanon, A. & Cuzick, J. Effectiveness of cervical screening with age: population based case-control study of prospectively recorded data. Br. Med. J. 339, b2968 (2009).
Drysdale, H., Marlow, L. A. V., Lim, A. & Waller, J. Experiences of self-sampling and future screening preferences in non-attenders who returned an HPV vaginal self-sample in the youscreen study: findings from a cross-sectional questionnaire. Health Expect. 27, e14118 (2024).
Lim, A. W. W. et al. Opportunistic offering of self-sampling to non-attenders within the English cervical screening programme: a pragmatic, multicentre, implementation feasibility trial with randomly allocated cluster intervention start dates (YouScreen). eClinicalMedicine 73, 102672 (2024).
Rebolj, M., Sargent, A., Njor, S. H. & Cuschieri, K. Widening the offer of human papillomavirus self-sampling to all women eligible for cervical screening: make haste slowly. Int. J. Cancer 153, 8–19 (2023).
Arbyn, M., Smith, S. B., Temin, S., Sultana, F. & Castle, P. Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. Br. Med. J. 363, k4823 (2018).
Falcaro, M. et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet 398, 2084–2092 (2021).
Douglas, E., Waller, J., Duffy, S. W. & Wardle, J. Socioeconomic inequalities in breast and cervical screening coverage in England: are we closing the gap? J. Med. Screen. 23, 98–103 (2016).
Bongaerts, T. H., Büchner, F. L., Middelkoop, B. J., Guicherit, O. R. & Numans, M. E. Determinants of (non-)attendance at the Dutch cancer screening programmes: a systematic review. J. Med. Screen. 27, 121–129 (2020).
Leinonen, M. K. et al. Personal and provider level factors influence participation to cervical cancer screening: a retrospective register-based study of 1.3 million women in Norway. Prev. Med. 94, 31–39 (2017).
Chorley, A. J., Marlow, L. A., Forster, A. S., Haddrell, J. B. & Waller, J. Experiences of cervical screening and barriers to participation in the context of an organised programme: a systematic review and thematic synthesis. Psychooncology 26, 161–172 (2017).
Wearn, A. & Shepherd, L. Determinants of routine cervical screening participation in underserved women: a qualitative systematic review. Psychol. Health 39, 145–170 (2024).
Falcaro, M., Soldan, K., Ndlela, B. & Sasieni, P. Effect of the HPV vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia by socioeconomic deprivation in England: population based observational study. Br. Med. J. 385, e077341 (2024).
Duffy, S. W. & Wald, N. J. When primary prevention replaces screening. J. Med. Screen. 29, 67–67 (2022).
Gilham, C. & Peto, J. Is elimination of cervical cancer in sight in England? Prev. Med. 191, 108218 (2025).
Human Papillomavirus (HPV) vaccination coverage. World Health Organization https://immunizationdata.who.int/global/wiise-detail-page/ (accessed 23 May 2025)
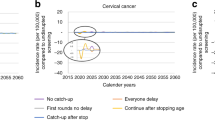
Castanon, A., Landy, R., Pesola, F., Windridge, P. & Sasieni, P. Prediction of cervical cancer incidence in England, UK, up to 2040, under four scenarios: a modelling study. Lancet Public Health 3, e34–e43 (2018).
Landy, R., Windridge, P., Gillman, M. S. & Sasieni, P. D. What cervical screening is appropriate for women who have been vaccinated against high risk HPV? A simulation study. Int. J. Cancer 142, 709–718 (2018).
Fenton, J. J. et al. Prostate-specific antigen–based screening for prostate cancer: evidence report and systematic review for the US Preventive Services Task Force. JAMA 319, 1914–1931 (2018).
Prostate cancer: diagnosis and management — NICE guideline NG131. National Institute for Health and Care Excellence https://www.nice.org.uk/guidance/ng131/chapter/recommendations#assessment-and-diagnosis (accessed 11 June 2025).
Heidegger, I. et al. Age-adjusted PSA levels in prostate cancer prediction: updated results of the tyrol prostate cancer early detection program. PLoS ONE 10, e0134134 (2015).
Hugosson, J. et al. A 16-yr follow-up of the european randomized study of screening for prostate cancer. Eur. Urol. 76, 43–51 (2019).
Shoag, J. E., Nyame, Y. A., Gulati, R., Etzioni, R. & Hu, J. C. Reconsidering the trade-offs of prostate cancer screening. N. Engl. J. Med. 382, 2465–2468 (2020).
Leenen, R. C. A. et al. Prostate cancer early detection in the European Union and UK. Eur. Urol. 87, 326–339 (2024).
Beyer, K. et al. Health policy for prostate cancer early detection in the european union and the impact of opportunistic screening: PRAISE-U consortium. J. Pers. Med. 14, 84 (2024).
Gómez Rivas, J. et al. Navigating through the controversies and emerging paradigms in early detection of prostate cancer: bridging the gap from classic RCTs to modern population-based pilot programs. J. Pers. Med. 13, 1677 (2023).
Prostate cancer statistics. Cancer Research UK https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer (accessed 08 August 2024).
Lodder, J. J. et al. A personalized, risk-based approach to active surveillance for prostate cancer with takeaways from broader oncology practices: a mixed methods review. J. Pers. Med. 15, 84 (2025).
Tosoian, J. J., Penson, D. F. & Chinnaiyan, A. M. A pragmatic approach to prostate cancer screening. JAMA 331, 1448–1450 (2024).
Ahmed, H. U. et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389, 815–822 (2017).
Kasivisvanathan, V. et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N. Engl. J. Med. 378, 1767–1777 (2018).
Ibraheem, N. et al. Innovations and emerging trends in prostate cancer management: a literature review. Cureus 16, e73128 (2024).
Bach, P. B., Kelley, M. J., Tate, R. C. & McCrory, D. C. Screening for lung cancer: a review of the current literature. Chest 123, 72S–82S (2003).
Henschke, C. I. et al. Early lung cancer action project: initial findings on repeat screenings. Cancer 92, 153–159 (2001).
Aberle, D. R. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 365, 395–409 (2011).
de Koning, H. J. et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N. Engl. J. Med. 382, 503–513 (2020).
Field, J. K. et al. Lung cancer mortality reduction by LDCT screening: UKLS randomised trial results and international meta-analysis. Lancet Reg. Health Eur. 10, 100179 (2021).
Leiter, A., Veluswamy, R. R. & Wisnivesky, J. P. The global burden of lung cancer: current status and future trends. Nat. Rev. Clin. Oncol. 20, 624–639 (2023).
US Preventive Services Task Force. Screening for lung cancer: US preventive services task force recommendation statement. JAMA 325, 962–970 (2021).
Adult screening programme — lung cancer. UK National Screening Committee https://view-health-screening-recommendations.service.gov.uk/lung-cancer/ (accessed 13 February 2025).
Lam, S. et al. Current and future perspectives on computed tomography screening for lung cancer: a roadmap from 2023 to 2027 from the International Association for the Study of Lung Cancer. J. Thorac. Oncol. 19, 36–51 (2024).
Zhong, D. et al. Lung nodule management in low-dose CT screening for lung cancer: lessons from the NELSON trial. Radiology 313, e240535 (2024).
Callister, M. E. J. et al. British Thoracic Society guidelines for the investigation and management of pulmonary nodules: accredited by NICE. Thorax 70, ii1–ii54 (2015).
Lung-RADS — lung CT screening, reporting and data system. American College of Radiology https://www.acr.org/Clinical-Resources/Clinical-Tools-and-Reference/Reporting-and-Data-Systems/Lung-RADS (accessed 31 October 2025).
Pinsky, P. F. Assessing the benefits and harms of low-dose computed tomography screening for lung cancer. Lung Cancer Manag. 3, 491–498 (2014).
Lancaster, H. L. et al. Histological proven AI performance in the UKLS CT lung cancer screening study: potential for workload reduction. Eur. J. Cancer 220, 115324 (2025).
Geppert, J. et al. Software using artificial intelligence for nodule and cancer detection in CT lung cancer screening: systematic review of test accuracy studies. Thorax 79, 1040–1049 (2024).
Afridi, W. A. et al. Minimally invasive biomarkers for triaging lung nodules-challenges and future perspectives. Cancer Metastasis Rev. 44, 29 (2025).
Harrison, N. J. et al. ‘Every touch point is an opportunity’: tobacco control experts’ views on how to implement smoking cessation interventions within an Australian lung cancer screening program. Cancer Med. 14, e70963 (2025).
de Nijs, K., Ten Haaf, K., van der Aalst, C. & de Koning, H. J. Projected effectiveness of lung cancer screening and concurrent smoking cessation support in the Netherlands. EClinicalMedicine 71, 102570 (2024).
Oesophageal cancer statistics. Cancer Research UK https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/oesophageal-cancer#heading-Two (accessed 12 February 2025).
Puhr, H. C. et al. Viennese risk prediction score for advanced gastroesophageal carcinoma based on alarm symptoms (VAGAS score): characterisation of alarm symptoms in advanced gastro-oesophageal cancer and its correlation with outcome. ESMO Open 5, e000623 (2020).
Hamade, N. et al. Significant decline in the prevalence of Barrett’s esophagus among patients with gastroesophageal reflux disease. Dis. Esophagus 34, doaa131 (2021).
Westhoff, B. et al. The frequency of Barrett’s esophagus in high-risk patients with chronic GERD. Gastrointest. Endosc. 61, 226–231 (2005).
Ronkainen, J. et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology 129, 1825–1831 (2005).
Hvid-Jensen, F., Pedersen, L., Drewes, A. M., Sorensen, H. T. & Funch-Jensen, P. Incidence of adenocarcinoma among patients with Barrett’s esophagus. N. Engl. J. Med. 365, 1375–1383 (2011).
Januszewicz, W. & Fitzgerald, R. C. Early detection and therapeutics. Mol. Oncol. 13, 599–613 (2019).
Offman, J. et al. Barrett’s oESophagus trial 3 (BEST3): study protocol for a randomised controlled trial comparing the Cytosponge-TFF3 test with usual care to facilitate the diagnosis of oesophageal pre-cancer in primary care patients with chronic acid reflux. BMC Cancer 18, 784 (2018).
Fitzgerald, R. C. et al. Cytosponge-trefoil factor 3 versus usual care to identify Barrett’s oesophagus in a primary care setting: a multicentre, pragmatic, randomised controlled trial. Lancet 396, 333–344 (2020).
BEST4 trial. University of Cambridge Early Cancer Institute https://www.earlycancer.cam.ac.uk/our-research/our-clinical-studies/best-4-trial (accessed 21 November 2024).
Moon, S., Song, Y. S., Jung, K. Y., Lee, E. K. & Park, Y. J. Lower thyroid cancer mortality in patients detected by screening: a meta-analysis. Endocrinol. Metab. 38, 93–103 (2023).
Lee, Y. K. et al. Changes in the diagnostic efficiency of thyroid fine-needle aspiration biopsy during the era of increased thyroid cancer screening in Korea. Cancer Res. Treat. 51, 1430–1436 (2019).
Toyoda, Y. et al. Increase in incidental detection of thyroid cancer in Osaka, Japan. Cancer Sci. 109, 2310–2314 (2018).
Li, M. et al. Mapping overdiagnosis of thyroid cancer in China. Lancet Diabetes Endocrinol. 9, 330–332 (2021).
Park, S. et al. Association between screening and the thyroid cancer “epidemic” in South Korea: evidence from a nationwide study. Br. Med. J. 355, i5745 (2016).
Bibbins-Domingo, K. et al. Screening for thyroid cancer: US Preventive Services Task Force recommendation statement. JAMA 317, 1882–1887 (2017).
Operational framework management of common cancers. Ministry of Health and Family Welfare–Government of India https://nhsrcindia.org/sites/default/files/2021-03/Operational%20Framework%20Management%20of%20Common%20Cancers.pdf (accessed 30 June 2025).
Sankaranarayanan, R. et al. Effect of screening on oral cancer mortality in Kerala, India: a cluster-randomised controlled trial. Lancet 365, 1927–1933 (2005).
Rumgay, H. et al. Global burden of oral cancer in 2022 attributable to smokeless tobacco and areca nut consumption: a population attributable fraction analysis. Lancet Oncol. 25, 1413–1423 (2024).
Parak, U., Carvalho, A. L., Roitberg, F. & Mandrik, O. Effectiveness of screening for oral cancer and oral potentially malignant disorders (OPMD): a systematic review. Prev. Med. Rep. 30, 101987 (2022).
Mayerhoefer, M. E., Kienzle, A., Woo, S. & Vargas, H. A. Update on liquid biopsy. Radiology 315, e241030 (2025).
Nielsen, S. & Narayan, A. K. Breast cancer screening modalities, recommendations, and novel imaging techniques. Surg. Clin. North. Am. 103, 63–82 (2023).
Taylor, L. C. et al. Acceptability of risk stratification within population-based cancer screening from the perspective of the general public: a mixed-methods systematic review. Health Expect. 26, 989–1008 (2023).
Parums, D. V. Artificial intelligence (AI), digital image analysis, and the future of cancer diagnosis and prognosis. Med. Sci. Monit. 30, e947038 (2024).
Guerra, C. E., Sharma, P. V. & Castillo, B. S. Multi-cancer early detection: the new frontier in cancer early detection. Annu. Rev. Med. 75, 67–81 (2024).
Sasieni, P., Swanton, C. & Neal, R. D. The National Health Service—Galleri multi-cancer screening trial: explanation and justification of unique and important design issues. J. Natl Cancer Inst. https://doi.org/10.1093/jnci/djaf218 (2025).
Klein, E. A. et al. Clinical validation of a targeted methylation-based multi-cancer early detection test using an independent validation set. Ann. Oncol. 32, 1167–1177 (2021).
Wan, J. C. M., Sasieni, P. & Rosenfeld, N. Promises and pitfalls of multi-cancer early detection using liquid biopsy tests. Nat. Rev. Clin. Oncol. 22, 566–580 (2025).
Shapiro, S. Periodic screening for breast cancer: the HIP randomized controlled trial. JNCI Monogr. 1997, 27–30 (1997).
Duffy, S. W. et al. The Swedish two-county trial of mammographic screening: cluster randomisation and end point evaluation. Ann. Oncol. 14, 1196–1198 (2003).
Andersson, I. et al. Mammographic screening and mortality from breast cancer: the Malmö mammographic screening trial. Br. Med. J. 297, 943–948 (1988).
Andersson, I. & Janzon, L. Reduced breast cancer mortality in women under age 50: updated results from the Malmö mammographic screening program. JNCI Monogr. 1997, 63–67 (1997).
Frisell, J. & Lidbrink, E. The Stockholm mammographic screening trial: risks and benefits in age group 40-49 Years. JNCI Monogr. 1997, 49–51 (1997).
Bjurstam, N. et al. The Gothenburg breast screening trial. Cancer 97, 2387–2396 (2003).
Duffy, S. W. et al. Effect of mammographic screening from age 40 years on breast cancer mortality (UK Age trial): final results of a randomised, controlled trial. Lancet Oncol. 21, 1165–1172 (2020).
Acknowledgements
J.O. receives support from the Barts Charity (grant G-001522/MGU0461).
Author information
Authors and Affiliations
Contributions
S.W.D. researched data for the article. J.O. and S.W.D. wrote, reviewed and/or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
S.W.D has occasionally been a consultant for Grail and Roche, both on methodological aspects. J.O. has occasionally been a consultant for Hardian Health.
Peer review
Peer review information
Nature Reviews Clinical Oncology thanks P. Basu and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Duffy, S.W., Offman, J. A guide to cancer screening. Nat Rev Clin Oncol (2026). https://doi.org/10.1038/s41571-025-01112-z
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41571-025-01112-z