Abstract
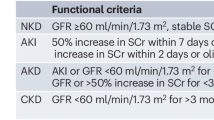
Acute kidney injury (AKI) is defined by a sudden loss of excretory kidney function. AKI is part of a range of conditions summarized as acute kidney diseases and disorders (AKD), in which slow deterioration of kidney function or persistent kidney dysfunction is associated with an irreversible loss of kidney cells and nephrons, which can lead to chronic kidney disease (CKD). New biomarkers to identify injury before function loss await clinical implementation. AKI and AKD are a global concern. In low-income and middle-income countries, infections and hypovolaemic shock are the predominant causes of AKI. In high-income countries, AKI mostly occurs in elderly patients who are in hospital, and is related to sepsis, drugs or invasive procedures. Infection and trauma-related AKI and AKD are frequent in all regions. The large spectrum of AKI implies diverse pathophysiological mechanisms. AKI management in critical care settings is challenging, including appropriate volume control, nephrotoxic drug management, and the timing and type of kidney support. Fluid and electrolyte management are essential. As AKI can be lethal, kidney replacement therapy is frequently required. AKI has a poor prognosis in critically ill patients. Long-term consequences of AKI and AKD include CKD and cardiovascular morbidity. Thus, prevention and early detection of AKI are essential.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
KDIGO AKI Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138 (2012).
Bhatraju, P. K. et al. Association between early recovery of kidney function after acute kidney injury and long-term clinical outcomes. JAMA Netw. Open 3, e202682 (2020).
Chu, R. et al. Assessment of KDIGO definitions in patients with histopathologic evidence of acute renal disease. Clin. J. Am. Soc. Nephrol. 9, 1175–1182 (2014).
Kane-Gill, S. L., Meersch, M. & Bell, M. Biomarker-guided management of acute kidney injury. Curr. Opin. Crit. Care 26, 556–562 (2020).
Ostermann, M. et al. Recommendations on acute kidney injury biomarkers from the acute disease quality initiative consensus conference: a consensus statement. JAMA Netw. Open 3, e2019209 (2020).
Bhagwanani, A., Carpenter, R. & Yusuf, A. Improving the management of acute kidney injury in a district general hospital: introduction of the DONUT bundle. BMJ Qual. Improv. Rep. 2, u202650.w1235 (2014).
Biswas, A. et al. Identification of patients expected to benefit from electronic alerts for acute kidney injury. Clin. J. Am. Soc. Nephrol. 13, 842–849 (2018).
Joslin, J. et al. Recognition and management of acute kidney injury in hospitalised patients can be partially improved with the use of a care bundle. Clin. Med. 15, 431–436 (2015).
Lachance, P. et al. Association between e-alert implementation for detection of acute kidney injury and outcomes: a systematic review. Nephrol. Dial. Transplant. 32, 265–272 (2017).
Wołyniec, W. et al. Glomerular filtration rate is unchanged by ultramarathon. J. Strength Cond. Res. 32, 3207–3215 (2018).
MacDonald, A. J., Nadim, M. K., Durand, F. & Karvellas, C. J. Acute kidney injury in cirrhosis: implications for liver transplantation. Curr. Opin. Crit. Care 25, 171–178 (2019).
Fenoglio, R., Sciascia, S., Baldovino, S. & Roccatello, D. Acute kidney injury associated with glomerular diseases. Curr. Opin. Crit. Care 25, 573–579 (2019).
Mannon, R. B. Delayed graft function: the AKI of kidney transplantation. Nephron 140, 94–98 (2018).
Selewski, D. T. et al. Neonatal acute kidney injury. Pediatrics 136, e463–e473 (2015).
Lewington, A. J., Cerdá, J. & Mehta, R. L. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 84, 457–467 (2013).
Cerdá, J., Bagga, A., Kher, V. & Chakravarthi, R. M. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat. Clin. Pract. Nephrol. 4, 138–153 (2008).
Luyckx, V. A., Tonelli, M. & Stanifer, J. W. The global burden of kidney disease and the sustainable development goals. Bull. World Health Organ. 96, 414–422 (2018).
Jha, V. & Parameswaran, S. Community-acquired acute kidney injury in tropical countries. Nat. Rev. Nephrol. 9, 278–290 (2013).
Olowu, W. A. et al. Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob. Health 4, e242–e250 (2016).
Susantitaphong, P. et al. World incidence of AKI: a meta-analysis. Clin. J. Am. Soc. Nephrol. 8, 1482–1493 (2013).
Martin-Cleary, C., Molinero-Casares, L. M., Ortiz, A. & Arce-Obieta, J. M. Development and internal validation of a prediction model for hospital-acquired acute kidney injury. Clin. Kidney J. 14, 309–316 (2021).
Hoste, E. A. J. et al. Global epidemiology and outcomes of acute kidney injury. Nat. Rev. Nephrol. 14, 607–625 (2018).
Mehta, R. L. et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet 385, 2616–2643 (2015).
Mehta, R. L. et al. Recognition and management of acute kidney injury in the International Society of Nephrology 0by25 Global Snapshot: a multinational cross-sectional study. Lancet 387, 2017–2025 (2016).
Bairey Merz, C. N. et al. Sex and the kidneys: current understanding and research opportunities. Nat. Rev. Nephrol. 15, 776–783 (2019).
Chew, S. T., Mar, W. M. & Ti, L. K. Association of ethnicity and acute kidney injury after cardiac surgery in a South East Asian population. Br. J. Anaesth. 110, 397–401 (2013).
Beers, K. et al. Racial and ethnic disparities in pregnancy-related acute kidney injury. Kidney 360 1, 169–178 (2020).
Grams, M. E. et al. Explaining the racial difference in AKI incidence. J. Am. Soc. Nephrol. 25, 1834–1841 (2014).
Cerdá, J. et al. Epidemiology of acute kidney injury. Clin. J. Am. Soc. Nephrol. 3, 881–886 (2008).
Lameire, N., Van Biesen, W. & Vanholder, R. The changing epidemiology of acute renal failure. Nat. Clin. Pract. Nephrol. 2, 364–377 (2006).
Lameire, N. H. et al. Acute kidney injury: an increasing global concern. Lancet 382, 170–179 (2013).
Kaul, A., Bhadauria, D., Prasad, N., Gupta, A. & Sharma, R. K. Recurrent acute kidney injury in tropics — epidemiology and outcomes. J. Assoc. Physicians India 66, 18–21 (2018).
Uchino, S. et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294, 813–818 (2005).
Denic, A. et al. The substantial loss of nephrons in healthy human kidneys with aging. J. Am. Soc. Nephrol. 28, 313–320 (2017).
Denic, A. et al. Single-nephron glomerular filtration rate in healthy adults. N. Engl. J. Med. 376, 2349–2357 (2017).
Levey, A. S. et al. Nomenclature for kidney function and disease: report of a Kidney Disease: Improving Global Outcomes (KDIGO) consensus conference. Kidney Int. 97, 1117–1129 (2020).
Saran, R. et al. US Renal Data System 2019 annual data report: epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 75, A6–A7 (2020).
Romagnani, P. et al. Chronic kidney disease. Nat. Rev. Dis. Prim. 3, 17088 (2017).
Prowle, J. R., Kirwan, C. J. & Bellomo, R. Fluid management for the prevention and attenuation of acute kidney injury. Nat. Rev. Nephrol. 10, 37–47 (2014). Overview of fluid status assessment and analysis of cardiovascular and renal targets for the prevention and attenuation of AKI.
Weyker, P. D., Pérez, X. L. & Liu, K. D. Management of acute kidney injury and acid-base balance in the septic patient. Clin. Chest Med. 37, 277–288 (2016).
Lee, S. A., Cozzi, M., Bush, E. L. & Rabb, H. Distant organ dysfunction in acute kidney injury: a review. Am. J. Kidney Dis. 72, 846–856 (2018).
Meijers, B., Evenepoel, P. & Anders, H. J. Intestinal microbiome and fitness in kidney disease. Nat. Rev. Nephrol. 15, 531–545 (2019).
Li, X., Hassoun, H. T., Santora, R. & Rabb, H. Organ crosstalk: the role of the kidney. Curr. Opin. Crit. Care 15, 481–487 (2009).
Faubel, S. & Edelstein, C. L. Mechanisms and mediators of lung injury after acute kidney injury. Nat. Rev. Nephrol. 12, 48–60 (2016).
Nakazawa, D. et al. Histones and neutrophil extracellular traps enhance tubular necrosis and remote organ injury in Ischemic AKI. J. Am. Soc. Nephrol. 28, 1753–1768 (2017).
Di Lullo, L., Reeves, P. B., Bellasi, A. & Ronco, C. Cardiorenal syndrome in acute kidney injury. Semin. Nephrol. 39, 31–40 (2019).
Kovalcikova, A. et al. Oxidative stress in the brain caused by acute kidney injury. Metab. Brain Dis. 33, 961–967 (2018).
Sharfuddin, A. A. & Molitoris, B. A. Pathophysiology of ischemic acute kidney injury. Nat. Rev. Nephrol. 7, 189–200 (2011).
Ehrmann, S. et al. Nephrotoxic drug burden among 1001 critically ill patients: impact on acute kidney injury. Ann. Intensive Care 9, 106 (2019).
Goldstein, S. L. et al. Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics 132, e756–e767 (2013).
Costa e Silva, V. T., Marçal, L. J. & Burdmann, E. A. Risk factors for vancomycin nephrotoxicity: still a matter of debate*. Crit. Care Med. 42, 2635–2636 (2014).
Joyce, E. L., Kane-Gill, S. L., Priyanka, P., Fuhrman, D. Y. & Kellum, J. A. Piperacillin/tazobactam and antibiotic-associated acute kidney injury in critically Ill children. J. Am. Soc. Nephrol. 30, 2243–2251 (2019).
Fu, E. L. et al. Association of acute increases in plasma creatinine after renin-angiotensin blockade with subsequent outcomes. Clin. J. Am. Soc. Nephrol. 14, 1336–1345 (2019).
Weisberg, L. S., Allgren, R. L., Genter, F. C. & Kurnik, B. R. Cause of acute tubular necrosis affects its prognosis. The Auriculin Anaritide Acute Renal Failure Study Group. Arch. Intern. Med. 157, 1833–1838 (1997).
Santos, W. J. et al. Patients with ischaemic, mixed and nephrotoxic acute tubular necrosis in the intensive care unit—a homogeneous population? Crit. Care 10, R68 (2006).
Mulay, S. R. & Anders, H. J. Crystal nephropathies: mechanisms of crystal-induced kidney injury. Nat. Rev. Nephrol. 13, 226–240 (2017).
Kers, J., Leemans, J. C. & Linkermann, A. An overview of pathways of regulated necrosis in acute kidney injury. Semin. Nephrol. 36, 139–152 (2016).
Linkermann, A. et al. Synchronized renal tubular cell death involves ferroptosis. Proc. Natl Acad. Sci. USA 111, 16836–16841 (2014). Study demonstrating the occurrence of regulated necrosis and synchronized death of upon AKI, with consequent triggering of a detrimental immune response.
Arai, S. et al. Apoptosis inhibitor of macrophage protein enhances intraluminal debris clearance and ameliorates acute kidney injury in mice. Nat. Med. 22, 183–193 (2016).
Salei, N. et al. The kidney contains ontogenetically distinct dendritic cell and macrophage subtypes throughout development that differ in their inflammatory properties. J. Am. Soc. Nephrol. 31, 257–278 (2020).
Linkermann, A., Stockwell, B. R., Krautwald, S. & Anders, H. J. Regulated cell death and inflammation: an auto-amplification loop causes organ failure. Nat. Rev. Immunol. 14, 759–767 (2014).
Mulay, S. R., Linkermann, A. & Anders, H. J. Necroinflammation in kidney disease. J. Am. Soc. Nephrol. 27, 27–39 (2016).
Lazzeri, E. et al. Endocycle-related tubular cell hypertrophy and progenitor proliferation recover renal function after acute kidney injury. Nat. Commun. 9, 1344 (2018). Study describing the occurrence of cellular hypertrophy in the absence of tissue reconstitution and limited regeneration after AKI.
Rinkevich, Y. et al. In vivo clonal analysis reveals lineage-restricted progenitor characteristics in mammalian kidney development, maintenance, and regeneration. Cell Rep. 7, 1270–1283 (2014).
Kang, H. M. et al. Sox9-positive progenitor cells play a key role in renal tubule epithelial regeneration in mice. Cell Rep. 14, 861–871 (2016).
Chawla, L. S. et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat. Rev. Nephrol. 13, 241–257 (2017).
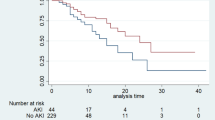
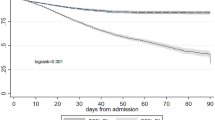
Kellum, J. A., Sileanu, F. E., Bihorac, A., Hoste, E. A. & Chawla, L. S. Recovery after acute kidney injury. Am. J. Respir. Crit. Care Med. 195, 784–791 (2017).
Lazzeri, E., Angelotti, M. L., Conte, C., Anders, H. J. & Romagnani, P. Surviving acute organ failure: cell polyploidization and progenitor proliferation. Trends Mol. Med. 25, 366–381 (2019).
Patel, S. S., Palant, C. E., Mahajan, V. & Chawla, L. S. Sequelae of AKI. Best. Pract. Res. Clin. Anaesthesiol. 31, 415–425 (2017).
Silver, S. A. et al. Causes of death after a hospitalization with AKI. J. Am. Soc. Nephrol. 29, 1001–1010 (2018). Study showing that cancer-related and cardiovascular deaths occurred at substantially higher rates than in the general population after AKI.
Newsome, B. B. et al. Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch. Intern. Med. 168, 609–616 (2008).
Parr, S. K. et al. Acute kidney injury is a risk factor for subsequent proteinuria. Kidney Int. 93, 460–469 (2018).
He, L. et al. AKI on CKD: heightened injury, suppressed repair, and the underlying mechanisms. Kidney Int. 92, 1071–1083 (2017).
Hsu, C. Y. et al. Elevated BP after AKI. J. Am. Soc. Nephrol. 27, 914–923 (2016). Study showing high incidence of hypertension after AKI.
Gammelager, H. et al. Three-year risk of cardiovascular disease among intensive care patients with acute kidney injury: a population-based cohort study. Crit. Care 18, 492 (2014).
Wu, V. C. et al. Long-term risk of coronary events after AKI. J. Am. Soc. Nephrol. 25, 595–605 (2014).
Odutayo, A. et al. AKI and long-term risk for cardiovascular events and mortality. J. Am. Soc. Nephrol. 28, 377–387 (2017).
Xue, J. L. et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J. Am. Soc. Nephrol. 17, 1135–1142 (2006).
Loef, B. G. et al. Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J. Am. Soc. Nephrol. 16, 195–200 (2005).
Coca, S. G., Yusuf, B., Shlipak, M. G., Garg, A. X. & Parikh, C. R. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am. J. Kidney Dis. 53, 961–973 (2009).
Peired, A. J. et al. Acute kidney injury promotes development of papillary renal cell adenoma and carcinoma from renal progenitor cells. Sci. Transl. Med. 12, eaaw6003 (2020).
Zhou, X. et al. Acute kidney injury instigates malignant renal cell carcinoma via CXCR2 in mice with inactivated Trp53 and Pten in proximal tubular kidney epithelial cells. Cancer Res. 81, 2690–2702 (2021).
Verine, J. et al. Human de novo papillary renal-cell carcinomas in a kidney graft: evidence of recipient origin with adenoma-carcinoma sequence. Am. J. Transpl. 13, 984–992 (2013).
Chertow, G. M., Burdick, E., Honour, M., Bonventre, J. V. & Bates, D. W. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 16, 3365–3370 (2005).
Lassnigg, A. et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J. Am. Soc. Nephrol. 15, 1597–1605 (2004).
Vanmassenhove, J. et al. Urinary output and fractional excretion of sodium and urea as indicators of transient versus intrinsic acute kidney injury during early sepsis. Crit. Care 17, R234 (2013).
Hoste, E. A. et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit. Care 10, R73 (2006).
Hsu, C. Y. et al. Nonrecovery of kidney function and death after acute on chronic renal failure. Clin. J. Am. Soc. Nephrol. 4, 891–898 (2009).
Hsu, C. Y. et al. The risk of acute renal failure in patients with chronic kidney disease. Kidney Int. 74, 101–107 (2008).
Ishani, A. et al. Acute kidney injury increases risk of ESRD among elderly. J. Am. Soc. Nephrol. 20, 223–228 (2009).
Lafrance, J. P., Djurdjev, O. & Levin, A. Incidence and outcomes of acute kidney injury in a referred chronic kidney disease cohort. Nephrol. Dial. Transpl. 25, 2203–2209 (2010).
Pannu, N. et al. Modification of outcomes after acute kidney injury by the presence of CKD. Am. J. Kidney Dis. 58, 206–213 (2011).
Waikar, S. S. & Bonventre, J. V. Creatinine kinetics and the definition of acute kidney injury. J. Am. Soc. Nephrol. 20, 672–679 (2009).
Broce, J. C., Price, L. L., Liangos, O., Uhlig, K. & Jaber, B. L. Hospital-acquired acute kidney injury: an analysis of nadir-to-peak serum creatinine increments stratified by baseline estimated GFR. Clin. J. Am. Soc. Nephrol. 6, 1556–1565 (2011).
Chen, J. J., Chang, C. H., Huang, Y. T. & Kuo, G. Furosemide stress test as a predictive marker of acute kidney injury progression or renal replacement therapy: a systemic review and meta-analysis. Crit. Care 24, 202 (2020).
Kellum, J. A. et al. Classifying AKI by urine output versus serum creatinine level. J. Am. Soc. Nephrol. 26, 2231–2238 (2015).
Priyanka, P. et al. The impact of acute kidney injury by serum creatinine or urine output criteria on major adverse kidney events in cardiac surgery patients. J. Thorac. Cardiovasc. Surg. https://doi.org/10.1016/j.jtcvs.2019.11.137 (2020).
Pottel, H., Mottaghy, F. M., Zaman, Z. & Martens, F. On the relationship between glomerular filtration rate and serum creatinine in children. Pediatr. Nephrol. 25, 927–934 (2010).
Schwartz, G. J. & Work, D. F. Measurement and estimation of GFR in children and adolescents. Clin. J. Am. Soc. Nephrol. 4, 1832–1843 (2009).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Schwartz, G. J., Haycock, G. B., Edelmann, C. M. Jr. & Spitzer, A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58, 259–263 (1976).
Plotz, F. B., Bouma, A. B., van Wijk, J. A., Kneyber, M. C. & Bokenkamp, A. Pediatric acute kidney injury in the ICU: an independent evaluation of pRIFLE criteria. Intensive Care Med. 34, 1713–1717 (2008).
Kaddourah, A., Basu, R. K., Bagshaw, S. M., Goldstein, S. L. & Investigators, A. Epidemiology of acute kidney injury in critically Ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Endre, Z. H. et al. Improved performance of urinary biomarkers of acute kidney injury in the critically ill by stratification for injury duration and baseline renal function. Kidney Int. 79, 1119–1130 (2011).
McCullough, P. A. et al. Implementation of novel biomarkers in the diagnosis, prognosis, and management of acute kidney injury: executive summary from the tenth consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib. Nephrol. 182, 5–12 (2013).
Murray, P. T. et al. Potential use of biomarkers in acute kidney injury: report and summary of recommendations from the 10th Acute Dialysis Quality Initiative consensus conference. Kidney Int. 85, 513–521 (2014).
Bagshaw, S. M., Zappitelli, M. & Chawla, L. S. Novel biomarkers of AKI: the challenges of progress ‘amid the noise and the haste’. Nephrol. Dial. Transpl. 28, 235–238 (2013).
Lameire, N. H., Vanholder, R. C. & Van Biesen, W. A. How to use biomarkers efficiently in acute kidney injury. Kidney Int. 79, 1047–1050 (2011).
Vanmassenhove, J., Vanholder, R., Nagler, E. & Van Biesen, W. Urinary and serum biomarkers for the diagnosis of acute kidney injury: an in-depth review of the literature. Nephrol. Dial. Transpl. 28, 254–273 (2013).
Goldstein, S. L. & Chawla, L. S. Renal angina. Clin. J. Am. Soc. Nephrol. 5, 943–949 (2010).
Cai, L., Rubin, J., Han, W., Venge, P. & Xu, S. The origin of multiple molecular forms in urine of HNL/NGAL. Clin. J. Am. Soc. Nephrol. 5, 2229–2235 (2010).
Devarajan, P. Review: neutrophil gelatinase-associated lipocalin: a troponin-like biomarker for human acute kidney injury. Nephrology 15, 419–428 (2010).
Mishra, P. K. et al. Long-term quality of life postacute kidney injury in cardiac surgery patients. Ann. Card. Anaesth. 21, 41–45 (2018).
Makris, K. et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) as an early marker of acute kidney injury in critically ill multiple trauma patients. Clin. Chem. Lab. Med. 47, 79–82 (2009).
McIlroy, D. R., Wagener, G. & Lee, H. T. Neutrophil gelatinase-associated lipocalin and acute kidney injury after cardiac surgery: the effect of baseline renal function on diagnostic performance. Clin. J. Am. Soc. Nephrol. 5, 211–219 (2010).
Perrotti, A. et al. Neutrophil gelatinase-associated lipocalin as early predictor of acute kidney injury after cardiac surgery in adults with chronic kidney failure. Ann. Thorac. Surg. 99, 864–869 (2015).
Doi, K. et al. Plasma neutrophil gelatinase-associated lipocalin in acute kidney injury superimposed on chronic kidney disease after cardiac surgery: a multicenter prospective study. Crit. Care 17, R270 (2013).
Kashani, K. et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit. Care 17, R25 (2013).
Bihorac, A. & Kellum, J. A. Acute kidney injury in 2014: a step towards understanding mechanisms of renal repair. Nat. Rev. Nephrol. 11, 74–75 (2015).
Hoste, E. A. et al. Urinary cell cycle arrest biomarkers and chitinase 3-like protein 1 (CHI3L1) to detect acute kidney injury in the critically ill: a post hoc laboratory analysis on the FINNAKI cohort. Crit. Care 24, 144 (2020).
Waskowski, J. et al. (TIMP2) x (IGFBP7) as early renal biomarker for the prediction of acute kidney injury in aortic surgery (TIGER). A single center observational study. PLoS ONE 16, e0244658 (2021).
Witzgall, R. Are renal proximal tubular epithelial cells constantly prepared for an emergency? Focus on “the proliferation capacity of the renal proximal tubule involves the bulk of differentiated epithelial cells”. Am. J. Physiol. Cell Physiol. 294, C1–C3 (2008).
Meersch, M. et al. Urinary TIMP-2 and IGFBP7 as early biomarkers of acute kidney injury and renal recovery following cardiac surgery. PLoS ONE 9, e93460 (2014).
Aregger, F. et al. Identification of IGFBP-7 by urinary proteomics as a novel prognostic marker in early acute kidney injury. Kidney Int. 85, 909–919 (2014).
Koyner, J. L. et al. Tissue inhibitor metalloproteinase-2 (TIMP-2)IGF-binding protein-7 (IGFBP7) levels are associated with adverse long-term outcomes in patients with AKI. J. Am. Soc. Nephrol. 26, 1747–1754 (2015).
Joannidis, M. et al. Use of cell cycle arrest biomarkers in conjunction with classical markers of acute kidney injury. Crit. Care Med. 47, e820–e826 (2019).
Xie, Y. et al. Tissue inhibitor metalloproteinase-2 (TIMP-2) • IGF-binding protein-7 (IGFBP7) levels are associated with adverse outcomes in patients in the intensive care unit with acute kidney injury. Kidney Int. 95, 1486–1493 (2019).
Ronco, C., Kellum, J. A. & Haase, M. Subclinical AKI is still AKI. Crit. Care 16, 313 (2012).
Haase, M. et al. The outcome of neutrophil gelatinase-associated lipocalin-positive subclinical acute kidney injury: a multicenter pooled analysis of prospective studies. J. Am. Coll. Cardiol. 57, 1752–1761 (2011).
Endre, Z. H., Pickering, J. W. & Walker, R. J. Clearance and beyond: the complementary roles of GFR measurement and injury biomarkers in acute kidney injury (AKI). Am. J. Physiol. Ren. Physiol. 301, F697–F707 (2011).
Rabito, C. A., Panico, F., Rubin, R., Tolkoff-Rubin, N. & Teplick, R. Noninvasive, real-time monitoring of renal function during critical care. J. Am. Soc. Nephrol. 4, 1421–1428 (1994).
Herrera-Gutierrez, M. E. et al. Replacement of 24-h creatinine clearance by 2-h creatinine clearance in intensive care unit patients: a single-center study. Intensive Care Med. 33, 1900–1906 (2007).
Pickering, J. W., Frampton, C. M., Walker, R. J., Shaw, G. M. & Endre, Z. H. Four hour creatinine clearance is better than plasma creatinine for monitoring renal function in critically ill patients. Crit. Care 16, R107 (2012).
Schieppati, A., Perico, N. & Remuzzi, G. Eliminating treatable deaths due to acute kidney injury in resource-poor settings. Semin. Dial. 28, 193–197 (2015).
Meersch, M. et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med. 43, 1551–1561 (2017).
Engelman, D. T. et al. Using urinary biomarkers to reduce acute kidney injury following cardiac surgery. J. Thorac. Cardiovasc. Surg. 160, 1235–1246.e2 (2020).
Göcze, I. et al. Biomarker-guided intervention to prevent acute kidney injury after major surgery: the prospective randomized BigpAK Study. Ann. Surg. 267, 1013–1020 (2018).
Küllmar, M. et al. A multinational observational study exploring adherence with the kidney disease: improving global outcomes recommendations for prevention of acute kidney injury after cardiac surgery. Anesth. Analg. 130, 910–916 (2020).
Al-Jaghbeer, M., Dealmeida, D., Bilderback, A., Ambrosino, R. & Kellum, J. A. Clinical decision support for in-hospital AKI. J. Am. Soc. Nephrol. 29, 654–660 (2018).
Ostermann, M. et al. Controversies in acute kidney injury: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) conference. Kidney Int. 98, 294–309 (2020).
Prowle, J. R., Echeverri, J. E., Ligabo, E. V., Ronco, C. & Bellomo, R. Fluid balance and acute kidney injury. Nat. Rev. Nephrol. 6, 107–115 (2010).
Busse, L. W. & Ostermann, M. Vasopressor therapy and blood pressure management in the setting of acute kidney injury. Semin. Nephrol. 39, 462–472 (2019).
Xu, J. Y. et al. A high mean arterial pressure target is associated with improved microcirculation in septic shock patients with previous hypertension: a prospective open label study. Crit. Care 19, 130 (2015).
Asfar, P. et al. High versus low blood-pressure target in patients with septic shock. N. Engl. J. Med. 370, 1583–1593 (2014).
Lamontagne, F. et al. Pooled analysis of higher versus lower blood pressure targets for vasopressor therapy septic and vasodilatory shock. Intensive Care Med. 44, 12–21 (2018).
Futier, E. et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA 318, 1346–1357 (2017).
Dalfino, L., Tullo, L., Donadio, I., Malcangi, V. & Brienza, N. Intra-abdominal hypertension and acute renal failure in critically ill patients. Intensive Care Med. 34, 707–713 (2008).
Pinsky, M. R. Functional hemodynamic monitoring. Crit. Care Clin. 31, 89–111 (2015).
Scheeren, T. W. L. et al. Current use of vasopressors in septic shock. Ann. Intensive Care 9, 20 (2019).
Rodriguez, R., Cucci, M., Kane, S., Fernandez, E. & Benken, S. Novel vasopressors in the treatment of vasodilatory shock: a systematic review of angiotensin II, selepressin, and terlipressin. J. Intensive Care Med. 35, 327–337 (2020).
Semler, M. W. et al. Balanced crystalloids versus saline in critically ill adults. N. Engl. J. Med. 378, 829–839 (2018).
Self, W. H. et al. Balanced crystalloids versus saline in noncritically ill adults. N. Engl. J. Med. 378, 819–828 (2018).
Bellomo, R., Kellum, J. A. & Ronco, C. Acute kidney injury. Lancet 380, 756–766 (2012).
Patschan, D., Patschan, S., Buschmann, I. & Ritter, O. Loop diuretics in acute kidney injury prevention, therapy, and risk stratification. Kidney Blood Press Res. 44, 457–464 (2019).
Peng, J. et al. Hyperglycemia, p53, and mitochondrial pathway of apoptosis are involved in the susceptibility of diabetic models to ischemic acute kidney injury. Kidney Int. 87, 137–150 (2015).
Lok, C. E. et al. KDOQI clinical practice guideline for vascular access: 2019 update. Am. J. Kidney Dis. 75, S1–s164 (2020).
O’Grady, N. P. et al. Guidelines for the prevention of intravascular catheter-related infections. Clin. Infect. Dis. 52, e162–e193 (2011).
Mehta, R. L. et al. Sepsis as a cause and consequence of acute kidney injury: program to improve care in acute renal disease. Intensive Care Med. 37, 241–248 (2011).
Formeck, C. L., Joyce, E. L., Fuhrman, D. Y. & Kellum, J. A. Association of acute kidney injury with subsequent sepsis in critically Ill children. Pediatr. Crit. Care Med. 22, e58–e66 (2020).
Singbartl, K. et al. Differential effects of kidney-lung cross-talk during acute kidney injury and bacterial pneumonia. Kidney Int. 80, 633–644 (2011).
Singbartl, K., Miller, L., Ruiz-Velasco, V. & Kellum, J. A. Reversal of acute kidney injury-induced neutrophil dysfunction: a critical role for resistin. Crit. Care Med. 44, e492–e501 (2016).
Palant, C. E., Patel, S. S. & Chawla, L. S. Acute kidney injury recovery. Contrib. Nephrol. 193, 35–44 (2018).
Hoste, E. et al. Identification and validation of biomarkers of persistent acute kidney injury: the RUBY study. Intensive Care Med. 46, 943–953 (2020).
Karsanji, D. J. et al. Disparity between nephrologists’ opinions and contemporary practices for community follow-up after AKI hospitalization. Clin. J. Am. Soc. Nephrol. 12, 1753–1761 (2017).
Kashani, K. et al. Quality improvement goals for acute kidney injury. Clin. J. Am. Soc. Nephrol. 14, 941–953 (2019).
McCulloch, M. et al. Challenges of access to kidney care for children in low-resource settings. Nat. Rev. Nephrol. 17, 33–45 (2021).
Callegari, J. et al. Peritoneal dialysis as a mode of treatment for acute kidney injury in sub-Saharan Africa. Blood Purif. 36, 226–230 (2013).
Cullis, B. et al. ISPD guidelines for peritoneal dialysis in acute kidney injury: 2020 update (adults). Perit. Dial. 41, 15–31 (2021).
Ponce, D., Berbel, M. N., Abrão, J. M., Goes, C. R. & Balbi, A. L. A randomized clinical trial of high volume peritoneal dialysis versus extended daily hemodialysis for acute kidney injury patients. Int. Urol. Nephrol. 45, 869–878 (2013).
Karkar, A. & Ronco, C. Prescription of CRRT: a pathway to optimize therapy. Ann. Intensive Care 10, 32 (2020).
Balgobin, S. et al. Continuous veno-venous high cut-off hemodialysis compared to continuous veno-venous hemodiafiltration in intensive care unit acute kidney injury patients. Blood Purif. 46, 248–256 (2018).
De Rosa, S., Villa, G. & Ronco, C. The golden hour of polymyxin B hemoperfusion in endotoxic shock: the basis for sequential extracorporeal therapy in sepsis. Artif. Organs 44, 184–186 (2020).
Zarbock, A. et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically Ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA 315, 2190–2199 (2016).
Gaudry, S. et al. Timing of renal support and outcome of septic shock and acute respiratory distress syndrome. a post hoc analysis of the AKIKI randomized clinical trial. Am. J. Respir. Crit. Care Med. 198, 58–66 (2018).
Barbar, S. D. et al. Timing of renal-replacement therapy in patients with acute kidney injury and sepsis. N. Engl. J. Med. 379, 1431–1442 (2018). Study showing that among critically ill patients with AKI an accelerated renal replacement strategy is not associated with a lower risk of death than a standard strategy.
Ronco, C. et al. Continuous renal replacement therapy in neonates and small infants: development and first-in-human use of a miniaturised machine (CARPEDIEM). Lancet 383, 1807–1813 (2014). Study reporting a new miniaturised machine that can provide various dialytic treatments and support for multiple organ dysfunction in neonates and small infants.
Garzotto, F. et al. Continuous kidney replacement therapy in critically ill neonates and infants: a retrospective analysis of clinical results with a dedicated device. Pediatr. Nephrol. 35, 1699–1705 (2020).
Villeneuve, P. M., Clark, E. G., Sikora, L., Sood, M. M. & Bagshaw, S. M. Health-related quality-of-life among survivors of acute kidney injury in the intensive care unit: a systematic review. Intensive Care Med. 42, 137–146 (2016). Study reporting that physical limitations and disabilities were more commonly exhibited by AKI patients.
Stengel, B. et al. Risk profile, quality of life and care of patients with moderate and advanced CKD: The French CKD-REIN Cohort Study. Nephrol. Dial. Transpl. 34, 277–286 (2019).
Richardson, K. L., Watson, R. S. & Hingorani, S. Quality of life following hospitalization-associated acute kidney injury in children. J. Nephrol. 31, 249–256 (2018).
Korkeila, M., Ruokonen, E. & Takala, J. Costs of care, long-term prognosis and quality of life in patients requiring renal replacement therapy during intensive care. Intensive Care Med. 26, 1824–1831 (2000).
Morsch, C., Thomé, F. S., Balbinotto, A., Guimarães, J. F. & Barros, E. G. Health-related quality of life and dialysis dependence in critically ill patient survivors of acute kidney injury. Ren. Fail. 33, 949–956 (2011).
Morgera, S., Kraft, A. K., Siebert, G., Luft, F. C. & Neumayer, H. H. Long-term outcomes in acute renal failure patients treated with continuous renal replacement therapies. Am. J. Kidney Dis. 40, 275–279 (2002).
Wang, A. Y. et al. Health-related quality of life in survivors of acute kidney injury: the prolonged outcomes study of the randomized evaluation of normal versus augmented level replacement therapy study outcomes. Nephrology 20, 492–498 (2015).
Akbar, S. & Moss, A. H. The ethics of offering dialysis for AKI to the older patient: time to re-evaluate? Clin. J. Am. Soc. Nephrol. 9, 1652–1656 (2014).
Oeyen, S. et al. Long-term quality of life in critically ill patients with acute kidney injury treated with renal replacement therapy: a matched cohort study. Crit. Care 19, 289 (2015).
Charlton, J. R. et al. Magnetic resonance imaging accurately tracks kidney pathology and heterogeneity in the transition from acute kidney injury to chronic kidney disease. Kidney Int. 99, 173–185 (2021).
Huang, J., Li, J., Lyu, Y., Miao, Q. & Pu, K. Molecular optical imaging probes for early diagnosis of drug-induced acute kidney injury. Nat. Mater. 18, 1133–1143 (2019).
Schneider, A. G. & Molitoris, B. A. Real-time glomerular filtration rate: improving sensitivity, accuracy and prognostic value in acute kidney injury. Curr. Opin. Crit. Care 26, 549–555 (2020).
Pickkers, P. et al. Alkaline phosphatase for treatment of sepsis-induced acute kidney injury: a prospective randomized double-blind placebo-controlled trial. Crit. Care 16, R14 (2012).
Pickkers, P. et al. Effect of human recombinant alkaline phosphatase on 7-day creatinine clearance in patients with sepsis-associated acute kidney injury: a randomized clinical trial. JAMA 320, 1998–2009 (2018).
Hoste, E. A. et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 41, 1411–1423 (2015).
Srisawat, N. et al. The epidemiology and characteristics of acute kidney injury in the Southeast Asia intensive care unit: a prospective multicentre study. Nephrol. Dial. Transpl. 35, 1729–1738 (2020).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child. Adolesc. Health 1, 184–194 (2017). Study reporting a high incidence of AKI in neonatal setting and its role as a common and independent risk factor for mortality and longer hospital stay.
National Clinical Guideline Centre. in Acute Kidney Injury: Prevention, Detection and Management Up to the Point of Renal Replacement Therapy 1–26 (National Clinical Guideline Centre, 2013).
Rondeau, E., Faguer, S. & Robert, T. Advocacy for a European network of renal intensive care units. Nephrol. Dial. Transpl. 34, 1262–1264 (2019).
Massy, Z. A. et al. Nephrology and public policy committee propositions to stimulate research collaboration in adults and children in Europe. Nephrol. Dial. Transpl. 34, 1469–1480 (2019).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3, 1–150 (2013).
Scheel, P. J., Liu, M. & Rabb, H. Uremic lung: new insights into a forgotten condition. Kidney Int. 74, 849–851 (2008).
Chan, L. et al. AKI in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 32, 151−160 (2020). Study reporting the high incidence of AKI in patients with Covid-19.
Hirsch, J. S. et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 98, 209–218 (2020).
Chan, L. & Coca, S. G. Acute kidney injury in the time of COVID-19. Kidney 360 1, 588–590 (2020).
Price-Haywood, E. G., Burton, J., Fort, D. & Seoane, L. Hospitalization and mortality among black patients and white patients with Covid-19. N. Engl. J. Med. 382, 2534–2543 (2020).
Su, H. et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 98, 219–227 (2020).
Nicolai, L. et al. Immunothrombotic dysregulation in covid-19 pneumonia is associated with respiratory failure and coagulopathy. Circulation 142, 1176–1189 (2020).
Santoriello, D. et al. Postmortem kidney pathology findings in patients with COVID-19. J. Am. Soc. Nephrol. 31, 2158–2167 (2020).
Braun, F. et al. SARS-CoV-2 renal tropism associates with acute kidney injury. Lancet 396, 597–598 (2020).
Roufosse, C. et al. Electron microscopic investigations in COVID-19: not all crowns are coronas. Kidney Int. 98, 505–506 (2020).
Nadim, M. K. et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat. Rev. Nephrol. 16, 747–764 (2020).
Gupta, S. et al. AKI treated with renal replacement therapy in critically ill patients with COVID-19. J. Am. Soc. Nephrol. 32, 161−176 (2020).
Acknowledgements
The European Research Council under the Consolidator Grant RENOIR supported P.R. (ERC-2014-CoG, grant number 648274). The Deutsche Forschungsgemeinschaft supported H.-J.A. (AN372/14-4, AN372/16-2, AN372/20-2, AN372/27-1 and AN372/30-1) and A.Z. (KFO342/1, ZA428/18-1 and ZA428/21-1). J.A.K. is supported by a grant (UH3DK114861) from the National Institute of Diabetes and Kidney Disease (NIDDK).
Author information
Authors and Affiliations
Contributions
Sections of the Primer were written by the authors as follows: Introduction (H.-J.A., J.A.K.); Epidemiology (H.-J.A., J.A.K., G.A.); Mechanisms/pathophysiology (P.R., H.-J.A.); Diagnosis, screening and prevention (H.-J.A., A.Z.); Management (H.-J.A., J.A.K., C.R.); Quality of life (H.J.A.); Outlook (H.-J.A., P.R.); Overview of the Primer (H.-J.A.).
Corresponding author
Ethics declarations
Competing interests
H.-J.A. received consultancy fees from Bayer, Boehringer, AstraZeneca, Janssen, Novartis, GlaxoSmithKline, Previpharma, Inositec and Secarna, unrelated to this publication. J.A.K. received consulting fees and/or grant support from Baxter, NxStage and Astute Medical/BioMerieux. J.A.K. became a full-time employee of Spectral Medical after submission of this manuscript. C.R. has been consulting or part of advisory boards for Asahi Kasei Pharma, Astute, Baxter, Biomerieux, B. Braun, Cytosorbents, Estor, Fresenius Medical Care, General Electric, Jafron, Medtronic and Toray. A.Z. has received consulting and/or lecture fees from Astute Medical/BioMerieux, Fresenius, Baxter, AM Pharma, La Jolla Pharmaceuticals and Astellas. A.Z. has received grant support from Astute Medical/BioMerieux, unrelated to this publication. G.A. and P.R. declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks M. Ostermann, R. Evans, E. Daher, who co-reviewed with G. C. Meneses, K. Doi, J. Prowle, S. Menez, D. Ponce, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Hepatorenal syndrome
-
Impaired kidney perfusion and function in patients with advanced liver failure as a consequence of marked abnormalities in arterial and venous circulation, as well as overactivity of endogenous vasoactive systems.
- Kidney failure
-
Complete (and life-threatening) loss of kidney function; kidney failure replaces the term end-stage kidney disease in new nomenclature put forward by the KDIGO.
- Glomerular filtration rate
-
The volume of filtrate passing the glomerular filtration barrier per unit of time; a marker of excretory kidney function.
- Third-space effusions
-
Accumulation of fluid in body cavities.
- Pulmonary congestion
-
An accumulation of fluid in the lungs, resulting in impaired gas exchange and arterial hypoxaemia.
- Fixed acid
-
An acid that accumulates in the body as a result of digestion, disease or metabolism and cannot be excreted by the lungs (non-volatile or fixed).
- Anion gap
-
The difference between the sum of routinely measured cations (Na+ and K+) and the sum of routinely measured anions (Cl− and HCO3−) in serum.
- Azotaemia
-
Abnormally high levels of nitrogen-containing compounds in the blood, occurring when the kidneys are no longer able to excrete nitrogen waste products via the urine.
- Venous congestion
-
A distention of veins filled with blood as a result of mechanical obstruction or right ventricular failure.
- Acute tubular necrosis
-
A form of AKI that involves loss of entire tubule segments due to necrotic death of tubular epithelial cells.
- Fluid resuscitation
-
Large-volume intravenous fluid replacement to treat AKI and circulatory shock due to severe intravascular volume depletion.
- G1 phase
-
The G1 phase is the first of four cell cycle phases that takes place in eukaryotic cell division and describes the period from the end of cell division to the beginning of DNA replication.
- Peritoneal dialysis
-
A treatment for kidney failure that uses the inside lining of the abdomen as a filtration membrane via intermittent filling and emptying of the peritoneal cavity with a dialysate solution to extract salt, uraemic toxins and other solutes from the blood.
Rights and permissions
About this article
Cite this article
Kellum, J.A., Romagnani, P., Ashuntantang, G. et al. Acute kidney injury. Nat Rev Dis Primers 7, 52 (2021). https://doi.org/10.1038/s41572-021-00284-z
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-021-00284-z
This article is cited by
-
Pediatric acute kidney injury following bee sting-induced anaphylaxis: a case series
Journal of Medical Case Reports (2026)
-
Ginsenoside Rb1 targets the NRF2-PPARγ-ACSL4 axis to inhibit PTECs ferroptosis
Chinese Medicine (2026)
-
Effects of social determinants of health on the landscape of kidney disease
Nature Reviews Nephrology (2026)
-
Multifactorial chronic kidney disease and the kidney capacity–workload balance
Nature Reviews Nephrology (2026)
-
The impact of urine output trajectory on clinical outcomes in female patients with genitourinary infections in the intensive care unit
Scientific Reports (2026)