Abstract
Cholangiocarcinoma (CCA) is a highly lethal adenocarcinoma of the hepatobiliary system, which can be classified as intrahepatic, perihilar and distal. Each anatomic subtype has distinct genetic aberrations, clinical presentations and therapeutic approaches. In endemic regions, liver fluke infection is associated with CCA, owing to the oncogenic effect of the associated chronic biliary tract inflammation. In other regions, CCA can be associated with chronic biliary tract inflammation owing to choledocholithiasis, cholelithiasis, or primary sclerosing cholangitis, but most CCAs have no identifiable cause. Administration of the anthelmintic drug praziquantel decreases the risk of CCA from liver flukes, but reinfection is common and future vaccination strategies may be more effective. Some patients with CCA are eligible for potentially curative surgical options, such as resection or liver transplantation. Genetic studies have provided new insights into the pathogenesis of CCA, and two aberrations that drive the pathogenesis of non-fluke-associated intrahepatic CCA, fibroblast growth factor receptor 2 fusions and isocitrate dehydrogenase gain-of-function mutations, can be therapeutically targeted. CCA is a highly desmoplastic cancer and targeting the tumour immune microenvironment might be a promising therapeutic approach. CCA remains a highly lethal disease and further scientific and clinical insights are needed to improve patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Fan, B. et al. Cholangiocarcinomas can originate from hepatocytes in mice. J. Clin. Invest. 122, 2911–2915 (2012).
Nakagawa, H. et al. Biliary epithelial injury-induced regenerative response by IL-33 promotes cholangiocarcinogenesis from peribiliary glands. Proc. Natl Acad. Sci. USA 114, E3806–E3815 (2017).
Razumilava, N. & Gores, G. J. Cholangiocarcinoma. Lancet 383, 2168–2179 (2014).
Zhu, Y. & Kwong, L. N. Insights into the origin of intrahepatic cholangiocarcinoma from mouse models. Hepatology 72, 305–314 (2020).
Blechacz, B., Komuta, M., Roskams, T. & Gores, G. J. Clinical diagnosis and staging of cholangiocarcinoma. Nat. Rev. Gastroenterol. Hepatol. 8, 512–522 (2011). The first paper that describes the three anatomic subtypes of cholangiocarcinoma.
Cardinale, V. Classifications and misclassification in cholangiocarcinoma. Liver Int. 39, 260–262 (2019).
Khan, S. A., Tavolari, S. & Brandi, G. Cholangiocarcinoma: epidemiology and risk factors. Liver Int. 39, 19–31 (2019).
Hainsworth, J. D. et al. Molecular gene expression profiling to predict the tissue of origin and direct site-specific therapy in patients with carcinoma of unknown primary site: a prospective trial of the Sarah Cannon Research Institute. J. Clin. Oncol. 31, 217–223 (2013).
Varadhachary, G. R. & Raber, M. N. Cancer of unknown primary site. N. Engl. J. Med. 371, 757–765 (2014).
Rizvi, S., Khan, S. A., Hallemeier, C. L., Kelley, R. K. & Gores, G. J. Cholangiocarcinoma – evolving concepts and therapeutic strategies. Nat. Rev. Clin. Oncol. 15, 95–111 (2018).
Kendall, T. et al. Anatomical, histomorphological and molecular classification of cholangiocarcinoma. Liver Int. 39, 7–18 (2019).
Binnewies, M. et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 24, 541–550 (2018).
Sirica, A. E. et al. Intrahepatic cholangiocarcinoma: continuing challenges and translational advances. Hepatology 69, 1803–1815 (2019).
Fabris, L. et al. The tumour microenvironment and immune milieu of cholangiocarcinoma. Liver Int. 39, 63–78 (2019).
Sripa, B., Tangkawattana, S. & Brindley, P. J. Update on pathogenesis of opisthorchiasis and cholangiocarcinoma. Adv. Parasitol. 102, 97–113 (2018).
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Biological agents. Volume 100 B. A review of human carcinogens. IARC Monogr. Eval. Carcinog. Risks Hum. 100, 1–441 (2012).
Sripa, B. et al. Opisthorchiasis and opisthorchis-associated cholangiocarcinoma in Thailand and Laos. Acta Trop. 120, S158–168 (2011).
Qian, M. B., Utzinger, J., Keiser, J. & Zhou, X. N. Clonorchiasis. Lancet 387, 800–810 (2016).
Sripa, B. et al. Liver fluke induces cholangiocarcinoma. PLoS Med. 4, e201 (2007).
Schwartz, D. A. Helminths in the induction of cancer: Opisthorchis viverrini, Clonorchis sinensis and cholangiocarcinoma. Trop. Geogr. Med. 32, 95–100 (1980).
Sithithaworn, P., Yongvanit, P., Duenngai, K., Kiatsopit, N. & Pairojkul, C. Roles of liver fluke infection as risk factor for cholangiocarcinoma. J. Hepatobiliary Pancreat. Sci. 21, 301–308 (2014).
Ogorodova, L. M. et al. Opisthorchiasis: an overlooked danger. PLoS Negl. Trop. Dis. 9, e0003563 (2015).
Choi, B. I., Han, J. K., Hong, S. T. & Lee, K. H. Clonorchiasis and cholangiocarcinoma: etiologic relationship and imaging diagnosis. Clin. Microbiol. Rev. 17, 540–552 (2004).
Keiser, J. & Utzinger, J. Food-borne trematodiases. Clin. Microbiol. Rev. 22, 466–483 (2009).
Petney, T. N., Andrews, R. H., Saijuntha, W., Wenz-Mucke, A. & Sithithaworn, P. The zoonotic, fish-borne liver flukes Clonorchis sinensis, Opisthorchis felineus and Opisthorchis viverrini. Int. J. Parasitol. 43, 1031–1046 (2013).
Pakharukova, M. Y. & Mordvinov, V. A. The liver fluke Opisthorchis felineus: biology, epidemiology and carcinogenic potential. Trans. R. Soc. Trop. Med. Hyg. 110, 28–36 (2016).
Na, B. K., Pak, J. H. & Hong, S. J. Clonorchis sinensis and clonorchiasis. Acta Trop. 203, 105309 (2020).
Lai, Y. S., Zhou, X. N., Pan, Z. H., Utzinger, J. & Vounatsou, P. Risk mapping of clonorchiasis in the People’s Republic of China: a systematic review and Bayesian geostatistical analysis. PLoS Negl. Trop. Dis. 11, e0005239 (2017).
Qian, M. B., Chen, Y. D., Liang, S., Yang, G. J. & Zhou, X. N. The global epidemiology of clonorchiasis and its relation with cholangiocarcinoma. Infect. Dis. Poverty 1, 4 (2012).
Doanh, P. N. & Nawa, Y. Clonorchis sinensis and Opisthorchis spp. in Vietnam: current status and prospects. Trans. R. Soc. Trop. Med. Hyg. 110, 13–20 (2016).
Cho, S. H. et al. Prevalence of clonorchiasis in southern endemic areas of Korea in 2006. Korean J. Parasitol. 46, 133–137 (2008).
Sohn, W. M. et al. High endemicity with Clonorchis sinensis metacercariae in fish from yongjeon-cheon (Stream) in Cheongsong-gun, Gyeongsangbuk-do, Korea. Korean J. Parasitol. 59, 97–101 (2021).
Fedorova, O. S. et al. Opisthorchis felineus infection, risks, and morbidity in rural Western Siberia, Russian Federation. PLoS Negl. Trop. Dis. 14, e0008421 (2020).
Sripa, B., Kaewkes, S., Intapan, P. M., Maleewong, W. & Brindley, P. J. Food-borne trematodiases in Southeast Asia epidemiology, pathology, clinical manifestation and control. Adv. Parasitol. 72, 305–350 (2010).
Sithithaworn, P. et al. The current status of opisthorchiasis and clonorchiasis in the Mekong Basin. Parasitol. Int. 61, 10–16 (2012).
Sohn, W. M. et al. Low-grade endemicity of opisthorchiasis, Yangon, Myanmar. Emerg. Infect. Dis. 25, 1435–1437 (2019).
Namsanor, J. et al. Infection dynamics of opisthorchis viverrini metacercariae in cyprinid fishes from two endemic areas in Thailand and Lao PDR. Am. J. Trop. Med. Hyg. 102, 110–116 (2020).
Taylor-Robinson, S. D. et al. Increase in mortality rates from intrahepatic cholangiocarcinoma in England and Wales 1968-1998. Gut 48, 816–820 (2001).
Patel, T. Worldwide trends in mortality from biliary tract malignancies. BMC Cancer 2, 10 (2002).
Bertuccio, P. et al. Global trends in mortality from intrahepatic and extrahepatic cholangiocarcinoma. J. Hepatol. 71, 104–114 (2019).
Saha, S. K., Zhu, A. X., Fuchs, C. S. & Brooks, G. A. Forty-year trends in cholangiocarcinoma incidence in the U.S.: intrahepatic disease on the rise. Oncologist 21, 594–599 (2016).
Lepage, C. et al. Trends in the incidence and management of biliary tract cancer: a French population-based study. J. Hepatol. 54, 306–310 (2011).
Khan, S. A. et al. Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J. Hepatol. 37, 806–813 (2002).
Jepsen, P., Vilstrup, H., Tarone, R. E., Friis, S. & Sorensen, H. T. Incidence rates of intra- and extrahepatic cholangiocarcinomas in Denmark from 1978 through 2002. J. Natl Cancer Inst. 99, 895–897 (2007).
Banales, J. M. et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 17, 557–588 (2020).
Yao, K. J., Jabbour, S., Parekh, N., Lin, Y. & Moss, R. A. Increasing mortality in the United States from cholangiocarcinoma: an analysis of the National Center for Health Statistics Database. BMC Gastroenterol. 16, 117 (2016).
Khan, S. A. et al. Rising trends in cholangiocarcinoma: is the ICD classification system misleading us? J. Hepatol. 56, 848–854 (2012).
DeOliveira, M. L. et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann. Surg. 245, 755–762 (2007).
Nakeeb, A. et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann. Surg. 224, 463–473 (1996). discussion 473-465.
Selvadurai, S. et al. Cholangiocarcinoma miscoding in hepatobiliary centres. Eur. J. Surg. Oncol. 47, 635–639 (2021).
Bosman, F. T., Carneiro, F., Hruban, R. H. & Theise, N. D. WHO Classification of Tumours: Digestive System Tumours (IARC, 2019).
Clements, O., Eliahoo, J., Kim, J. U., Taylor-Robinson, S. D. & Khan, S. A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a systematic review and meta-analysis. J. Hepatol. 72, 95–103 (2020). This paper is an updated and comprehensive review and meta-analysis of cholangiocarcinoma risk factors.
Petrick, J. L. et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based study in SEER-Medicare. PLoS ONE 12, e0186643 (2017).
Chan-On, W. et al. Exome sequencing identifies distinct mutational patterns in liver fluke-related and non-infection-related bile duct cancers. Nat. Genet. 45, 1474–1478 (2013). This paper links aetiological exposures to distinct somatic mutations.
Jusakul, A. et al. Whole-genome and epigenomic landscapes of etiologically distinct subtypes of cholangiocarcinoma. Cancer Discov. 7, 1116–1135 (2017).
Nakamura, H. et al. Genomic spectra of biliary tract cancer. Nat. Genet. 47, 1003–1010 (2015). This paper provides a comprehensive molecular characterization of the different subtypes of biliary tract cancers.
Farshidfar, F. et al. Integrative genomic analysis of cholangiocarcinoma identifies distinct IDH-mutant molecular profiles. Cell Rep. 18, 2780–2794 (2017).
Jiao, Y. et al. Exome sequencing identifies frequent inactivating mutations in BAP1, ARID1A and PBRM1 in intrahepatic cholangiocarcinomas. Nat. Genet. 45, 1470–1473 (2013).
Liu, Z. H. et al. Whole-exome mutational and transcriptional landscapes of combined hepatocellular cholangiocarcinoma and intrahepatic cholangiocarcinoma reveal molecular diversity. Biochim. Biophys. Acta Mol. Basis Dis. 1864, 2360–2368 (2018).
Lowery, M. A. et al. Comprehensive molecular profiling of intrahepatic and extrahepatic cholangiocarcinomas: potential targets for intervention. Clin. Cancer Res. 24, 4154–4161 (2018).
Ong, C. K. et al. Exome sequencing of liver fluke-associated cholangiocarcinoma. Nat. Genet. 44, 690–693 (2012).
Zou, S. et al. Mutational landscape of intrahepatic cholangiocarcinoma. Nat. Commun. 5, 5696 (2014).
Chaisaingmongkol, J. et al. Common molecular subtypes among Asian hepatocellular carcinoma and cholangiocarcinoma. Cancer Cell 32, 57–70.e3 (2017).
Montal, R. et al. Molecular classification and therapeutic targets in extrahepatic cholangiocarcinoma. J. Hepatol. 73, 315–327 (2020). This paper is the most comprehensive, integrated genomic analysis of perihilar/distal cholangiocarcinoma to date.
Sia, D. et al. Massive parallel sequencing uncovers actionable FGFR2-PPHLN1 fusion and ARAF mutations in intrahepatic cholangiocarcinoma. Nat. Commun. 6, 6087 (2015).
Wu, Y. M. et al. Identification of targetable FGFR gene fusions in diverse cancers. Cancer Discov. 3, 636–647 (2013).
Kongpetch, S. et al. Lack of targetable FGFR2 fusions in endemic fluke-associated cholangiocarcinoma. JCO Glob. Oncol. 6, 628–638 (2020).
Suttiprapa, S. et al. Opisthorchis viverrini proteome and host–parasite interactions. Adv. Parasitol. 102, 45–72 (2018).
Siripongsakun, S. et al. Premalignant lesions of cholangiocarcinoma: characteristics on ultrasonography and MRI. Abdom. Radiol. 44, 2133–2146 (2019).
Wu, M. Y., Yiang, G. T., Cheng, P. W., Chu, P. Y. & Li, C. J. Molecular targets in hepatocarcinogenesis and implications for therapy. J. Clin. Med. 7, 213 (2018).
Sripa, B. et al. Advanced periductal fibrosis from infection with the carcinogenic human liver fluke Opisthorchis viverrini correlates with elevated levels of interleukin-6. Hepatology 50, 1273–1281 (2009).
Forrer, A. et al. Spatial distribution of, and risk factors for, Opisthorchis viverrini infection in southern Lao PDR. PLoS Negl. Trop. Dis. 6, e1481 (2012).
Lun, Z. R. et al. Clonorchiasis: a key foodborne zoonosis in China. Lancet Infect. Dis. 5, 31–41 (2005).
Thamavit, W., Bhamarapravati, N., Sahaphong, S., Vajrasthira, S. & Angsubhakorn, S. Effects of dimethylnitrosamine on induction of cholangiocarcinoma in Opisthorchis viverrini-infected Syrian golden hamsters. Cancer Res. 38, 4634–4639 (1978).
Pakharukova, M. Y., Zaparina, O. G., Kovner, A. V. & Mordvinov, V. A. Inhibition of Opisthorchis felineus glutathione-dependent prostaglandin synthase by resveratrol correlates with attenuation of cholangiocyte neoplasia in a hamster model of opisthorchiasis. Int. J. Parasitol. 49, 963–973 (2019).
Smout, M. J. et al. Carcinogenic parasite secretes growth factor that accelerates wound healing and potentially promotes neoplasia. PLoS Pathog. 11, e1005209 (2015).
Chaiyadet, S. et al. Carcinogenic liver fluke secretes extracellular vesicles that promote cholangiocytes to adopt a tumorigenic phenotype. J. Infect. Dis. 212, 1636–1645 (2015).
Arunsan, P. et al. Programmed knockout mutation of liver fluke granulin attenuates virulence of infection-induced hepatobiliary morbidity. eLife 8, e41463 (2019).
Brivio, S., Cadamuro, M., Fabris, L. & Strazzabosco, M. Molecular mechanisms driving cholangiocarcinoma invasiveness: an overview. Gene Expr. 18, 31–50 (2018).
Labib, P. L., Goodchild, G. & Pereira, S. P. Molecular pathogenesis of cholangiocarcinoma. BMC Cancer 19, 185 (2019).
Roy, S., Glaser, S. & Chakraborty, S. Inflammation and progression of cholangiocarcinoma: role of angiogenic and lymphangiogenic mechanisms. Front. Med 6, 293 (2019).
Servais, F. A. et al. Modulation of the IL-6-signaling pathway in liver cells by miRNAs targeting gp130, JAK1, and/or STAT3. Mol. Ther. Nucleic Acids 16, 419–433 (2019).
Alvaro, D. et al. Estrogens and insulin-like growth factor 1 modulate neoplastic cell growth in human cholangiocarcinoma. Am. J. Pathol. 169, 877–888 (2006).
Zavadil, J. & Bottinger, E. P. TGF-β and epithelial-to-mesenchymal transitions. Oncogene 24, 5764–5774 (2005).
Claperon, A. et al. EGF/EGFR axis contributes to the progression of cholangiocarcinoma through the induction of an epithelial-mesenchymal transition. J. Hepatol. 61, 325–332 (2014).
Miyamoto, M. et al. Prognostic significance of overexpression of c-Met oncoprotein in cholangiocarcinoma. Br. J. Cancer 105, 131–138 (2011).
Pant, K., Richard, S., Peixoto, E. & Gradilone, S. A. Role of glucose metabolism reprogramming in the pathogenesis of cholangiocarcinoma. Front. Med. 7, 113 (2020).
Phoomak, C. et al. Overexpression of O-GlcNAc-transferase associates with aggressiveness of mass-forming cholangiocarcinoma. Asian Pac. J. Cancer Prev. 13, 101–105 (2012).
Phoomak, C. et al. Mechanistic insights of O-GlcNAcylation that promote progression of cholangiocarcinoma cells via nuclear translocation of NF-κB. Sci. Rep. 6, 27853 (2016).
Phoomak, C. et al. O-GlcNAc-induced nuclear translocation of hnRNP-K is associated with progression and metastasis of cholangiocarcinoma. Mol. Oncol. 13, 338–357 (2019).
Saengboonmee, C., Seubwai, W., Wongkham, C. & Wongkham, S. Diabetes mellitus: possible risk and promoting factors of cholangiocarcinoma: association of diabetes mellitus and cholangiocarcinoma. Cancer Epidemiol. 39, 274–278 (2015).
Phoomak, C. et al. High glucose levels boost the aggressiveness of highly metastatic cholangiocarcinoma cells via O-GlcNAcylation. Sci. Rep. 7, 43842 (2017).
Saengboonmee, C., Seubwai, W., Pairojkul, C. & Wongkham, S. High glucose enhances progression of cholangiocarcinoma cells via STAT3 activation. Sci. Rep. 6, 18995 (2016).
Indramanee, S. et al. Terminal fucose mediates progression of human cholangiocarcinoma through EGF/EGFR activation and the Akt/Erk signaling pathway. Sci. Rep. 9, 17266 (2019).
Phoomak, C. et al. O-GlcNAcylation mediates metastasis of cholangiocarcinoma through FOXO3 and MAN1A1. Oncogene 37, 5648–5665 (2018).
Park, D. D. et al. Metastasis of cholangiocarcinoma is promoted by extended high-mannose glycans. Proc. Natl Acad. Sci. USA 117, 7633–7644 (2020).
Talabnin, K., Talabnin, C., Ishihara, M. & Azadi, P. Increased expression of the high-mannose M6N2 and NeuAc3H3N3M3N2F tri-antennary N-glycans in cholangiocarcinoma. Oncol. Lett. 15, 1030–1036 (2018).
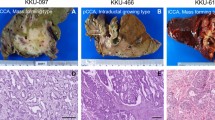
Nakanuma, Y. et al. Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J. Hepatol. 2, 419–427 (2010).
Banales, J. M. et al. Expert consensus document: Cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat. Rev. Gastroenterol. Hepatol. 13, 261–280 (2016).
Vijgen, S., Terris, B. & Rubbia-Brandt, L. Pathology of intrahepatic cholangiocarcinoma. Hepatobiliary Surg. Nutr. 6, 22–34 (2017).
Sirica, A. E. et al. Intrahepatic cholangiocarcinoma progression: prognostic factors and basic mechanisms. Clin. Gastroenterol. Hepatol. 7, S68–S78 (2009).
Bragazzi, M. C. et al. New insights into cholangiocarcinoma: multiple stems and related cell lineages of origin. Ann. Gastroenterol. 31, 42–55 (2018).
Akita, M. et al. Histological and molecular characterization of intrahepatic bile duct cancers suggests an expanded definition of perihilar cholangiocarcinoma. HPB 21, 226–234 (2019).
Bae, J. Y. et al. Intestinal type cholangiocarcinoma of intrahepatic large bile duct associated with hepatolithiasis–a new histologic subtype for further investigation. Hepatogastroenterology 49, 628–630 (2002).
Brunt, E. et al. cHCC-CCA: Consensus terminology for primary liver carcinomas with both hepatocytic and cholangiocytic differentation. Hepatology 68, 113–126 (2018).
Balitzer, D. et al. Immunohistochemical and molecular features of cholangiolocellular carcinoma are similar to well-differentiated intrahepatic cholangiocarcinoma. Mod. Pathol. 32, 1486–1494 (2019).
Brivio, S., Cadamuro, M., Strazzabosco, M. & Fabris, L. Tumor reactive stroma in cholangiocarcinoma: the fuel behind cancer aggressiveness. World J. Hepatol. 9, 455–468 (2017).
Bosmuller, H. et al. Microvessel density and angiogenesis in primary hepatic malignancies: differential expression of CD31 and VEGFR-2 in hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Pathol. Res. Pract. 214, 1136–1141 (2018).
Xu, J. et al. Intrahepatic cholangiocarcinomas in cirrhosis are hypervascular in comparison with those in normal livers. Liver Int. 32, 1156–1164 (2012).
Cadamuro, M. et al. The deleterious interplay between tumor epithelia and stroma in cholangiocarcinoma. Biochim. Biophys. Acta Mol. Basis Dis. 1864, 1435–1443 (2018).
Loeuillard, E., Conboy, C. B., Gores, G. J. & Rizvi, S. Immunobiology of cholangiocarcinoma. JHEP Rep. 1, 297–311 (2019).
Vaquero, J., Aoudjehane, L. & Fouassier, L. Cancer-associated fibroblasts in cholangiocarcinoma. Curr. Opin. Gastroenterol. 36, 63–69 (2020).
Affo, S. et al. Promotion of cholangiocarcinoma growth by diverse cancer-associated fibroblast subpopulations. Cancer Cell. 39, 866–882.e11 (2021). The first paper to describe subtypes of cancer-associated fibroblasts in cholangiocarcinoma.
Sahai, E. et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat. Rev. Cancer 20, 174–186 (2020).
Alvaro, D. et al. Cholangiocarcinoma in Italy: a national survey on clinical characteristics, diagnostic modalities and treatment. Results from the “Cholangiocarcinoma” committee of the Italian Association for the Study of Liver disease. Dig. Liver Dis. 43, 60–65 (2011).
Patel, A. H., Harnois, D. M., Klee, G. G., LaRusso, N. F. & Gores, G. J. The utility of CA 19-9 in the diagnoses of cholangiocarcinoma in patients without primary sclerosing cholangitis. Am. J. Gastroenterol. 95, 204–207 (2000).
Kim, M. J., Choi, J. Y. & Chung, Y. E. Evaluation of biliary malignancies using multidetector-row computed tomography. J. Comput. Assist. Tomogr. 34, 496–505 (2010).
Wildner, D. et al. CEUS in hepatocellular carcinoma and intrahepatic cholangiocellular carcinoma in 320 patients–early or late washout matters: a subanalysis of the DEGUM multicenter trial. Ultraschall Med. 36, 132–139 (2015).
Iavarone, M. et al. Contrast enhanced CT-scan to diagnose intrahepatic cholangiocarcinoma in patients with cirrhosis. J. Hepatol. 58, 1188–1193 (2013).
Kim, S. H. et al. Typical and atypical imaging findings of intrahepatic cholangiocarcinoma using gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging. J. Comput. Assist. Tomogr. 36, 704–709 (2012).
Choi, S. H. et al. Intrahepatic cholangiocarcinoma in patients with cirrhosis: differentiation from hepatocellular carcinoma by using gadoxetic acid-enhanced MR imaging and dynamic CT. Radiology 282, 771–781 (2017).
Vilana, R. et al. Intrahepatic peripheral cholangiocarcinoma in cirrhosis patients may display a vascular pattern similar to hepatocellular carcinoma on contrast-enhanced ultrasound. Hepatology 51, 2020–2029 (2010).
Petrowsky, H. et al. Impact of integrated positron emission tomography and computed tomography on staging and management of gallbladder cancer and cholangiocarcinoma. J. Hepatol. 45, 43–50 (2006).
Lamarca, A. et al. (18)F-fluorodeoxyglucose positron emission tomography ((18)FDG-PET) for patients with biliary tract cancer: systematic review and meta-analysis. J. Hepatol. 71, 115–129 (2019).
Jhaveri, K. S. & Hosseini-Nik, H. MRI of cholangiocarcinoma. J. Magn. Reson. Imaging 42, 1165–1179 (2015).
Saluja, S. S., Sharma, R., Pal, S., Sahni, P. & Chattopadhyay, T. K. Differentiation between benign and malignant hilar obstructions using laboratory and radiological investigations: a prospective study. HPB 9, 373–382 (2007).
Trikudanathan, G., Navaneethan, U., Njei, B., Vargo, J. J. & Parsi, M. A. Diagnostic yield of bile duct brushings for cholangiocarcinoma in primary sclerosing cholangitis: a systematic review and meta-analysis. Gastrointest. Endosc. 79, 783–789 (2014).
Barr Fritcher, E. G. et al. An optimized set of fluorescence in situ hybridization probes for detection of pancreatobiliary tract cancer in cytology brush samples. Gastroenterology 149, 1813–1824.e1 (2015). Fluorescence in situ hybridization has become an essential tool in cholangiocarcinoma diagnosis.
Rizvi, S., Eaton, J., Yang, J. D., Chandrasekhara, V. & Gores, G. J. Emerging technologies for the diagnosis of perihilar cholangiocarcinoma. Semin. Liver Dis. 38, 160–169 (2018).
Mohamadnejad, M. et al. Role of EUS for preoperative evaluation of cholangiocarcinoma: a large single-center experience. Gastrointest. Endosc. 73, 71–78 (2011).
Heimbach, J. K., Sanchez, W., Rosen, C. B. & Gores, G. J. Trans-peritoneal fine needle aspiration biopsy of hilar cholangiocarcinoma is associated with disease dissemination. HPB 13, 356–360 (2011).
Lim, J. H. Liver flukes: the malady neglected. Korean J. Radiol. 12, 269–279 (2011).
Khuntikeo, N. et al. The socioeconomic burden of cholangiocarcinoma associated with Opisthorchis viverrini sensu lato infection in northeast Thailand: a preliminary analysis. Adv. Parasitol. 102, 141–163 (2018).
Saijuntha, W. et al. Recent advances in the diagnosis and detection of Opisthorchis viverrini sensu lato in human and intermediate hosts for use in control and elimination programs. Adv. Parasitol. 101, 177–214 (2018).
Sadaow, L. et al. Development of an immunochromatographic point-of-care test for serodiagnosis of opisthorchiasis and clonorchiasis. Am. J. Trop. Med. Hyg. 101, 1156–1160 (2019).
Sayasone, S. et al. Efficacy and safety of tribendimidine versus praziquantel against Opisthorchis viverrini in Laos: an open-label, randomised, non-inferiority, phase 2 trial. Lancet Infect. Dis. 18, 155–161 (2018).
Sripa, B., Tangkawattana, S. & Sangnikul, T. The Lawa model: a sustainable, integrated opisthorchiasis control program using the EcoHealth approach in the Lawa Lake region of Thailand. Parasitol. Int. 66, 346–354 (2017).
Phimpraphai, W., Tangkawattana, S., Kasemsuwan, S. & Sripa, B. Social influence in liver fluke transmission: application of social network analysis of food sharing in Thai Isaan culture. Adv. Parasitol. 101, 97–124 (2018).
Tang, Z. L., Huang, Y. & Yu, X. B. Current status and perspectives of Clonorchis sinensis and clonorchiasis: epidemiology, pathogenesis, omics, prevention and control. Infect. Dis. Poverty 5, 71 (2016).
Shin, H. R. et al. Descriptive epidemiology of cholangiocarcinoma and clonorchiasis in Korea. J. Korean Med. Sci. 25, 1011–1016 (2010).
Tangkawattana, S. & Sripa, B. Integrative EcoHealth/One Health approach for sustainable liver fluke control: the Lawa model. Adv. Parasitol. 102, 115–139 (2018).
Mairiang, E. et al. Ultrasonography assessment of hepatobiliary abnormalities in 3359 subjects with Opisthorchis viverrini infection in endemic areas of Thailand. Parasitol. Int. 61, 208–211 (2012).
Khuntikeo, N. et al. Cohort profile: cholangiocarcinoma screening and care program (CASCAP). BMC Cancer 15, 459 (2015).
Khuntikeo, N. et al. A comparison of the proportion of early stage cholangiocarcinoma found in an ultrasound-screening program compared to walk-in patients. HPB 22, 874–883 (2020).
Chamadol, N. et al. Histological confirmation of periductal fibrosis from ultrasound diagnosis in cholangiocarcinoma patients. J. Hepatobiliary Pancreat. Sci. 21, 316–322 (2014).
Khuntikeo, N., Loilome, W., Thinkhamrop, B., Chamadol, N. & Yongvanit, P. A comprehensive public health conceptual framework and strategy to effectively combat cholangiocarcinoma in Thailand. PLoS Negl. Trop. Dis. 10, e0004293 (2016).
Chamadol, N. et al. Teleconsultation ultrasonography: a new weapon to combat cholangiocarcinoma. ESMO Open 2, e000231 (2017).
Weismuller, T. J. et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology 152, 1975–1984.e8 (2017).
Rizvi, S., Eaton, J. E. & Gores, G. J. Primary sclerosing cholangitis as a premalignant biliary tract disease: surveillance and management. Clin. Gastroenterol. Hepatol. 13, 2152–2165 (2015).
Darwish Murad, S. et al. Efficacy of neoadjuvant chemoradiation, followed by liver transplantation, for perihilar cholangiocarcinoma at 12 US centers. Gastroenterology 143, 88–98 e83 quiz e14 (2012). This multicentre study established neoadjuvant chemoradiation plus liver transplantation as an effective option for perihilar cholangiocarcinoma.
Eaton, J. E. et al. Early cholangiocarcinoma detection with magnetic resonance imaging versus ultrasound in primary sclerosing cholangitis. Hepatology 73, 1868–1881 (2021).
Chapman, R. et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology 51, 660–678 (2010).
Doussot, A. et al. Outcomes after resection of intrahepatic cholangiocarcinoma: external validation and comparison of prognostic models. J. Am. Coll. Surg. 221, 452–461 (2015).
Weber, S. M. et al. Intrahepatic cholangiocarcinoma: expert consensus statement. HPB 17, 669–680 (2015).
Weber, S. M. et al. Intrahepatic cholangiocarcinoma: resectability, recurrence pattern, and outcomes. J. Am. Coll. Surg. 193, 384–391 (2001).
Spolverato, G. et al. The impact of surgical margin status on long-term outcome after resection for intrahepatic cholangiocarcinoma. Ann. Surg. Oncol. 22, 4020–4028 (2015).
Buettner, S. et al. Survival after resection of multiple tumor foci of intrahepatic cholangiocarcinoma. J. Gastrointest. Surg. 23, 2239–2246 (2019).
Lamarca, A. et al. Liver metastases of intrahepatic cholangiocarcinoma: implications for an updated staging system. Hepatology 73, 2311–2325 (2021).
Kim, Y. et al. Surgical management of intrahepatic cholangiocarcinoma: defining an optimal prognostic lymph node stratification schema. Ann. Surg. Oncol. 22, 2772–2778 (2015).
Kizy, S. et al. Surgical resection of lymph node positive intrahepatic cholangiocarcinoma may not improve survival. HPB 21, 235–241 (2019).
Sapisochin, G., de Sevilla, E. F., Echeverri, J. & Charco, R. Management of “very early” hepatocellular carcinoma on cirrhotic patients. World J. Hepatol. 6, 766–775 (2014).
Sapisochin, G. et al. Liver transplantation for “very early” intrahepatic cholangiocarcinoma: international retrospective study supporting a prospective assessment. Hepatology 64, 1178–1188 (2016).
Lunsford, K. E. et al. Liver transplantation for locally advanced intrahepatic cholangiocarcinoma treated with neoadjuvant therapy: a prospective case-series. Lancet Gastroenterol. Hepatol. 3, 337–348 (2018).
Hyder, O. et al. Intra-arterial therapy for advanced intrahepatic cholangiocarcinoma: a multi-institutional analysis. Ann. Surg. Oncol. 20, 3779–3786 (2013).
Cercek, A. et al. Assessment of hepatic arterial infusion of floxuridine in combination with systemic gemcitabine and oxaliplatin in patients with unresectable intrahepatic cholangiocarcinoma: a phase 2 clinical trial. JAMA Oncol. 6, 60–67 (2020).
Hong, T. S. et al. Multi-institutional phase II study of high-dose hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J. Clin. Oncol. 34, 460–468 (2016).
Bird, N. et al. Role of staging laparoscopy in the stratification of patients with perihilar cholangiocarcinoma. Br. J. Surg. 104, 418–425 (2017).
Nuzzo, G. et al. Improvement in perioperative and long-term outcome after surgical treatment of hilar cholangiocarcinoma: results of an Italian multicenter analysis of 440 patients. Arch. Surg. 147, 26–34 (2012).
Nagino, M. et al. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann. Surg. 258, 129–140 (2013).
Abbas, S. & Sandroussi, C. Systematic review and meta-analysis of the role of vascular resection in the treatment of hilar cholangiocarcinoma. HPB 15, 492–503 (2013).
de Jong, M. C. et al. The impact of portal vein resection on outcomes for hilar cholangiocarcinoma: a multi-institutional analysis of 305 cases. Cancer 118, 4737–4747 (2012).
Ebata, T. et al. Surgical resection for Bismuth type IV perihilar cholangiocarcinoma. Br. J. Surg. 105, 829–838 (2018).
van Vugt, J. L. A. et al. The prognostic value of portal vein and hepatic artery involvement in patients with perihilar cholangiocarcinoma. HPB 20, 83–92 (2018).
Dickson, P. V. & Behrman, S. W. Distal cholangiocarcinoma. Surg. Clin. North. Am. 94, 325–342 (2014).
Rea, D. J. et al. Liver transplantation with neoadjuvant chemoradiation is more effective than resection for hilar cholangiocarcinoma. Ann. Surg. 242, 451–458 (2005). discussion 458-461.
Sudan, D. et al. Radiochemotherapy and transplantation allow long-term survival for nonresectable hilar cholangiocarcinoma. Am. J. Transpl. 2, 774–779 (2002).
Darwish Murad, S. et al. Predictors of pretransplant dropout and posttransplant recurrence in patients with perihilar cholangiocarcinoma. Hepatology 56, 972–981 (2012).
Valle, J. et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N. Engl. J. Med. 362, 1273–1281 (2010). This study established gemcitabine and cisplatin as the first-line systemic therapy for cholangiocarcinoma.
Lamarca, A. et al. Second-line FOLFOX chemotherapy versus active symptom control for advanced biliary tract cancer (ABC-06): a phase 3, open-label, randomised, controlled trial. Lancet Oncol. 22, 690–701 (2021).
Morizane, C. et al. Combination gemcitabine plus S-1 versus gemcitabine plus cisplatin for advanced/recurrent biliary tract cancer: the FUGA-BT (JCOG1113) randomized phase III clinical trial. Ann. Oncol. 30, 1950–1958 (2019).
Phelip, J. M. et al. Modified FOLFIRINOX versus CISGEM as first-line chemotherapy for advanced biliary tract cancer: results of AMEBICA PRODIGE 38 randomized phase II trial [abstract 52P]. Ann. Oncol. 31, S260–S261 (2020).
Shroff, R. T. et al. Gemcitabine, cisplatin, and nab-paclitaxel for the treatment of advanced biliary tract cancers: a phase 2 clinical trial. JAMA Oncol. 5, 824–830 (2019).
Lamarca, A. et al. Advanced intrahepatic cholangiocarcinoma: post hoc analysis of the ABC-01, -02, and -03 clinical trials. J. Natl Cancer Inst. 112, 200–210 (2020).
Abou-Alfa, G. K. et al. Ivosidenib in IDH1-mutant, chemotherapy-refractory cholangiocarcinoma (ClarIDHy): a multicentre, randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 21, 796–807 (2020).
Abou-Alfa, G. K. et al. Pemigatinib for previously treated, locally advanced or metastatic cholangiocarcinoma: a multicentre, open-label, phase 2 study. Lancet Oncol. 21, 671–684 (2020). Pemigatinib was the first targeted therapy to receive FDA approval in cholangiocarcinoma.
Javle, M. et al. Phase II study of BGJ398 in patients with FGFR-altered advanced cholangiocarcinoma. J. Clin. Oncol. 36, 276–282 (2018).
Rizvi, S. & Gores, G. J. Emerging molecular therapeutic targets for cholangiocarcinoma. J. Hepatol. 67, 632–644 (2017).
Goeppert, B. et al. BRAF V600E-specific immunohistochemistry reveals low mutation rates in biliary tract cancer and restriction to intrahepatic cholangiocarcinoma. Mod. Pathol. 27, 1028–1034 (2014).
Javle, M. et al. Biliary cancer: utility of next-generation sequencing for clinical management. Cancer 122, 3838–3847 (2016).
Subbiah, V. et al. Dabrafenib plus trametinib in patients with BRAF(V600E)-mutated biliary tract cancer (ROAR): a phase 2, open-label, single-arm, multicentre basket trial. Lancet Oncol. 21, 1234–1243 (2020).
Piha-Paul, S. A. et al. Efficacy and safety of pembrolizumab for the treatment of advanced biliary cancer: results from the KEYNOTE-158 and KEYNOTE-028 studies. Int. J. Cancer 147, 2190–2198 (2020).
Asaoka, Y., Ijichi, H. & Koike, K. PD-1 blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 373, 1979 (2015).
Kim, R. D. et al. A phase 2 multi-institutional study of nivolumab for patients with advanced refractory biliary tract cancer. JAMA Oncol. 6, 888–894 (2020).
Klein, O. et al. Evaluation of combination nivolumab and ipilimumab immunotherapy in patients with advanced biliary tract cancers: subgroup analysis of a phase 2 nonrandomized clinical trial. JAMA Oncol. 6, 1405–1409 (2020).
Finn, R. S. et al. KEYNOTE-966: A randomized, double-blind, placebo-controlled, phase 3 study of pembrolizumab in combination with gemcitabine and cisplatin for the treatment of advanced biliary tract carcinoma [abstract CT283]. Cancer Res. 80 (Suppl. 16), CT283 (2020).
Nathan, H. et al. Trends in survival after surgery for cholangiocarcinoma: a 30-year population-based SEER database analysis. J. Gastrointest. Surg. 11, 1488–1496; discussion 1496–1487 (2007).
Wang, Y. et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J. Clin. Oncol. 31, 1188–1195 (2013).
Edeline, J. et al. Gemcitabine and oxaliplatin chemotherapy or surveillance in resected biliary tract cancer (PRODIGE 12-ACCORD 18-UNICANCER GI): a randomized phase III study. J. Clin. Oncol. 37, 658–667 (2019).
Ebata, T. et al. Randomized clinical trial of adjuvant gemcitabine chemotherapy versus observation in resected bile duct cancer. Br. J. Surg. 105, 192–202 (2018).
Primrose, J. N. et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 20, 663–673 (2019).
Shroff, R. T. et al. Adjuvant therapy for resected biliary tract cancer: ASCO clinical practice guideline. J. Clin. Oncol. 37, 1015–1027 (2019).
Fitzmaurice, C., Seiler, C. M., Buchler, M. W. & Diener, M. K. Survival, mortality and quality of life after pylorus-preserving or classical Whipple operation. A systematic review with meta-analysis. Chirurg 81, 454–471 (2010).
Dasgupta, D. et al. Quality of life after liver resection for hepatobiliary malignancies. Br. J. Surg. 95, 845–854 (2008).
Loeuillard, E., Fischbach, S. R., Gores, G. J. & Rizvi, S. Animal models of cholangiocarcinoma. Biochim. Biophys. Acta Mol. Basis Dis. 1865, 982–992 (2019).
Lavu, S. et al. Effect of statins on the risk of extrahepatic cholangiocarcinoma. Hepatology 72, 1298–1309 (2020).
Fabris, L., Cadamuro, M., Cagnin, S., Strazzabosco, M. & Gores, G. J. Liver matrix in benign and malignant biliary tract disease. Semin. Liver Dis. 40, 282–297 (2020).
Abou-Alfa, G. K., Pandya, S. S. & Zhu, A. X. Ivosidenib for advanced IDH1-mutant cholangiocarcinoma – Authors’ reply. Lancet Oncol. 21, e371 (2020).
Lamarca, A. et al. Molecular profiling in daily clinical practice: practicalities in advanced cholangiocarcinoma and other biliary tract cancers. J. Clin. Med. 9, 2854 (2020).
Smout, M. J. et al. Infection with the carcinogenic human liver fluke, Opisthorchis viverrini. Mol. BioSyst. 7, 1367–1375 (2011).
Sirica, A. E., Strazzabosco, M. & Cadamuro, M. Intrahepatic cholangiocarcinoma: morpho-molecular pathology, tumor reactive microenvironment, and malignant progression. Adv. Cancer Res. 149, 321–387 (2021).
Chuchuen, O. et al. Rapid label-free analysis of Opisthorchis viverrini eggs in fecal specimens using confocal Raman spectroscopy. PLoS ONE 14, e0226762 (2019).
Suwannatrai, A., Saichua, P. & Haswell, M. Epidemiology of Opisthorchis viverrini infection. Adv. Parasitol. 101, 41–67 (2018).
Diemert, D. J., Bottazzi, M. E., Plieskatt, J., Hotez, P. J. & Bethony, J. M. Lessons along the critical path: developing vaccines against human helminths. Trends Parasitol. 34, 747–758 (2018).
McManus, D. P. Recent progress in the development of liver fluke and blood fluke vaccines. Vaccines (Basel) 8, 553 (2020).
Sun, H. et al. Bacillus subtilis spore with surface display of paramyosin from Clonorchis sinensis potentializes a promising oral vaccine candidate. Parasit. Vectors 11, 156 (2018).
Wang, X. et al. Surface display of Clonorchis sinensis enolase on Bacillus subtilis spores potentializes an oral vaccine candidate. Vaccine 32, 1338–1345 (2014).
Mekonnen, G. G., Pearson, M., Loukas, A. & Sotillo, J. Extracellular vesicles from parasitic helminths and their potential utility as vaccines. Expert Rev. Vaccines 17, 197–205 (2018).
Phumrattanaprapin, W. et al. Orally administered Bacillus spores expressing an extracellular vesicle-derived tetraspanin protect hamsters against challenge infection with carcinogenic human liver fluke. J. Infect. Dis. 223, 1445–1455 (2021).
Acknowledgements
G.J.G. is supported by the SPORE grant CA210964. P.J.B. and A.L. receive grant support (R01CA164719) from the National Institute of Health. S.A.K. is grateful for support from the UK National Institute for Health Research (NIHR) Biomedical Facilities at Imperial College London. B.T.T. receives support from The National Medical Research Council (grant MOH-000248). S.I.I. receives support from the National Cancer Institute (1K08CA236874) and the Mayo Foundation. A.L. receives support from National Health and Medical Research Council Senior Principal Research Fellowship 1117504. S.W. receives support from National Science and Technology Development Agency (NSTDA), Thailand, and the e-ASIA JRP.
Author information
Authors and Affiliations
Contributions
Introduction (G.J.G.); Epidemiology (P.J.B. and S.A.K.); Mechanisms/pathophysiology (B.T.T., A.L., S.W. and A.E.S.); Diagnosis, screening and prevention (S.I.I., P.J.B. and G.J.G.); Management (S.I.I.); Quality of life (M.B.); Outlook (G.J.G.); Overview of Primer (G.J.G.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks B. Koerkamp; D.-Y. Oh, who co-reviewed with J. Yoon; R. T. Shroff, who co-reviewed with M. Savani; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brindley, P.J., Bachini, M., Ilyas, S.I. et al. Cholangiocarcinoma. Nat Rev Dis Primers 7, 65 (2021). https://doi.org/10.1038/s41572-021-00300-2
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-021-00300-2
This article is cited by
-
Integrative single-cell and machine-learning analysis identifies ac4C-related S100A13 as a causal risk gene in cholangiocarcinoma
BMC Cancer (2026)
-
A subcellular spatial atlas illuminates the microenvironmental remodeling of perineural invasion in distal cholangiocarcinoma
Journal of Hematology & Oncology (2026)
-
SLC25A11-mediated reprogramming of mitochondrial redox state and lipid peroxidation confers NRF2-dependent ferroptosis resistance in biliary tract cancer
Cellular & Molecular Biology Letters (2026)
-
Cholangiocarcinoma derived exosomes attenuate the anti-tumor functions of NK cells
Scientific Reports (2026)
-
Identification of serum peptide biomarkers for cholangiocarcinoma diagnosis and staging via MALDI-TOF MS and LC-MS/MS
British Journal of Cancer (2026)