Abstract
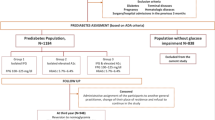
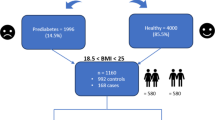
Prediabetes or intermediate hyperglycaemia represents a preliminary stage in the development of type 2 diabetes mellitus (T2DM). In addition to an increased likelihood of developing T2DM, individuals with prediabetes have an elevated risk of various vascular and non-vascular complications. No consensus has been achieved on the ideal screening strategy for prediabetes, with fasting plasma glucose concentration, glycated haemoglobin (HbA1c) and the oral glucose tolerance test being the most frequently measured parameters. The two major phenotypes of prediabetes, that is, impaired fasting glucose and impaired glucose tolerance, may represent different pathophysiologies with varying natural history, risk of adverse outcomes and responsiveness to treatment. Most of the evidence for managing prediabetes focuses on lifestyle modification with or without medications in individuals with overweight or obesity and impaired glucose tolerance. Whether these interventions are beneficial in individuals with impaired fasting glucose and those of normal body weight is unclear, as is the cost-effectiveness and sustainability of pharmacotherapy for treating prediabetes. Large-scale national T2DM prevention programmes are currently under way to assess whether the benefits of interventions for prediabetes can be translated to the community setting.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Rao Kondapally Seshasai, S. et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 364, 829–841 (2011).
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of care in diabetes-2025. Diabetes Care 48, S27–S49 (2025).
International Federation of Clinical Chemistry and Laboratory Medicine, IFCC Scientific Division, Nordin, G. & Dybkaer, R. Recommendation for term and measurement unit for ‘HbA1c’. Clin. Chem. Lab. Med. 45, 1081–1082 (2007).
IDF Diabetes Atlas 2025. Diabetes Atlas https://diabetesatlas.org/resources/idf-diabetes-atlas-2025/ (2025).
Rooney, M. R. et al. Global prevalence of prediabetes. Diabetes Care 46, 1388–1394 (2023).
Abdul-Ghani, M. A., Tripathy, D. & DeFronzo, R. A. Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care 29, 1130–1139 (2006).
NCD Risk Factor Collaboration (NCD-RisC). Global variation in diabetes diagnosis and prevalence based on fasting glucose and hemoglobin A1c. Nat. Med. 29, 2885–2901 (2023).
Nicolaisen, S. K., Pedersen, L., Witte, D. R., Sørensen, H. T. & Thomsen, R. W. HbA1c-defined prediabetes and progression to type 2 diabetes in Denmark: a population-based study based on routine clinical care laboratory data. Diabetes Res. Clin. Pract. 203, 110829 (2023).
Liu, J. et al. Trends and disparities in diabetes and prediabetes among adults in the United States, 1999-2018. Public Health 214, 163–170 (2023).
Richter, B., Hemmingsen, B., Metzendorf, M.-I. & Takwoingi, Y. Development of type 2 diabetes mellitus in people with intermediate hyperglycaemia. Cochrane Database Syst. Rev. 10, CD012661 (2018).
The Lancet Diabetes Endocrinology. Prediabetes: much more than just a risk factor. Lancet Diabetes Endocrinol. 13, 165 (2025).
Hostalek, U. Global epidemiology of prediabetes — present and future perspectives. Clin. Diabetes Endocrinol. 5, 5 (2019).
Zeyad, M., Saudi, L., Maraqa, B., Musmar, B. & Nazzal, Z. Prevalence of prediabetes and associated risk factors in the Eastern Mediterranean Region: a systematic review. BMC Public Health 25, 1382 (2025).
Muscogiuri, G. et al. Current evidence on gender-related risk factors for type 1 diabetes, type 2 diabetes and prediabetes: a reappraisal of the Italian study group on gender difference in endocrine diseases. J. Endocrinol. Invest. 48, 573–585 (2025).
Siddiqui, S., Zainal, H., Harun, S. N., Sheikh Ghadzi, S. M. & Ghafoor, S. Gender differences in the modifiable risk factors associated with the presence of prediabetes: a systematic review. Diabetes Metab. Syndr. 14, 1243–1252 (2020).
Schlesinger, S. et al. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies. Diabetologia 65, 275–285 (2022).
Ndumele, C. E. et al. Cardiovascular-kidney-metabolic health: a presidential advisory from the American Heart Association. Circulation 148, 1606–1635 (2023).
Roden, M. & Shulman, G. I. The integrative biology of type 2 diabetes. Nature 576, 51–60 (2019).
Weyer, C., Bogardus, C., Mott, D. M. & Pratley, R. E. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J. Clin. Invest. 104, 787–794 (1999).
DeFronzo, R. A. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58, 773 (2009).
Hammoud, R. & Drucker, D. J. Beyond the pancreas: contrasting cardiometabolic actions of GIP and GLP1. Nat. Rev. Endocrinol. 19, 201–216 (2023).
Mitrakou, A. et al. Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. N. Engl. J. Med. 326, 22–29 (1992).
Mastrototaro, L. & Roden, M. Insulin resistance and insulin sensitizing agents. Metabolism 125, 154892 (2021).
Petersen, M. C. & Shulman, G. I. Mechanisms of insulin action and insulin resistance. Physiol. Rev. 98, 2133–2223 (2018).
Scherer, P. E. The many secret lives of adipocytes: implications for diabetes. Diabetologia 62, 223–232 (2019).
Xourafa, G., Korbmacher, M. & Roden, M. Inter-organ crosstalk during development and progression of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 20, 27–49 (2024).
Barnett, A. H., Eff, C., Leslie, R. D. & Pyke, D. A. Diabetes in identical twins. A study of 200 pairs. Diabetologia 20, 87–93 (1981).
Fuchsberger, C. et al. The genetic architecture of type 2 diabetes. Nature 536, 41–47 (2016).
Spracklen, C. N. et al. Identification of type 2 diabetes loci in 433,540 East Asian individuals. Nature 582, 240–245 (2020).
Mahajan, A. et al. Refining the accuracy of validated target identification through coding variant fine-mapping in type 2 diabetes. Nat. Genet. 50, 559–571 (2018).
Suzuki, K. et al. Genetic drivers of heterogeneity in type 2 diabetes pathophysiology. Nature 627, 347–357 (2024).
Barrès, R. & Zierath, J. R. The role of diet and exercise in the transgenerational epigenetic landscape of T2DM. Nat. Rev. Endocrinol. 12, 441–451 (2016).
McCarthy, M. & Birney, E. Personalized profiles for disease risk must capture all facets of health. Nature 597, 175–177 (2021).
Wahl, S. et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 541, 81–86 (2017).
Chan, J. C. N. et al. The Lancet Commission on Diabetes: using data to transform diabetes care and patient lives. Lancet 396, 2019–2082 (2021).
Takeuchi, T. et al. Gut microbial carbohydrate metabolism contributes to insulin resistance. Nature 621, 389 (2023).
Sandforth, A. et al. Mechanisms of weight loss-induced remission in people with prediabetes: a post-hoc analysis of the randomised, controlled, multicentre prediabetes lifestyle intervention study (PLIS). Lancet Diabetes Endocrinol. 11, 798–810 (2023).
Tabák, A. G. et al. Adiponectin trajectories before type 2 diabetes diagnosis: Whitehall II study. Diabetes Care 35, 2540 (2012).
Targher, G., Corey, K. E., Byrne, C. D. & Roden, M. The complex link between NAFLD and type 2 diabetes mellitus — mechanisms and treatments. Nat. Rev. Gastroenterol. Hepatol. 18, 599–612 (2021).
Fromenty, B. & Roden, M. Mitochondrial alterations in fatty liver diseases. J. Hepatol. 78, 415–429 (2023).
Chan, K. E. et al. Longitudinal outcomes associated with metabolic dysfunction-associated steatotic liver disease: a meta-analysis of 129 studies. Clin. Gastroenterol. Hepatol. 22, 488–498.e14 (2024).
Tabák, A. G., Herder, C., Rathmann, W., Brunner, E. J. & Kivimäki, M. Prediabetes: a high-risk state for diabetes development. Lancet 379, 2279–2290 (2012).
Kahn, S. E. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia 46, 3–19 (2003).
Tabák, A. G. et al. Trajectories of glycemia, insulin sensitivity and insulin secretion preceding the diagnosis of type 2 diabetes: the Whitehall II study. Lancet 373, 2215 (2009).
Ferrannini, E. et al. Mode of onset of type 2 diabetes from normal or impaired glucose tolerance. Diabetes 53, 160–165 (2004).
Mason, C. C., Hanson, R. L. & Knowler, W. C. Progression to type 2 diabetes characterized by moderate then rapid glucose increases. Diabetes 56, 2054–2061 (2007).
Sattar, N. et al. Serial metabolic measurements and conversion to type 2 diabetes in the west of Scotland coronary prevention study: specific elevations in alanine aminotransferase and triglycerides suggest hepatic fat accumulation as a potential contributing factor. Diabetes 56, 984–991 (2007).
Hulman, A. et al. Trajectories of glycaemia, insulin sensitivity and insulin secretion in South Asian and white individuals before diagnosis of type 2 diabetes: a longitudinal analysis from the Whitehall II cohort study. Diabetologia 60, 1252 (2017).
Weir, G. C. & Bonner-Weir, S. Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes 53, S16–S21 (2004).
Esser, N., Utzschneider, K. M. & Kahn, S. E. Early beta cell dysfunction vs insulin hypersecretion as the primary event in the pathogenesis of dysglycaemia. Diabetologia 63, 2007–2021 (2020).
Reaven, G. M. Insulin secretion and insulin action in non-insulin-dependent diabetes mellitus: which defect is primary? Diabetes Care 7, 17–24 (1984).
Wagner, R. et al. Pathophysiology-based subphenotyping of individuals at elevated risk for type 2 diabetes. Nat. Med. 27, 49–57 (2021).
Ahlqvist, E. et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 6, 361–369 (2018).
Zaharia, O. P. et al. Risk of diabetes-associated diseases in subgroups of patients with recent-onset diabetes: a 5-year follow-up study. Lancet Diabetes Endocrinol. 7, 684–694 (2019).
Cowie, C. C. et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: national health and nutrition examination survey 1999-2002. Diabetes Care 29, 1263–1268 (2006).
Guerrero, R., Vega, G. L., Grundy, S. M. & Browning, J. D. Ethnic differences in hepatic steatosis: an insulin resistance paradox? Hepatology 49, 791–801 (2009).
Chung, S. T. et al. Gluconeogenesis and risk for fasting hyperglycemia in Black and White women. JCI Insight 3, e121495 (2018).
Edwards, C. M. & Cusi, K. Prediabetes: a worldwide epidemic. Endocrinol. Metab. Clin. North Am. 45, 751–764 (2016).
Ramzy, A. & Kieffer, T. J. Altered islet prohormone processing: a cause or consequence of diabetes? Physiol. Rev. 102, 155–208 (2022).
Robertson, R. P. et al. Arginine is preferred to glucagon for stimulation testing of β-cell function. Am. J. Physiol. Endocrinol. Metab. 307, E720–E727 (2014).
Nauck, M. A. & Müller, T. D. Incretin hormones and type 2 diabetes. Diabetologia 66, 1780–1795 (2023).
Kanat, M. et al. Distinct β-cell defects in impaired fasting glucose and impaired glucose tolerance. Diabetes 61, 447–453 (2012).
Kowall, B. et al. Incidence rates of type 2 diabetes in people with impaired fasting glucose (ADA vs. WHO criteria) and impaired glucose tolerance: results from an older population (KORA S4/F4/FF4 study). Diabetes Care 42, e18–e20 (2019).
Tura, A. et al. Profiles of glucose metabolism in different prediabetes phenotypes, classified by fasting glycemia, 2-hour OGTT, glycated hemoglobin, and 1-hour OGTT: an IMI DIRECT study. Diabetes 70, 2092–2106 (2021).
Lagou, V. et al. Sex-dimorphic genetic effects and novel loci for fasting glucose and insulin variability. Nat. Commun. 12, 24 (2021).
Prystupa, K. et al. Clusters of prediabetes and type 2 diabetes stratify all-cause mortality in a cohort of participants undergoing invasive coronary diagnostics. Cardiovasc. Diabetol. 22, 211 (2023).
Huemer, M.-T. et al. Phenotype-based clusters, inflammation and cardiometabolic complications in older people before the diagnosis of type 2 diabetes: KORA F4/FF4 cohort study. Cardiovasc. Diabetol. 24, 83 (2025).
Zheng, R. et al. Data-driven subgroups of prediabetes and the associations with outcomes in Chinese adults. Cell Rep. Med. 4, 100958 (2023).
Anjana, R. M. et al. Novel subgroups of type 2 diabetes and their association with microvascular outcomes in an Asian Indian population: a data-driven cluster analysis: the INSPIRED study. BMJ Open Diabetes Res. Care 8, e001506 (2020).
Hodgson, S. et al. Integrating polygenic risk scores in the prediction of type 2 diabetes risk and subtypes in British Pakistanis and Bangladeshis: a population-based cohort study. PLoS Med. 19, e1003981 (2022).
Ke, C., Narayan, K. M. V., Chan, J. C. N., Jha, P. & Shah, B. R. Pathophysiology, phenotypes and management of type 2 diabetes mellitus in Indian and Chinese populations. Nat. Rev. Endocrinol. 18, 413–432 (2022).
Prasad, R. B. et al. Subgroups of patients with young-onset type 2 diabetes in India reveal insulin deficiency as a major driver. Diabetologia 65, 65–78 (2022).
Yajnik, C. S. et al. Polygenic scores of diabetes-related traits in subgroups of type 2 diabetes in India: a cohort study. Lancet Reg. Health Southeast Asia 14, 100182 (2023).
Kirthi, V. et al. Prevalence of peripheral neuropathy in pre-diabetes: a systematic review. BMJ Open Diabetes Res. Care 9, e002040 (2021).
Eleftheriadou, A. et al. The prevalence of cardiac autonomic neuropathy in prediabetes: a systematic review. Diabetologia 64, 288–303 (2021).
Jin, J. & Lu, P. Association between prediabetes and retinopathy: a meta-analysis. Horm. Metab. Res. 53, 801–809 (2021).
Rinella, M. E. et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology 78, 1966–1986 (2023).
Kahl, S. et al. Dysglycemia and liver lipid content determine the relationship of insulin resistance with hepatic OXPHOS capacity in obesity. J. Hepatol. 82, 417–426 (2025).
Yilmaz, Y., Senates, E., Yesil, A., Ergelen, R. & Colak, Y. Not only type 2 diabetes but also prediabetes is associated with portal inflammation and fibrosis in patients with non-alcoholic fatty liver disease. J. Diabetes Complicat. 28, 328–331 (2014).
Færch, K. et al. Trajectories of cardiometabolic risk factors before diagnosis of three subtypes of type 2 diabetes: a post-hoc analysis of the longitudinal Whitehall II cohort study. Lancet Diabetes Endocrinol. 1, 43–51 (2013).
Echouffo-Tcheugui, J. B., Narayan, K. M., Weisman, D., Golden, S. H. & Jaar, B. G. Association between prediabetes and risk of chronic kidney disease: a systematic review and meta-analysis. Diabet. Med. 33, 1615–1624 (2016).
Herder, C., Roden, M. & Ziegler, D. Novel insights into sensorimotor and cardiovascular autonomic neuropathy from recent-onset diabetes and population-based cohorts. Trends Endocrinol. Metab. 30, 286–298 (2019).
Bönhof, G. J. et al. Emerging biomarkers, tools, and treatments for diabetic polyneuropathy. Endocr. Rev. 40, 153–192 (2019).
Eid, S. A. et al. New perspectives in diabetic neuropathy. Neuron 111, 2623–2641 (2023).
Sune, M. P., Sune, M., Sune, P. & Dhok, A. Prevalence of retinopathy in prediabetic populations: a systematic review and meta-analysis. Cureus 15, e49602 (2023).
Bergman, M. et al. Pitfalls of HbA1c in the diagnosis of diabetes. J. Clin. Endocrinol. Metab. 105, 2803–2811 (2020).
Little, R. R. & Roberts, W. L. A review of variant hemoglobins interfering with hemoglobin A1c measurement. J. Diabetes Sci. Technol. 3, 446–451 (2009).
Leong, A. et al. Association of G6PD variants with hemoglobin A1c and impact on diabetes diagnosis in East Asian individuals. BMJ Open Diabetes Res. Care 8, e001091 (2020).
Cavagnolli, G., Pimentel, A. L., Freitas, P. A. C., Gross, J. L. & Camargo, J. L. Effect of ethnicity on HbA1c levels in individuals without diabetes: systematic review and meta-analysis. PLoS ONE 12, e0171315 (2017).
Chivese, T. et al. The diagnostic accuracy of HbA1c, compared to the oral glucose tolerance test, for screening for type 2 diabetes mellitus in Africa — a systematic review and meta-analysis. Diabet. Med. 39, e14754 (2022).
Briker, S. M. et al. A1C underperforms as a diagnostic test in Africans even in the absence of nutritional deficiencies, anemia and hemoglobinopathies: insight from the Africans in America study. Front. Endocrinol. 10, 533 (2019).
Echouffo-Tcheugui, J. B. & Selvin, E. Prediabetes and what it means: the epidemiological evidence. Annu. Rev. Public Health 42, 59–77 (2021).
Salinero-Fort, M. A. et al. Glycemic variability and all-cause mortality in a large prospective southern European cohort of patients with differences in glycemic status. PLoS ONE 17, e0271632 (2022).
Ma, C. et al. Association between glucose fluctuation during 2-hour oral glucose tolerance test, inflammation and oxidative stress markers, and β-cell function in a Chinese population with normal glucose tolerance. Ann. Transl. Med. 9, 327 (2021).
Duong, K. N. C. et al. Comparison of diagnostic accuracy for diabetes diagnosis: a systematic review and network meta-analysis. Front. Med. 10, 1016381 (2023).
Sathish, T. et al. Effect of conventional lifestyle interventions on type 2 diabetes incidence by glucose-defined prediabetes phenotype: an individual participant data meta-analysis of randomized controlled trials. Diabetes Care 46, 1903–1907 (2023).
Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the diabetes prevention program outcomes study. Lancet Diabetes Endocrinol. 3, 866–875 (2015).
Li, G. et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing diabetes prevention study: a 23-year follow-up study. Lancet Diabetes Endocrinol. 2, 474–480 (2014).
Ahuja, V. et al. Accuracy of 1-hour plasma glucose during the oral glucose tolerance test in diagnosis of type 2 diabetes in adults: a meta-analysis. Diabetes Care 44, 1062–1069 (2021).
Bergman, M. et al. Current diagnostic criteria identify risk for type 2 diabetes too late. Lancet Diabetes Endocrinol. 11, 224–226 (2023).
Ha, J. et al. One-hour glucose is an earlier marker of dysglycemia than two-hour glucose. Diabetes Res. Clin. Pract. 203, 110839 (2023).
Bergman, M. et al. International diabetes federation position statement on the 1-hour post-load plasma glucose for the diagnosis of intermediate hyperglycaemia and type 2 diabetes. Diabetes Res. Clin. Pract. 209, 111589 (2024).
Ko, G. T. et al. The reproducibility and usefulness of the oral glucose tolerance test in screening for diabetes and other cardiovascular risk factors. Ann. Clin. Biochem. 35, 62–67 (1998).
Gerich, J. E. Metabolic abnormalities in impaired glucose tolerance. Metabolism 46, 40–43 (1997).
Coetzee, A. et al. A comparison between point-of-care testing and venous glucose determination for the diagnosis of diabetes mellitus 6-12 weeks after gestational diabetes. Diabet. Med. 36, 591–599 (2019).
Freitas, P. A. C., Ehlert, L. R. & Camargo, J. L. Glycated albumin: a potential biomarker in diabetes. Arch. Endocrinol. Metab. 61, 296–304 (2017).
Chan, J. C., Yeung, V. T., Cheung, C. K., Swaminathan, R. & Cockram, C. S. The inter-relationships between albuminuria, plasma albumin concentration and indices of glycaemic control in non-insulin-dependent diabetes mellitus. Clin. Chim. Acta 210, 179–185 (1992).
Sumner, A. E. et al. A1C combined with glycated albumin improves detection of prediabetes in Africans: the Africans in America study. Diabetes Care 39, 271–277 (2016).
Lindström, J. & Tuomilehto, J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 26, 725–731 (2003).
Mohan, V., Deepa, R., Deepa, M., Somannavar, S. & Datta, M. A simplified Indian diabetes risk score for screening for undiagnosed diabetic subjects. J. Assoc. Physicians India 53, 759–763 (2005).
Lee, C. M. Y. et al. Comparing different definitions of prediabetes with subsequent risk of diabetes: an individual participant data meta-analysis involving 76 513 individuals and 8208 cases of incident diabetes. BMJ Open Diab. Res. Care 7, e000794 (2019).
Bell, K. et al. A position statement on screening and management of prediabetes in adults in primary care in Australia. Diabetes Res. Clin. Pract. 164, 108188 (2020).
Puavilai, G. et al. Random capillary plasma glucose measurement in the screening of diabetes mellitus in high-risk subjects in Thailand. Diabetes Res. Clin. Pract. 51, 125–131 (2001).
Rhee, M. K. et al. Random plasma glucose predicts the diagnosis of diabetes. PLoS ONE 14, e0219964 (2019).
Somannavar, S., Ganesan, A., Deepa, M., Datta, M. & Mohan, V. Random capillary blood glucose cut points for diabetes and pre-diabetes derived from community-based opportunistic screening in India. Diabetes Care 32, 641–643 (2009).
Susairaj, P. et al. Cut-off value of random blood glucose among Asian Indians for preliminary screening of persons with prediabetes and undetected type 2 diabetes defined by the glycosylated haemoglobin criteria. J. Diabetes Clin. Res. 1, 53–58 (2019).
Herman, W. H. & Ye, W. Precision prevention of diabetes. Diabetes Care 46, 1894–1896 (2023).
Bergman, M. et al. Staging schema for early diagnosis of prediabetes. Lancet Diabetes Endocrinol. 12, 873–876 (2024).
Knowler, W. C. et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 346, 393–403 (2002).
Pan, X. R. et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 20, 537–544 (1997).
Tuomilehto, J. et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 344, 1343–1350 (2001).
Rendell, M. Pharmacotherapeutic options for prediabetes. Expert Opin. Pharmacother. 22, 45–54 (2021).
Ramachandran, A. et al. The Indian diabetes prevention programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 49, 289–297 (2006).
Davies, M. J. et al. A community based primary prevention programme for type 2 diabetes integrating identification and lifestyle intervention for prevention: the let’s prevent diabetes cluster randomised controlled trial. Prev. Med. 84, 48–56 (2016).
Kosaka, K., Noda, M. & Kuzuya, T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res. Clin. Pract. 67, 152–162 (2005).
Lakka, T. A. et al. Real-world effectiveness of digital and group-based lifestyle interventions as compared with usual care to reduce type 2 diabetes risk — a stop diabetes pragmatic randomised trial. Lancet Reg. Health Eur. 24, 100527 (2023).
Ramachandran, A. et al. Pioglitazone does not enhance the effectiveness of lifestyle modification in preventing conversion of impaired glucose tolerance to diabetes in Asian Indians: results of the Indian diabetes prevention programme-2 (IDPP-2). Diabetologia 52, 1019–1026 (2009).
Saito, T. et al. Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels: a randomized controlled trial. Arch. Intern. Med. 171, 1352–1360 (2011).
Thankappan, K. R. et al. A peer-support lifestyle intervention for preventing type 2 diabetes in India: a cluster-randomized controlled trial of the Kerala diabetes prevention program. PLoS Med. 15, e1002575 (2018).
Weber, M. B. et al. The stepwise approach to diabetes prevention: results from the D-CLIP randomized controlled trial. Diabetes Care 39, 1760–1767 (2016).
Lindström, J. et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish diabetes prevention study. Lancet 368, 1673–1679 (2006).
Gong, Q. et al. Long-term effects of a randomised trial of a 6-year lifestyle intervention in impaired glucose tolerance on diabetes-related microvascular complications: the China Da Qing diabetes prevention outcome study. Diabetologia 54, 300–307 (2011).
Goldberg, R. B. et al. Effects of long-term metformin and lifestyle interventions on cardiovascular events in the diabetes prevention program and its outcome study. Circulation 145, 1632–1641 (2022).
Birkenfeld, A. L. & Mohan, V. Prediabetes remission for type 2 diabetes mellitus prevention. Nat. Rev. Endocrinol. 20, 441–442 (2024).
Buchanan, T. A. et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk Hispanic women. Diabetes 51, 2796–2803 (2002).
Chiasson, J.-L. et al. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet 359, 2072–2077 (2002).
DeFronzo, R. A. et al. Pioglitazone for diabetes prevention in impaired glucose tolerance. N. Engl. J. Med. 364, 1104–1115 (2011).
DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 368, 1096–1105 (2006).
DREAM Trial Investigators et al. Effect of ramipril on the incidence of diabetes. N. Engl. J. Med. 355, 1551–1562 (2006).
Gerstein, H. C. et al. Impact of acarbose on incident diabetes and regression to normoglycemia in people with coronary heart disease and impaired glucose tolerance: insights from the ACE trial. Diabetes Care 43, 2242–2247 (2020).
Jastreboff, A. M. et al. Tirzepatide for obesity treatment and diabetes prevention. N. Engl. J. Med. 392, 958–971 (2025).
Kawamori, R. et al. Voglibose for prevention of type 2 diabetes mellitus: a randomised, double-blind trial in Japanese individuals with impaired glucose tolerance. Lancet 373, 1607–1614 (2009).
Knowler, W. C. et al. Prevention of type 2 diabetes with troglitazone in the diabetes prevention program. Diabetes 54, 1150–1156 (2005).
le Roux, C. W. et al. 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. Lancet 389, 1399–1409 (2017).
NAVIGATOR Study Group et al. Effect of nateglinide on the incidence of diabetes and cardiovascular events. N. Engl. J. Med. 362, 1463–1476 (2010).
NAVIGATOR Study Group et al. Effect of valsartan on the incidence of diabetes and cardiovascular events. N. Engl. J. Med. 362, 1477–1490 (2010).
Pi-Sunyer, X. et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N. Engl. J. Med. 373, 11–22 (2015).
Torgerson, J. S., Hauptman, J., Boldrin, M. N. & Sjöström, L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care 27, 155–161 (2004).
Wilding, J. P. H. et al. Once-weekly semaglutide in adults with overweight or obesity. N. Engl. J. Med. 384, 989–1002 (2021).
Zinman, B. et al. Low-dose combination therapy with rosiglitazone and metformin to prevent type 2 diabetes mellitus (CANOE trial): a double-blind randomised controlled study. Lancet 376, 103–111 (2010).
Hughes, A. et al. Metformin prescription rates for patients with prediabetes. J. Am. Board Fam. Med. 35, 821–826 (2022).
Zhang, C. & Zhang, R. More effective glycaemic control by metformin in African Americans than in whites in the prediabetic population. Diabetes Metab. 41, 173–175 (2015).
Diabetes Prevention Program Research Group et al. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet 374, 1677–1686 (2009).
Moin, T. et al. Review of metformin use for type 2 diabetes prevention. Am. J. Prev. Med. 55, 565–574 (2018).
Diabetes Prevention Program Research Group. HbA1c as a predictor of diabetes and as an outcome in the diabetes prevention program: a randomized clinical trial. Diabetes Care 38, 51–58 (2015).
Zhang, L. et al. Safety and effectiveness of metformin plus lifestyle intervention compared with lifestyle intervention alone in preventing progression to diabetes in a Chinese population with impaired glucose regulation: a multicentre, open-label, randomised controlled trial. Lancet Diabetes Endocrinol. 11, 567–577 (2023).
Diabetes Prevention Program Research Group. Effects of withdrawal from metformin on the development of diabetes in the diabetes prevention program. Diabetes Care 26, 977–980 (2003).
Lehtovirta, M. et al. Metabolic effects of metformin in patients with impaired glucose tolerance. Diabet. Med. 18, 578–583 (2001).
American Diabetes Association Professional Practice Committee. 3. Prevention or delay of diabetes and associated comorbidities: standards of care in diabetes-2025. Diabetes Care 48, S50–S58 (2025).
Echouffo-Tcheugui, J. B., Perreault, L., Ji, L. & Dagogo-Jack, S. Diagnosis and management of prediabetes: a review. JAMA 329, 1206–1216 (2023).
American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2025. Diabetes Care 48, S181–S206 (2025).
Diabetes Prevention Program Research Group. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care 35, 723–730 (2012).
Azen, S. P. et al. TRIPOD (TRoglitazone in the prevention of diabetes): a randomized, placebo-controlled trial of troglitazone in women with prior gestational diabetes mellitus. Control. Clin. Trials 19, 217–231 (1998).
Xiang, A. H. et al. Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes 55, 517–522 (2006).
Defronzo, R. A. et al. Prevention of diabetes with pioglitazone in ACT NOW: physiologic correlates. Diabetes 62, 3920–3926 (2013).
Luo, Y. et al. A randomized controlled clinical trial of lifestyle intervention and pioglitazone for normalization of glucose status in Chinese with prediabetes. J. Diabetes Res. 2022, 2971382 (2022).
Chiasson, J.-L. et al. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 290, 486–494 (2003).
Rossing, P. et al. Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. Lancet Diabetes Endocrinol. 10, 24–34 (2022).
Anker, S. D. et al. Empagliflozin in heart failure with a preserved ejection fraction. N. Engl. J. Med. 385, 1451–1461 (2021).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424 (2020).
McGowan, B. M. et al. Efficacy and safety of once-weekly semaglutide 2·4 mg versus placebo in people with obesity and prediabetes (STEP 10): a randomised, double-blind, placebo-controlled, multicentre phase 3 trial. Lancet Diabetes Endocrinol. 12, 631–642 (2024).
Loomba, R. et al. Tirzepatide for metabolic dysfunction-associated steatohepatitis with liver fibrosis. N. Engl. J. Med. 391, 299–310 (2024).
Wang, W. et al. Effects of treatment with glucagon-like peptide-1 receptor agonist on prediabetes with overweight/obesity: a systematic review and meta-analysis. Diabetes Metab. Res. Rev. 39, e3680 (2023).
Mozaffarian, D. GLP-1 agonists for obesity — a new recipe for success? JAMA 331, 1007–1008 (2024).
Pittas, A. G. et al. Vitamin D and risk for type 2 diabetes in people with prediabetes: a systematic review and meta-analysis of individual participant data from 3 randomized clinical trials. Ann. Intern. Med. 176, 355–363 (2023).
Jorde, R. et al. Vitamin D 20,000 IU per week for five years does not prevent progression from prediabetes to diabetes. J. Clin. Endocrinol. Metab. 101, 1647–1655 (2016).
Pittas, A. G. et al. Vitamin D supplementation and prevention of type 2 diabetes. N. Engl. J. Med. 381, 520–530 (2019).
Kawahara, T. et al. Effect of active vitamin D treatment on development of type 2 diabetes: DPVD randomised controlled trial in Japanese population. BMJ 377, e066222 (2022).
Sim, G., Kim, Y., Lee, S. M., Hahn, J. & Kim, J. Role of vitamin D in prevention of type 2 diabetes mellitus: a systematic review and meta-analysis. Exp. Ther. Med. 28, 451 (2024).
Carris, N. W., Bunnell, B. E., Mhaskar, R., DuCoin, C. G. & Stern, M. A systematic approach to treating early metabolic disease and prediabetes. Diabetes Ther. 14, 1595–1607 (2023).
Borges-Canha, M. et al. Prediabetes remission after bariatric surgery: a 4-years follow-up study. BMC Endocr. Disord. 24, 7 (2024).
Stenberg, E., Rask, E., Szabo, E., Näslund, I. & Ottosson, J. The effect of laparoscopic gastric bypass surgery on insulin resistance and glycosylated hemoglobin A1c: a 2-year follow-up study. Obes. Surg. 30, 3489–3495 (2020).
Dicker, D. et al. Conversion from prediabetes to diabetes in individuals with obesity, 5-years post-band, sleeve, and gastric bypass surgeries. Obes. Surg. 29, 3901–3906 (2019).
Canakis, A., Wall-Wieler, E., Liu, Y., Zheng, F. & Sharaiha, R. Z. New-onset type 2 diabetes after bariatric surgery: a matched cohort study. Am. J. Prev. Med. 67, 581–585 (2024).
Lean, M. E. et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391, 541–551 (2018).
Ely, E. K. et al. A National effort to prevent type 2 diabetes: participant-level evaluation of CDC’s national diabetes prevention program. Diabetes Care 40, 1331–1341 (2017).
Herman, W. H., Villatoro, C., Joiner, K. L. & McEwen, L. N. Retention and outcomes of national diabetes prevention program enrollees and non-enrollees with prediabetes: the University of Michigan experience. J. Diabetes Complicat. 37, 108527 (2023).
Campione, J. R. et al. Use and impact of type 2 diabetes prevention interventions. Am. J. Prev. Med. 63, 603–610 (2022).
Ravindrarajah, R. et al. Referral to the NHS diabetes prevention programme and conversion from nondiabetic hyperglycaemia to type 2 diabetes mellitus in England: a matched cohort analysis. PLoS Med. 20, e1004177 (2023).
Parkinson, B., McManus, E., Meacock, R. & Sutton, M. Level of attendance at the English National Health Service diabetes prevention programme and risk of progression to type 2 diabetes. Int. J. Behav. Nutr. Phys. Act. 21, 6 (2024).
Khademi, A., Shi, L., Nasrollahzadeh, A. A., Narayanan, H. & Chen, L. Comparing the lifestyle interventions for prediabetes: an integrated microsimulation and population simulation model. Sci. Rep. 9, 11927 (2019).
Rise, M. B., Pellerud, A., Rygg, L. Ø. & Steinsbekk, A. Making and maintaining lifestyle changes after participating in group based type 2 diabetes self-management educations: a qualitative study. PLoS ONE 8, e64009 (2013).
Carlsson, L. M. S. et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N. Engl. J. Med. 367, 695–704 (2012).
Chen, X., Zhao, P., Wang, W., Guo, L. & Pan, Q. The antidepressant effects of GLP-1 receptor agonists: a systematic review and meta-analysis. Am. J. Geriatr. Psychiatry 32, 117–127 (2024).
Cezaretto, A., Siqueira-Catania, A., de Barros, C. R., Salvador, E. P. & Ferreira, S. R. G. Benefits on quality of life concomitant to metabolic improvement in intervention program for prevention of diabetes mellitus. Qual. Life Res. 21, 105–113 (2012).
Florez, H. et al. Impact of lifestyle intervention and metformin on health-related quality of life: the diabetes prevention program randomized trial. J. Gen. Intern. Med. 27, 1594 (2012).
Hoskin, M. A. et al. Prevention of diabetes through the lifestyle intervention: lessons learned from the diabetes prevention program and outcomes study and its translation to practice. Curr. Nutr. Rep. 3, 364 (2014).
Herman, W. H. et al. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann. Intern. Med. 142, 323–332 (2005).
Kuo, S. et al. Cost-effectiveness of the national diabetes prevention program: a real-world, 2-year prospective study. Diabetes Care 48, 1180–1188 (2025).
Kengne, A. P. & Ramachandran, A. Feasibility of prevention of type 2 diabetes in low- and middle-income countries. Diabetologia 67, 763–772 (2024).
Sarker, A., Das, R., Ether, S., Shariful Islam, M. & Saif-Ur-Rahman, K. M. Non-pharmacological interventions for the prevention of type 2 diabetes in low-income and middle-income countries: a systematic review of randomised controlled trials. BMJ Open 12, e062671 (2022).
Rahim, N. E. et al. Diabetes risk and provision of diabetes prevention activities in 44 low-income and middle-income countries: a cross-sectional analysis of nationally representative, individual-level survey data. Lancet Glob. Health 11, e1576–e1586 (2023).
Lemay, J., Waheedi, M., Al-Sharqawi, S. & Bayoud, T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer. Adherence 12, 1687–1698 (2018).
Ren, Z., Xu, X. & Yue, R. Preferences and adherence of people with prediabetes for disease management and treatment: a systematic review. Patient Prefer. Adherence 17, 2981 (2023).
Cannon, M. J. et al. Retention among participants in the national diabetes prevention program lifestyle change program, 2012-2017. Diabetes Care 43, 2042–2049 (2020).
Chan, J. C. N. et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301, 2129–2140 (2009).
Narayan, K. M. V., Jagannathan, R. & Ridderstråle, M. Managing type 2 diabetes needs a paradigm change. Lancet Diabetes Endocrinol. 11, 534–536 (2023).
World Health Organization. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation (WHO, 2011).
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20, 1183–1197 (1997).
Dagogo-Jack, S. et al. Outcome of lifestyle intervention in relation to duration of pre-diabetes: the pathobiology and reversibility of prediabetes in a biracial cohort (PROP-ABC) study. BMJ Open Diabetes Res. Care 10, e002748 (2022).
Poloz, Y. & Stambolic, V. Obesity and cancer, a case for insulin signaling. Cell Death Dis. 6, e2037–e2037 (2015).
Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. National diabetes data group. Diabetes 28, 1039–1057 (1979).
WHO Expert Committee on Diabetes Mellitus: second report. World Health Organ. Tech. Rep. Ser. 646, 1–80 (1980).
Looker, H. C., Chang, D. C., Baier, L. J., Hanson, R. L. & Nelson, R. G. Diagnostic criteria and etiopathogenesis of type 2 diabetes and its complications: lessons from the Pima Indians. Presse Med. 52, 104176 (2023).
Sayegh, H. A. & Jarrett, R. J. Oral glucose-tolerance tests and the diagnosis of diabetes: results of a prospective study based on the Whitehall survey. Lancet 2, 431–433 (1979).
Genuth, S. et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26, 3160–3167 (2003).
World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia https://www.who.int/publications/i/item/definition-and-diagnosis-of-diabetes-mellitus-and-intermediate-hyperglycaemia (2006).
Zhang, X. et al. A1C level and future risk of diabetes: a systematic review. Diabetes Care 33, 1665–1673 (2010).
Ramachandran, A., Snehalatha, C., Mohan, V. & Viswanathan, M. Remission in non-insulin dependent diabetes. J. Med. Assoc. Thai. 70, 185–189 (1987).
Acknowledgements
The authors acknowledge T. A. Pramod Kumar for his assistance in preparation of Tables.
Author information
Authors and Affiliations
Contributions
Introduction (R.U. and V.M.); Epidemiology (S.H.W.); Mechanisms/pathophysiology (M.R.); Diagnosis and screening (R.U., V.M. and J.E.S.); Management (A.L.P.); Quality of life (S.O.); Outlook (R.U. and V.M.); overview of the Primer (R.U. and V.M.).
Corresponding author
Ethics declarations
Competing interests
V.M. has acted as consultant and speaker, and received research or educational grants from Abbott, Medtronics, Novo Nordisk, Sanofi, Servier, Boehringer-Ingelheim, Eli Lilly, Johnson & Johnson, Lifescan, Roche, MSD, Novartis, Aventis, Bayer, USV, Dr. Reddy’s, Sun Pharma, INTAS, Lupin, Glenmark, Zydus, IPCA, Torrent, Cipla, Biocon, Primus, Franco Indian, Wockhardt, Emcure, Mankind, Fourrts, Apex, GSK and Alembic. M.R. has received lecture fees or served on advisory boards for AstraZeneca, Boehringer-Ingelheim, Echosens, Eli Lilly, Madrigal, MSD, Novo Nordisk and Target RWE and has performed investigator-initiated research with support from Boehringer-Ingelheim and Novo Nordisk to the German Diabetes Center (DDZ). J.E.S. has received lecture fees or served on advisory boards for and/or received honoraria from Zuellig Pharma, AstraZeneca, Sanofi, Novo Nordisk, Eli Lilly, Abbott, Mylan, Boehringer-Ingelheim, Roche, Pfizer and GSK. R.U., S.H.W. and S.O. declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks W. Knowler; A.E. Sumner, who co-reviewed with K. Ntabadde; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Unnikrishnan, R., Shaw, J.E., Chan, J.C.N. et al. Prediabetes. Nat Rev Dis Primers 11, 49 (2025). https://doi.org/10.1038/s41572-025-00635-0
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-025-00635-0
This article is cited by
-
Impact of skeletal muscle mass index on glycemic progression and remission in Chinese adults with prediabetes: a nationwide cohort study
European Journal of Medical Research (2025)