Abstract
Thyroid dysfunction and diabetes mellitus frequently occur together, with evidence showing higher rates of each condition in individuals affected by the other. Beyond their statistical association, emerging research indicates shared mechanisms involving autoimmunity, obesity, ageing and insulin resistance, which might explain their bidirectional relationship. This Review synthesizes current evidence on these links, with a particular focus on how thyroid dysfunction influences glycaemic control and how antidiabetic therapies affect thyroid function. Unlike earlier reviews, we frame thyroid disorders within the broader category of non-communicable diseases (NCDs), emphasizing their public health relevance and the need for greater attention in global funding and policy agendas. By combining clinical insights with a population health perspective, this Review aims to promote earlier detection, integrated management strategies and recognition of thyroid disease as a neglected NCD priority.
Key points
-
Thyroid disorders and diabetes mellitus often coexist owing to overlapping pathophysiological mechanisms and shared autoimmune and metabolic risk factors.
-
Autoimmune hypothyroidism, particularly Hashimoto thyroiditis, is significantly more prevalent in patients with type 1 diabetes mellitus owing to common genetic predispositions.
-
Hyperthyroidism can worsen glycaemic control in type 2 diabetes mellitus by increasing hepatic glucose output and insulin resistance.
-
Both hypothyroidism and hyperthyroidism can alter glucose metabolism, insulin sensitivity and the pharmacodynamics of diabetes mellitus medications.
-
Regular screening for thyroid dysfunction in patients with diabetes mellitus, especially those with type 1 diabetes mellitus, is important for timely diagnosis and management.
-
Coordinated care between endocrinologists and primary care providers is vital to address the complex interplay between thyroid function and glucose metabolism for optimal patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
ElSayed, N. A. et al. Classification and diagnosis of diabetes: standards of care in diabetes — 2023. Diabetes Care 46, S19–S40 (2023).
Sun, H. et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Handelsman, Y. et al. Cardiovascular outcomes in patients with diabetes and kidney disease: JACC review topic of the week. J. Am. Coll. Cardiol. 82, 161–170 (2023).
Sinha, R. A. & Yen, P. M. Metabolic messengers: thyroid hormones. Nat. Metab. 6, 639–650 (2024).
Chaker, L. et al. Hypothyroidism. Nat. Rev. Dis. Primers 8, 30 (2022).
Binder, G. et al. Thyroid disorders in children and adolescents: a review. JAMA Pediatr. 170, 1008–1019 (2016).
Laurberg, P. et al. Hyperthyroidism: aetiology, pathogenesis, diagnosis, management, complications, and prognosis. Lancet Diabetes Endocrinol. 11, 282–298 (2023).
Davies, T. F. et al. Graves’ disease. Autoimmune Rev. 22, 102805 (2023).
Smith, T. J. & Hegedüs, L. Graves’ disease. N. Engl. J. Med. 375, 1552–1565 (2016).
Kahaly, G. J. & Hansen, M. P. Type 1 diabetes associated autoimmunity. Autoimmun. Rev. 15, 644–648 (2016).
Hadgu, R., Worede, A. & Ambachew, S. Prevalence of thyroid dysfunction and associated factors among adult type 2 diabetes mellitus patients, 2000–2022: a systematic review and meta-analysis. Syst. Rev. 13, 119 (2024).
Gronich, N. et al. Hypothyroidism is a risk factor for new-onset diabetes mellitus: a population-based cohort study. BMC Med. 19, 257 (2021).
Rong, F. et al. Association between thyroid dysfunction and type 2 diabetes: a meta-analysis of prospective observational studies. BMC Med. 19, 257 (2021).
Dueñas, O. H. R. et al. Thyroid function and the risk of prediabetes and type 2 diabetes. J. Clin. Endocrinol. Metab. 107, 1789–1798 (2025).
Biondi, B., Kahaly, G. J. & Robertson, R. P. Thyroid dysfunction and diabetes mellitus: two closely associated disorders. Endocr. Rev. 40, 789–824 (2019).
Mobasseri, M. et al. Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Health Promot. Perspect. 10, 98–115 (2020).
Abela, A. G. & Fava, S. Why is the incidence of type 1 diabetes increasing. Curr. Diabetes Rev. 17, e030521193110 (2021).
Herczeg, V. et al. Increasing prevalence of thyroid autoimmunity in childhood type 1 diabetes in the pre-COVID but not during the COVID era. Front. Endocrinol. 15, 1496155 (2025).
Nederstigt, C., Corssmit, E. P. M., de Koning, E. J. P. & Dekkers, O. M. Incidence and prevalence of thyroid dysfunction in type 1 diabetes. J. Diabetes Complications 30, 420–425 (2016).
Frommer, L. & Kahaly, G. J. Type 1 diabetes and associated autoimmune diseases. World J. Diabetes 11, 527–539 (2020).
National Institute for Health and Care Excellence. When should I screen for hypothyroidism? NICE https://cks.nice.org.uk/topics/hypothyroidism/diagnosis/screening/ (2024).
Garber, J. R. et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr. Pract. 18, 988–1028 (2012).
Birtwhistle, R. et al. Recommendation on screening adults for asymptomatic thyroid dysfunction in primary care. CMAJ 191, E1274–E1280 (2019).
Huang, X., Wu, Y., Ni, Y. & He, Y. Global, regional, and national burden of type 2 diabetes mellitus caused by high BMI from 1990 to 2021, and forecast to 2045: analysis from the Global Burden of Disease Study 2021. Front. Public. Health 13, 1515797 (2025).
Guzman-Vilca, W. C. & Carrillo-Larco, R. M. Number of people with type 2 diabetes mellitus in 2035 and 2050: a modelling study in 188 countries. Curr. Diabetes Rev. 21, e120124225603 (2024).
Kyrou, I. et al. Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: a narrative review with emphasis on data from Europe. BMC Endocr. Disord. 20, 134 (2020).
Fleiner, H. F. et al. Prevalence of thyroid dysfunction in autoimmune and type 2 diabetes: the population-based HUNT study in Norway. J. Clin. Endocrinol. Metab. 101, 669–677 (2016).
Benseñor, I. M. et al. Thyrotropin levels, insulin resistance, and metabolic syndrome: a cross-sectional analysis in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Metab. Syndr. Relat. Disord. 13, 362–369 (2015).
Roos, A. et al. Thyroid function is associated with components of the metabolic syndrome in euthyroid subjects. J. Clin. Endocrinol. Metab. 92, 491–496 (2007).
Jun, J. E. et al. Association between changes in thyroid hormones and incident type 2 diabetes: a seven-year longitudinal study. Thyroid 27, 29–38 (2017).
Alwan, H. et al. Subclinical thyroid dysfunction and incident diabetes: a systematic review and an individual participant data analysis of prospective cohort studies. Eur. J. Endocrinol. 187, S35–S46 (2022).
Pinto, S., Croce, L., Carlier, L., Cosson, E. & Rotondi, M. Thyroid dysfunction during gestation and gestational diabetes mellitus: a complex relationship. J. Endocrinol. Invest. 46, 1737–1759 (2023).
Pinto, S. et al. Association between hypothyroidism and metabolic profile in gestational diabetes mellitus. Front. Endocrinol. 16, 1614802 (2025).
Eom, Y. S., Wilson, J. R. & Bernet, V. J. Links between thyroid disorders and glucose homeostasis. Diabetes Metab. J. 46, 239–256 (2022).
Giannakou, K. et al. Risk factors for gestational diabetes: an umbrella review of meta-analyses of observational studies. PLoS ONE 14, e0215372 (2019).
Osinga, J. A. J. et al. Association of gestational thyroid function and thyroid autoimmunity with gestational diabetes: a systematic review and individual participant meta-analysis. Lancet Diabetes Endocrinol. 13, 651–661 (2025).
Zou, C., Shen, Q., Yang, Y., Liao, Y. & Du, Q. Association of maternal thyroid function and gestational diabetes with pregnancy outcomes: a retrospective cohort study. Front. Endocrinol. 16, 1555409 (2025).
Alexander, E. K. et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27, 315–389 (2017).
[No authors listed] Thyroid disease in pregnancy: ACOG Practice Bulletin, number 223. Obstet. Gynecol. 135, e261–e274 (2020).
Stagnaro-Green, A., Dong, A. & Stephenson, M. D. Universal screening for thyroid disease during pregnancy should be performed. Best. Pract. Res. Clin. Endocrinol. Metab. 34, 101320 (2020).
Delgado-Rodríguez, M. & Llorca, J. Bias. J. Epidemiol. Community Health 58, 635–641 (2004).
Perros, P., McCrimmon, R. J., Shaw, G. & Frier, B. M. Frequency of thyroid dysfunction in diabetic patients: value of annual screening. Diabet. Med. 12, 622–627 (1995).
Flynn, R. W. et al. The thyroid epidemiology, audit, and research study: thyroid dysfunction in the general population. J. Clin. Endocrinol. Metab. 89, 3879–3884 (2004).
Pleić, N., Gunjača, I., Babić Leko, M. & Zemunik, T. Thyroid function and metabolic syndrome: a two-sample bidirectional Mendelian randomization study. J. Clin. Endocrinol. Metab. 108, 3190–3200 (2023).
Jonklaas, J. & Razvi, S. Reference intervals in the diagnosis of thyroid dysfunction: treating patients not numbers. Lancet Diabetes Endocrinol. 7, 473–483 (2019).
Guan, B. et al. Effect of bariatric surgery on thyroid function in obese patients: a systematic review and meta-analysis. Obes. Surg. 27, 3292–3305 (2017).
Lips, M. A. et al. Roux-en-Y gastric bypass and calorie restriction induce comparable time-dependent effects on thyroid hormone function tests in obese female subjects. Eur. J. Endocrinol. 169, 339–347 (2013).
Azran, C. et al. Hypothyroidism and levothyroxine therapy following bariatric surgery: a systematic review, meta-analysis, network meta-analysis, and meta-regression. Surg. Obes. Relat. Dis. 17, 1206–1217 (2021).
Tee, S. A., Tsatlidis, V. & Razvi, S. The GLP-1 receptor agonist exenatide reduces serum TSH by its effect on body weight in people with type 2 diabetes. Clin. Endocrinol. 99, 401–408 (2023).
Santini, F. et al. Mechanisms in endocrinology: the crosstalk between thyroid gland and adipose tissue: signal integration in health and disease. Eur. J. Endocrinol. 171, R137–R152 (2014).
Fontenelle, L. C. et al. Thyroid function in human obesity: underlying mechanisms. Horm. Metab. Res. 48, 787–794 (2016).
Nannipieri, M. et al. Expression of thyrotropin and thyroid hormone receptors in adipose tissue of patients with morbid obesity and/or type 2 diabetes: effects of weight loss. Int. J. Obes. 33, 1001–1006 (2009).
Chen, X., Zhang, C., Liu, W., Zhang, J. & Zhou, Z. Laparoscopic sleeve gastrectomy-induced decreases in FT3 and TSH are related to fasting C-peptide in euthyrioid patients with obesity. Diabetes. Metab. Syndr. Obes. 13, 4077–4084 (2020).
Wang, X. et al. Causal association between serum thyrotropin and obesity: a bidirectional, Mendelian randomization study. J. Clin. Endocrinol. Metab. 106, e4251–e4259 (2021).
Feller, M. et al. Association of thyroid hormone therapy with quality of life and thyroid-related symptoms in patients with subclinical hypothyroidism: a systematic review and meta-analysis. JAMA 320, 1349–1359 (2018).
Okosieme, O. et al. Management of primary hypothyroidism: statement by the British Thyroid Association executive committee. Clin. Endocrinol. 84, 799–808 (2016).
Razvi, S., Korevaar, T. I. M. & Taylor, P. Trends, determinants, and associations of treated hypothyroidism in the United Kingdom, 2005–2014. Thyroid 29, 174–182 (2019).
Song, F. et al. The prevalence and determinants of hypothyroidism in hospitalized patients with type 2 diabetes mellitus. Endocrine 55, 179–185 (2017).
McCahon, D., Haque, M. S., Parle, J., Hobbs, F. R. & Roberts, L. M. Subclinical thyroid dysfunction symptoms in older adults: cross-sectional study in UK primary care. Br. J. Gen. Pract. 70, e208–e214 (2020).
Hollowell, J. G. et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J. Clin. Endocrinol. Metab. 87, 489–499 (2002).
Javaid, U., Kennedy, D., Addison, C., Tsatlidis, V. & Razvi, S. Frequency, determinants and costs of thyroid function testing in a laboratory serving a large population. Eur. J. Endocrinol. 186, 553–560 (2022).
Surks, M. I. & Hollowell, J. G. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 92, 4575–4582 (2007).
Zhai, X. et al. An age-specific serum thyrotropin reference range for the diagnosis of thyroid diseases in older adults: a cross-sectional survey in China. Thyroid 28, 1571–1579 (2018).
Lee, S. Y. & Pearce, E. N. Hyperthyroidism: a review. JAMA 330, 1472–1483 (2023).
Han, C. et al. Subclinical hypothyroidism and type 2 diabetes: a systematic review and meta-analysis. PLoS ONE 10, e0135233 (2015).
Bano, A. et al. Thyroid function and the risk of fibrosis of the liver, heart, and lung in humans: a systematic review and meta-analysis. Thyroid 30, 806–820 (2020).
Ding, X. et al. Subclinical hypothyroidism in polycystic ovary syndrome: a systematic review and meta-analysis. Front. Endocrinol. 9, 700 (2018).
Vyakaranam, S., Vanaparthy, S., Nori, S., Palarapu, S. & Bhongir, A. V. Study of insulin resistance in subclinical hypothyroidism. Int. J. Health Sci. Res. 4, 147–153 (2014).
Lu, C. & Cheng, S. Y. Thyroid hormone receptors regulate adipogenesis and carcinogenesis via crosstalk signaling with peroxisome proliferator-activated receptors. J. Mol. Endocrinol. 44, 143–154 (2010).
Moskva, K. A. et al. Effect of pioglitazone on thyroid stimulating hormone and insulin resistance in hypothyroid patients [abstract 976]. Diabetologia 58, 1–607 (2015).
Lupoli, R. et al. Effects of treatment with metformin on TSH levels: a meta-analysis of literature studies. J. Clin. Endocrinol. Metab. 99, E143–E148 (2014).
Kim, H. J. et al. Thyroid autoimmunity and metabolic syndrome: a nationwide population-based study. Eur. J. Endocrinol. 185, 707–715 (2021).
Hoffmann, C. J. & Brown, T. T. Thyroid function abnormalities in HIV-infected patients. Clin. Infect. Dis. 45, 488–494 (2007).
Melamed, S. B. et al. Thyroid function assessment before and after diagnosis of schizophrenia: a community-based study. Psychiatry Res. 293, 113356 (2020).
Shanbhogue, V. V., Finkelstein, J. S., Bouxsein, M. L. & Yu, E. W. Association between insulin resistance and bone structure in nondiabetic postmenopausal women. J. Clin. Endocrinol. Metab. 101, 3114–3122 (2016).
Jansen, H. I., Bruinstroop, E., Heijboer, A. C. & Boelen, A. Biomarkers indicating tissue thyroid hormone status: ready to be implemented yet? J. Endocrinol. 253, R21–R45 (2022).
Birkebaek, N. H. et al. Effect of weight reduction on insulin sensitivity, sex hormone-binding globulin, sex hormones and gonadotrophins in obese children. Eur. J. Endocrinol. 163, 895–900 (2010).
Krause, C. et al. Reduced expression of thyroid hormone receptor β in human nonalcoholic steatohepatitis. Endocr. Connect. 7, 1448–1456 (2018).
Harrison, S. A. et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 394, 2012–2024 (2019).
de Candia, P. et al. Type 2 diabetes: how much of an autoimmune disease? Front. Endocrinol. 10, 451 (2019).
Hawa, M. I. et al. Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: Action LADA 7. Diabetes Care 36, 908–913 (2013).
Diamanti-Kandarakis, E. et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr. Rev. 30, 293–342 (2009).
Gore, A. C. et al. EDC-2: The Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev. 36, E1–E150 (2015).
Howard, S. G. Developmental exposure to endocrine disrupting chemicals and type 1 diabetes mellitus. Front. Endocrinol. 9, 513 (2018).
Calsolaro, V., Pasqualetti, G., Niccolai, F., Caraccio, N. & Monzani, F. Thyroid disrupting chemicals. Int. J. Mol. Sci. 18, 2583 (2017).
Hinault, C., Caroli-Bosc, P., Bost, F. & Chevalier, N. Critical overview on endocrine disruptors in diabetes mellitus. Int. J. Mol. Sci. 24, 4537 (2023).
Martinez-Pinna, J. et al. Endocrine disruptors in plastics alter β-cell physiology and increase the risk of diabetes mellitus. Am. J. Physiol. Endocrinol. Metab. 324, E488–E505 (2023).
Kohrle, J. & Fradrich, C. Thyroid hormone system disrupting chemicals. Best. Pract. Res. Clin. Endocrinol. Metab. 35, 101562 (2021).
Goulart-Silva, F., Serrano-Nascimento, C., Texeira, S. S. & Nunes, M. T. Triiodothyronine (T3) induces proinsulin gene expression by activating PI3K: possible roles for GSK-3β and the transcriptional factor PDX-1. Exp. Clin. Endocrinol. Diabetes. 121, 14–19 (2013).
Ortega, F. J. et al. Subcutaneous fat shows higher thyroid hormone receptor-α1 gene expression than omental fat. Obesity 17, 2134–2141 (2009).
Wang, C. The relationship between type 2 diabetes mellitus and related thyroid diseases. J. Diabetes Res. 2013, 390534 (2013).
Weitzel, J. M. & Iwen, K. A. Coordination of mitochondrial biogenesis by thyroid hormone. Mol. Cell Endocrinol. 342, 1–7 (2011).
Marino, L., Kim, A., Ni, B. & Celi, F. S. Thyroid hormone action and liver disease, a complex interplay. Hepatology 81, 651–669 (2025).
Videla, L. A. et al. T3-induced liver AMP-activated protein kinase signaling: redox dependency and upregulation of downstream targets. World. J. Gastoenterol. 20, 17416–17425 (2014).
Falzacappa, C. V. et al. Thyroid hormone receptor TRβ1 mediates Akt activation by T3 in pancreatic β cells. J. Mol. Endocrinol. 38, 221–233 (2007).
Morte, B. & Bernal, J. Thyroid hormone action: astrocyte-neuron communication. Front. Endocrinol. 5, 82 (2014).
Chen, G., Xu, S., Renko, K. & Derwahi, M. Metformin inhibits growth of thyroid carcinoma cells, suppresses self-renewal of derived cancer stem cells, and potentiates the effect of chemotherapeutic agents. J. Clin. Endocrinol. Metab. 97, E510–E520 (2012).
Liu, S. et al. Circulating leptin levels in thyroid dysfunction: a systematic review and meta-analysis. BMC Endocr. Disord. 25, 140 (2025).
Markos, I. S. et al. The concentration of interleukin 6 and tumor necrosis factor alpha in saliva and blood of patients with inactive multiple sclerosis and coexisting Hashimoto’s thyroiditis. Acta Clin. Croat. 62, 339–344 (2023).
Tjorve, E., Tjorve, K. M. C., Olsen, J. O., Senum, R. & Oftebro, H. On commonness and rarity of thyroid hormone resistance: a discussion based on mechanisms of reduced sensitivity in peripheral tissues. Med. Hypotheses. 69, 913–921 (2007).
Lacraustra, M. et al. Impaired sensitivity to thyroid hormones is associated with diabetes and metabolic syndrome. Diabetes Care 42, 303–310 (2019).
Sun, Y. et al. Impaired sensitivity to thyroid hormones is associated with hyperuricemia, obesity, and cardiovascular disease risk in subjects with subclinical hypothyroidism. Thyroid 32, 376–384 (2022).
Zhang, C. et al. Effects of acarbose and metformin on thyroid function and thyroid hormone sensitivity in type 2 diabetes patients: a post-hoc analysis of the MARCH study. J. Endocrinol. Invest. 48, 419–433 (2025).
Sessa, L., Malavolta, E., Sodero, G., Cipolla, C. & Rigante, D. The conspiring role of gut microbiota as primer of autoimmune thyroid diseases: a scoping focus. Autoimm. Rev. 24, 103780 (2025).
Canfora, E. E., Meex, R. C. R., Venema, K. & Blaak, E. E. Gut microbial metabolites in obesity, NAFLD and T2DM. Nat. Rev. Endocrinol. 15, 261–273 (2019).
Wu, J., Yang, K., Fan, H., Wei, M. & Xiong, Q. Targeting the gut microbiota and its metabolites for type 2 diabetes mellitus. Front. Endocrinol. 14, 1114424 (2023).
Jiang, T. et al. Gut microbiota in hypothyroidism: pathogenic mechanisms and opportunities for precision microbiome interventions. Front. Microbiol. 16, 1661211 (2025).
Shu, Q. et al. Effect of probiotics or prebiotics on thyroid function: a meta-analysis of eight randomized controlled trials. PLoS ONE 19, e0296733 (2024).
Gray, R. S., Borsey, D. Q., Irvine, W. J., Seth, J. & Clarke, B. F. Natural history of thyroid function in diabetics with impaired thyroid reserve: a four year controlled study. Clin. Endocrinol. 19, 445–451 (1983).
Wang, J., Gao, J., Fan, Q., Li, H. & Di, Y. The effect of metformin on thyroid-associated serum hormone levels and physiological indexes: a meta-analysis. Curr. Pharm. Des. 25, 3257–3265 (2019).
Sencar, M. E. et al. The effect of exenatide on thyroid-stimulating hormone and thyroid volume. Eur. Thyroid. J. 8, 307–311 (2019).
Köseoğlu, D., Özdemir Başer, Ö, Berker, D. & Güler, S. Exenatide treatment reduces thyroid gland volume, but has no effect on the size of thyroid nodules. Acta Endocrinol. 16, 275–279 (2020).
Ye, J., Xu, J., Wen, W. & Huang, B. Effect of liraglutide on serum TSH levels in patients with NAFLD and its underlying mechanisms. Int. J. Clin. Pract. 2022, 1786559 (2022).
Hitsuwari, T. et al. Two cases of thyrotoxicosis and euglycemic diabetic ketoacidosis under sodium-glucose transport protein 2 inhibitor treatment. Intern. Med. 61, 3069–3075 (2022).
Nikkila, E. A. & Teir, H. Effects of long-term use of antidiabetic sulfonylureas on thyroid weight and arteriosclerosis. Ann. Med. Exp. Biol. Fenn. 38, 182–185 (1960).
Lee, S., Tsirbas, A., Goldberg, R. A. & McCann, J. D. Thiazolidinedione induced thyroid associated orbitopathy. BMC Ophthalmol. 7, 8 (2007).
Brent, G. A. Mechanisms of thyroid hormone action. J. Clin. Invest. 122, 3035–3043 (2012).
Klieverik, L. P. et al. Effects of thyrotoxicosis and selective hepatic autonomic denervation on hepatic glucose metabolism in rats. Am. J. Physiol. Endocrinol. Metab. 294, E513–E520 (2008).
Randin, J. P., Tappy, L., Scazziga, B., Jequier, E. & Felber, J. P. Insulin sensitivity and exogenous insulin clearance in Graves’ disease. Measurement by the glucose clamp technique and continuous indirect calorimetry. Diabetes 35, 178–181 (1986).
Foss, M. C. et al. Peripheral glucose metabolism in human hyperthyroidism. J. Clin. Endocrinol. Metab. 70, 1167–1172 (1990).
Havekes, B. & Sauerwein, H. P. Adipocyte-myocyte crosstalk in skeletal muscle insulin resistance; is there a role for thyroid hormone. Curr. Opin. Clin. Nutr. Metab. Care 13, 641–646 (2010).
Cooper, D. S. Antithyroid drugs. N. Engl. J. Med. 352, 905–917 (2005).
Bartalena, L. Diagnosis and management of Graves’ disease: a global overview. Nat. Rev. Endocrinol. 9, 724–734 (2013).
Tan, L. et al. NOACs versus warfarin in people with atrial fibrillation and thyroid dysfunction. Medicine 104, e43328 (2025).
Jonklaas, J. et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association Task Force on thyroid hormone replacement. Thyroid 24, 1670–1751 (2014).
Dimitriadis, G. et al. Insulin action in adipose tissue and muscle in hypothyroidism. J. Clin. Endocrinol. Metab. 91, 4930–4937 (2006).
Mohn, A., Di Michele, S., Di Luzio, R., Tumini, S. & Chiarelli, F. The effect of subclinical hypothyroidism on metabolic control in children and adolescents with type 1 diabetes mellitus. Diabet. Med. 19, 70–73 (2002).
Ostadrahimi, A. et al. Effects of levothyroxine replacement therapy on insulin resistance in patients with untreated primary hypothyroidism. BMC Res. Notes 16, 237 (2023).
Cooper, D. S. & Biondi, B. Subclinical thyroid disease. Lancet 379, 1142–1154 (2012).
Rodondi, N. et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA 304, 1365–1374 (2010).
Collet, T. H. et al. Subclinical hyperthyroidism and the risk of coronary heart disease and mortality. Arch. Intern. Med. 172, 799–809 (2012).
Pearce, S. H. et al. 2013 ETA guideline: management of subclinical hypothyroidism. Eur. Thyroid. J. 2, 215–228 (2013).
Biondi, B. et al. The 2015 European Thyroid Association guidelines on diagnosis and treatment of endogenous subclinical hyperthyroidism. Eur. Thyroid. J. 4, 149–163 (2015).
Zijlstra, L. E. et al. Levothyroxine treatment and cardiovascular outcomes in older people with subclinical hypothyroidism: pooled individual results of two randomised controlled trials. Front. Endocrinol. 12, 674841 (2021).
Acknowledgements
Review criteria
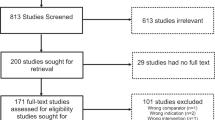
Relevant studies were identified through PubMed and Google Scholar searches up to June 2025 using combinations of the terms ‘diabetes mellitus’, ‘thyroid dysfunction’, ‘hypothyroidism’, ‘hyperthyroidism’, ‘obesity’, ‘autoimmunity’ and ‘non-communicable diseases’. Priority was given to publications from the past decade, including epidemiological studies, clinical trials and mechanistic research, with seminal older works cited where foundational. Narrative reviews and meta-analyses were used for context, and references were selected for their quality, relevance and contribution to understanding the epidemiology, mechanisms or management of coexisting diabetes mellitus and thyroid dysfunction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Mario Rotondi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Razvi, S. The public health burden of diabetes mellitus and thyroid disease: twin epidemics. Nat Rev Endocrinol (2026). https://doi.org/10.1038/s41574-025-01226-5
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41574-025-01226-5