Abstract
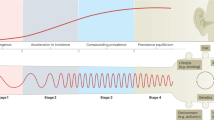
Inflammatory bowel disease (IBD) is a global disease; its evolution can be stratified into four epidemiological stages: Emergence, Acceleration in Incidence, Compounding Prevalence and Prevalence Equilibrium. In 2020, developing countries are in the Emergence stage, newly industrialized countries are in the Acceleration in Incidence stage, and Western regions are in the Compounding Prevalence stage. Western regions will eventually transition to the Prevalence Equilibrium stage, in which the accelerating prevalence levels off as the IBD population ages and possibly as a result of an unexpected rise in mortality during the COVID-19 pandemic. Mitigating the global burden of IBD will require concerted efforts in disease prevention and health-care delivery innovations that respond to changing demographics of the global IBD population. In this Perspective, we summarize the global epidemiology of IBD and use these data to stratify disease evolution into four epidemiological stages.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Kaplan, G. G. The global burden of IBD: from 2015 to 2025. Nat. Rev. Gastroenterol. Hepatol. 12, 720–727 (2015).
Kaplan, G. G. & Ng, S. C. Globalisation of inflammatory bowel disease: perspectives from the evolution of inflammatory bowel disease in the UK and China. Lancet Gastroenterol. Hepatol. 1, 307–316 (2016).
Molodecky, N. A. et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 142, 46–54 (2012).
Ng, S. C. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390, 2769–2778 (2018).
Omran, A. R. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem. Fund. Q. 49, 509–538 (1971).
Barrett, B., Charles, J. W. & Temte, J. L. Climate change, human health, and epidemiological transition. Prev. Med. 70, 69–75 (2015).
Zuckerman, M. K., Harper, K. N., Barrett, R. & Armelagos, G. J. The evolution of disease: anthropological perspectives on epidemiologic transitions. Glob. Health Action. 7, 23303 (2014).
Kedia, S. & Ahuja, V. Is the emergence of inflammatory bowel disease a prime example of “the third epidemiological transition”? Indian J. Gastroenterol. 37, 183–185 (2018).
Coward, S. et al. Past and future burden of inflammatory bowel diseases based on modeling of population-based data. Gastroenterology 156, 1345–1353 (2019).
Kaplan, G. G. & Ng, S. C. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology 152, 313–321 (2017).
Darwin, C. On the Origin of Species by Means of Natural Selection, or the Preservation of Favoured Races in the Struggle for Life (J. Murray, 1859).
Orrego, F. & Quintana, C. Darwin’s illness: a final diagnosis. Notes Rec. R. Soc. Lond. 61, 23–29 (2007).
Baillie, M. The Morbid Anatomy of Some of the Most Important Parts of the Human Body (J. Johnson, 1793).
Abercrombie, J. Pathological and Practical Researches on Diseases of the Stomach, the Intestinal Canal, the Liver and other Viscera of the Abdomen (Carey & Lea, 1828).
Wilks, S. Morbid appearances in the intestine of Miss Bankes. Lond. Med. Gazette 2, 264 (1859).
White, H. A discussion on “ulcerative colitis.” Introductory address. Proc. R. Soc. Med. 2, 79–82 (1909).
Mulder, D. J., Noble, A. J., Justinich, C. J. & Duffin, J. M. A tale of two diseases: the history of inflammatory bowel disease. J. Crohns Colitis 8, 341–348 (2014).
Allchin, W. H. A discussion on “ulcerative colitis”: introductory address. Proc. R. Soc. Med. 2, 59–75 (1909).
Dalziel, T. K. Chronic interstitial enteritis. Br. Med. J. 2, 1068–1070 (1913).
Crohn, B. B., Ginzburg, L. & Oppenheimer, G. D. Regional ileitis: a pathologic and clinical entity. J. Am. Med. Assoc. 99, 1323–1329 (1932).
Chopra, R. N. & Ray, P. N. Chronic ulcerative colitis. Ind. Med. Gaz. 74, 65–74 (1939).
Jiang, X. L. & Cui, H. F. An analysis of 10218 ulcerative colitis cases in China. World J. Gastroenterol. 8, 158–161 (2002).
Crutzen, P. J. & Stoermer, E. F. Anthropocene. IGBP Glob. Change Newslet. 41, 17–18 (2000).
Waters, C. N. et al. The Anthropocene is functionally and stratigraphically distinct from the Holocene. Science 351, aad2622 (2016).
Steffen, W., Broadgate, W., Deutsch, L., Gaffney, O. & Ludwig, C. The trajectory of the Anthropocene: the Great Acceleration. Anthr. Rev. 2, 81–98 (2015).
Roser M., Ritchie H. & Ortiz-Ospina E. World Population Growth. https://ourworldindata.org/world-population-growth (2019).
Steffen, W., Crutzen, J. & McNeill, J. R. The Anthropocene: are humans now overwhelming the great forces of Nature? Ambio 36, 614–621 (2007).
Shivashankar, R., Tremaine, W. J., Harmsen, W. S. & Loftus, E. V. Jr. Incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted county, Minnesota from 1970 through 2010. Clin. Gastroenterol. Hepatol. 15, 857–863 (2017).
Gunesh, S., Thomas, G. A., Williams, G. T., Roberts, A. & Hawthorne, A. B. The incidence of Crohn’s disease in Cardiff over the last 75 years: an update for 1996–2005. Aliment. Pharmacol. Ther. 27, 211–219 (2008).
Mayberry, J., Rhodes, J. & Hughes, L. E. Incidence of Crohn’s disease in Cardiff between 1934–1977. Gut 20, 602–608 (1979).
Rose, J. D., Roberts, G. M., Williams, G., Mayberry, J. F. & Rhodes, J. Cardiff Crohn’s disease jubilee: the incidence over 50 years. Gut 29, 346–351 (1988).
Loftus, E. V. Jr. et al. Ulcerative colitis in Olmsted County, Minnesota, 1940–1993: incidence, prevalence, and survival. Gut 46, 336–343 (2000).
Jacobsen, B. A. et al. Increase in incidence and prevalence of inflammatory bowel disease in northern Denmark: a population-based study, 1978–2002. Eur. J. Gastroenterol. Hepatol. 18, 601–606 (2006).
Björnsson, S. Inflammatory bowel disease in Iceland during a 30-year period, 1950–1979. Scand. J. Gastroenterol. Suppl. 170, 47–79 (1989).
Lakatos, L. et al. Striking elevation in incidence and prevalence of inflammatory bowel disease in a province of western Hungary between 1977–2001. World J. Gastroenterol. 10, 404–409 (2004).
Kaplan, G. G. et al. The impact of inflammatory bowel disease in Canada 2018: epidemiology. J. Can. Assoc. Gastroenterol. 2, S6–S16 (2019).
Benchimol, E. I. et al. Changing age demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflamm. Bowel Dis. 20, 1761–1769 (2014).
Roberts S. E. et al. A systematic review and meta analysis of paediatric inflammatory bowel disease incidence and prevalence across Europe. J. Crohns Colitis https://doi.org/10.1093/ecco-jcc/jjaa037 (2020).
Benchimol, E. I. et al. Incidence, outcomes, and health services burden of very early onset inflammatory bowel disease. Gastroenterology 147, 803–813 (2014).
Su, H. Y., Gupta, V., Day, A. S. & Gearry, R. B. Rising incidence of inflammatory bowel disease in Canterbury, New Zealand. Inflamm. Bowel Dis. 22, 2238–2244 (2016).
Chaaro Benallal, D. et al. Evolution of the incidence of inflammatory bowel disease in Southern Spain. Rev. Esp. Enferm. Dig. 109, 757–760 (2017).
Lophaven, S. N., Lynge, E. & Burisch, J. The incidence of inflammatory bowel disease in Denmark 1980–2013: a nationwide cohort study. Aliment. Pharmacol. Ther. 45, 961–972 (2017).
Leddin, D., Tamim, H. & Levy, A. R. Decreasing incidence of inflammatory bowel disease in eastern Canada: a population database study. BMC Gastroenterol. 14, 140 (2014).
Hammer, T., Nielsen, K. R., Munkholm, P., Burisch, J. & Lynge, E. The Faroese IBD study: incidence of inflammatory bowel diseases across 54 years of population-based data. J. Crohns Colitis. 10, 934–942 (2016).
Molodecky, N. A. et al. Challenges associated with identifying the environmental determinants of the inflammatory bowel diseases. Inflamm. Bowel Dis. 17, 1792–1799 (2011).
Hammer, T. et al. Dietary risk factors for inflammatory bowel diseases in a high-risk population: results from the Faroese IBD study. U. Eur. Gastroenterol. J. 7, 924–932 (2019).
Abdulla, M. et al. Inflammatory bowel disease in Bahrain: single-center experience. Clin. Exp. Gastroenterol. 10, 133–145 (2017).
Mokhtar, N. M. et al. A four-decade analysis of the incidence trends, sociodemographic and clinical characteristics of inflammatory bowel disease patients at single tertiary centre, Kuala Lumpur, Malaysia. BMC Public Health 19, 550 (2019).
Kotze, P. G. et al. Progression of inflammatory bowel diseases throughout Latin America and the Caribbean: a systematic review. Clin. Gastroenterol. Hepatol. 18, 304–312 (2020).
Victoria, C. R., Sassak, L. Y. & Nunes, H. R. Incidence and prevalence rates of inflammatory bowel diseases, in midwestern of Sao Paulo State, Brazil. Arq. Gastroenterol. 46, 20–25 (2009).
Gasparini, R. G., Sassaki, L. Y. & Saad-Hossne, R. Inflammatory bowel disease epidemiology in Sao Paulo State, Brazil. Clin. Exp. Gastroenterol. 11, 423–429 (2018).
Ng, S. C. et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn’s and colitis epidemiology study. Gastroenterology 145, 158–165 (2013).
Ng, S. C. et al. Population density and risk of inflammatory bowel disease: a prospective population-based study in 13 countries or regions in Asia-Pacific. Am. J. Gastroenterol. 114, 107–115 (2019).
Ananthakrishnan, A. N. Epidemiology and risk factors for IBD. Nat. Rev. Gastroenterol. Hepatol. 12, 205–217 (2015).
Mak, W. Y., Zhao, M., Ng, S. C. & Burisch, J. The epidemiology of inflammatory bowel disease: East meets west. J. Gastroenterol. Hepatol. 35, 380–389 (2020).
Ng, S. C. et al. Environmental risk factors in inflammatory bowel disease: a population-based case-control study in Asia-Pacific. Gut 64, 1063–1071 (2015).
Kedia, S. & Ahuja, V. Epidemiology of inflammatory bowel disease in India: the great shift east. Inflamm. Intest. Dis. 2, 102–115 (2017).
Freeman, J. & Hutchison, G. B. Prevalence, incidence and duration. Am. J. Epidemiol. 112, 707–723 (1980).
Feenstra, T. L., van Genugten, M. L., Hoogenveen, R. T., Wouters, E. F. & Rutten-van Mölken, M. P. The impact of aging and smoking on the future burden of chronic obstructive pulmonary disease: a model analysis in the Netherlands. Am. J. Respir. Crit. Care Med. 164, 590–596 (2001).
Brookmeyer, R. & Gray, S. Methods for projecting the incidence and prevalence of chronic diseases in aging populations: application to Alzheimer’s disease. Stat. Med. 19, 1481–1493 (2000).
Etzioni, R., Cha, R., Feuer, E. J. & Davidov, O. Asymptomatic incidence and duration of prostate cancer. Am. J. Epidemiol. 148, 775–785 (1998).
Gail, M. H., Kessler, L., Midthune, D. & Scoppa, S. Two approaches for estimating disease prevalence from population-based registries of incidence and total mortality. Biometrics 55, 1137–1144 (1999).
Bitton, A., Vutcovici, M., Sewitch, M., Suissa, S. & Brassard, P. Mortality trends in Crohn’s disease and ulcerative colitis: a population-based study in Quebec, Canada. Inflamm. Bowel Dis. 22, 416–423 (2016).
Burisch, J. et al. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut 63, 588–597 (2014).
Coward, S. et al. The evolving incidence of inflammatory bowel disease: what will the future hold? J. Can. Assoc. Gastroenterol. 2, 56–58 (2019).
Benchimol, E. I. et al. Inflammatory bowel disease in immigrants to Canada and their children: a population-based cohort study. Am. J. Gastroenterol. 110, 553–563 (2015).
Sedlack, R. E., Nobrega, F. T., Kurland, L. T. & Sauer, W. G. Inflammatory colon disease in Rochester, Minnesota, 1935-1964. Gastroenterology 62, 935–941 (1972).
Loftus, E. V. Jr. et al. Crohn’s disease in Olmsted County, Minnesota, 1940–1993: incidence, prevalence, and survival. Gastroenterology 114, 1161–1168 (1998).
Jones, G. R. et al. IBD prevalence in Lothian, Scotland, derived by capture-recapture methodology. Gut 68, 1953–1960 (2019).
Coward S. Forecasting the Future: A Trek through the Changing Landscape of Inflammatory Bowel Disease. Thesis, Univ. Calgary (2019).
Knickman, J. R. & Snell, E. K. The 2030 problem: caring for aging baby boomers. Health Serv. Res. 37, 849–884 (2002).
Muszynska, M. M. & Rau, R. The old-age healthy dependency ratio in Europe. J. Popul. Ageing 5, 151–162 (2012).
Sanderson, W. C. & Scherbov, S. Average remaining lifetimes can increase as human populations age. Nature 435, 811–813 (2005).
Appleby, J. How long can we expect to live? BMJ 346, f331 (2013).
Nguyen, G. C. et al. The impact of inflammatory bowel disease in Canada 2018: IBD in seniors. J. Can. Assoc. Gastroenterol. 2, S68–S72 (2019).
Bernstein, C. N., Nugent, Z., Targownik, L. E., Singh, H. & Lix, L. M. Predictors and risks for death in a population-based study of persons with IBD in Manitoba. Gut 64, 1403–1411 (2015).
Windsor, J. W. et al. Parallel epidemiologies in newly vs. highly industrialized countries. J. Can. Assoc. Gastroenterol. 3, 34–35 (2020).
Yen, H. H. et al. Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study. Intest. Res. 17, 54–62 (2019).
Kwak, M. S. et al. Emerging trends of inflammatory bowel disease in South Korea: a nationwide population-based study. J. Gastroenterol. Hepatol. 34, 1018–1026 (2019).
Organisation for Economic Co-operation and Development (2017) Pensions at a Glance 2017: OECD and G20 Indicators 122–123 (OECD, 2017).
Bar-Gil Shitrit, A. et al. Inflammatory bowel disease: an emergent disease among Ethiopian Jews migrating to Israel. Inflamm. Bowel Dis. 21, 631–635 (2015).
Archampong, T. N. & Nkrumah, K. N. Inflammatory bowel disease in Accra: what new trends. West. Afr. J. Med. 32, 40–44 (2013).
Khalifa, S. E., Mudawi, H. M. & Fedail, S. S. Presentation and management outcome of inflammatory bowel disease in Sudan. Trop. Gastroenterol. 26, 194–196 (2005).
Ng, W. K., Wong, S. H. & Ng, S. C. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest. Res. 14, 111–119 (2016).
Morita, N. et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J. Gastroenterol. 30 (Suppl. 8), 1–4 (1995).
Asakura, K. et al. Prevalence of ulcerative colitis and Crohn’s disease in Japan. J. Gastroenterol. 44, 659–665 (2009).
Murakami, Y. et al. Estimated prevalence of ulcerative colitis and Crohn’s disease in Japan in 2014: an analysis of a nationwide survey. J. Gastroenterol. 54, 1070–1077 (2019).
Yang, S. K. et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: a KASID study. Inflamm. Bowel Dis. 14, 542–549 (2008).
Ye, L., Cao, Q. & Cheng, J. Review of inflammatory bowel disease in China. ScientificWorldJournal 2013, 296470 (2013).
Regueiro, M. et al. Reduced unplanned care and disease activity and increased quality of life after patient enrollment in an inflammatory bowel disease medical home. Clin. Gastroenterol. Hepatol. 16, 1777–1785 (2018).
Flamant, M. & Roblin, X. Inflammatory bowel disease: towards a personalized medicine. Ther. Adv. Gastroenterol. 11, 1756283X17745029 (2018).
Cross, R. K. et al. A randomized controlled trial of TELEmedicine for patients with inflammatory bowel disease (TELE-IBD). Am. J. Gastroenterol. 114, 472–482 (2019).
Ananthakrishnan, A. N. et al. Use of narrative concepts in electronic health records to validate associations between genetic factors and response to treatment of inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 18, 1890–1892 (2020).
Stidham, R. W. et al. Performance of a deep learning model vs human reviewers in grading endoscopic disease severity of patients with ulcerative colitis. JAMA Netw. Open 2, e193963 (2019).
Waljee, A. K. et al. Development and validation of machine learning models in prediction of remission in patients with moderate to severe Crohn disease. JAMA Netw. Open 2, e193721 (2019).
Wu, F. et al. A new coronavirus associated with human respiratory disease in China. Nature 579, 265–269 (2020).
Brenner, E. J. et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology 159, 481–491 (2020).
World Bank. Health Nutrition and Population Statistics. https://databank.worldbank.org/source/health-nutrition-and-population-statistics (2020).
United Nations. United Nations World Economic Situation and Prospects. https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/WESP2019_BOOK-web.pdf (2019).
Acknowledgements
The authors thank F. Underwood and S. Coward for contributing to the article through literature searches, providing advice and graphic design. The authors have received funding from the Canadian Institutes for Health Research Operating Grant reference number PJT 162393.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks V. Ahuja, J. Burisch and M. Kappelman for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Global IBD Visualization of Epidemiology Studies: https://wpsites.ucalgary.ca/gilkaplan/ioibd-gives/
Kaplan Lab interactive maps: https://wpsites.ucalgary.ca/gilkaplan/
SECURE-IBD interactive map: https://wpsites.ucalgary.ca/gilkaplan/secure-ibd/
Video Abstract: https://youtu.be/6Cp7TAcc8XM
Rights and permissions
About this article
Cite this article
Kaplan, G.G., Windsor, J.W. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol 18, 56–66 (2021). https://doi.org/10.1038/s41575-020-00360-x
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41575-020-00360-x
This article is cited by
-
Review on advances in small molecule inhibitors on the treatment of inflammatory bowel disease
Molecular Biology Reports (2026)
-
Upadacitinib as rescue therapy for acute severe ulcerative colitis and severe Crohn’s disease – current knowledge and future directions
Pharmacological Reports (2026)
-
Abelmoschus Manihot flowers inhibit dysbiotic Enterobacteriaceae expansion by promoting Clostridium bolteae-mediated hypoxia restoration
Microbiome (2025)
-
Does benign paroxysmal positional vertigo impact the psychological state of patients? A case–control study
The Egyptian Journal of Otolaryngology (2025)
-
Association between avoidant/restrictive food intake disorder risk, dietary attitudes and behaviors among Chinese patients with inflammatory bowel disease: a cross-sectional study
BMC Gastroenterology (2025)