Abstract
Investigations into the microbiome in human diseases have exponentially increased over the past several decades, and the microbiome has been associated with nearly every malignancy, with research moving beyond associative studies to investigations into the microbiome as a causative factor in carcinogenesis. Pancreatic ductal adenocarcinoma (PDAC), the most common malignancy of the pancreas, is a major cause of worldwide cancer mortality owing to the lack of screening methods, late stage at diagnosis and poor response to currently available treatments. Microbiome–pancreatic cancer research has advanced, with research demonstrating that elements of the gut microbiome can modulate antitumour immune function, and microbial-derived products have been shown to influence response to chemotherapy. Additionally, microbiome-based ‘signatures’ have been identified that can act as biomarkers to predict PDAC and improve on currently available serum tumour markers. In this Review, how the microbiome mechanistically influences pancreatic tumours, with a focus on PDAC, and its clinical implications is described using ground-breaking historical and contemporary studies as a framework. The direction for future studies is also discussed.
Key points
-
Bacterial, viral and fungal microbiomes have been associated with pancreatic ductal adenocarcinoma.
-
Intrapancreatic as well as the gut microbiome both have a critical role in immunomodulation within the tumour microenvironment of pancreatic cancer.
-
The microbiome can influence the immunosuppressive tumour microenvironment of pancreatic cancer and facilitate activation of antitumour immune cells.
-
Microbial-derived metabolites and by-products have been shown to influence pancreatic carcinogenesis and treatment response.
-
Evidence exists that sequencing the bacterial microbiome from faeces, when combined with the clinically used serum marker CA19-9, can provide diagnostic accuracy for pancreatic cancer superior to CA19-9 alone.
-
Elements of the microbiome have been shown to influence the response of pancreatic ductal adenocarcinoma to systemic chemotherapy and immunotherapy either directly or indirectly.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Russell, W. An address on a characteristic organism of cancer. Br. Med. J. 2, 1356–1360 (1890).
Whipps, J. M., Lewis, K. & Cooke, R. C. in Fungi in Biological Control Systems (ed. Burge, M. N.) 161–187 (Manchester Univ. Press, 1988).
Huang, D. W., Sherman, B. T. & Lempicki, R. A. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 37, 1–13 (2009).
Di Bella, J. M., Bao, Y., Gloor, G. B., Burton, J. P. & Reid, G. High throughput sequencing methods and analysis for microbiome research. J. Microbiol. Methods 95, 401–414 (2013).
Staley, C. & Sadowsky, M. J. Practical considerations for sampling and data analysis in contemporary metagenomics-based environmental studies. J. Microbiol. Methods 154, 14–18 (2018).
Thomas, R. M. & Jobin, C. The microbiome and cancer: is the “oncobiome” mirage real? Trends Cancer 1, 24–35 (2015).
Rose, C., Parker, A., Jefferson, B. & Cartmell, E. The characterization of feces and urine: a review of the literature to inform advanced treatment technology. Crit. Rev. Environ. Sci. Technol. 45, 1827–1879 (2015).
Borges-Canha, M. et al. Role of colonic microbiota in colorectal carcinogenesis: a systematic review. Rev. Esp. Enferm. Dig. 107, 659–671 (2015).
Sobhani, I. et al. Microbial dysbiosis in colorectal cancer (CRC) patients. PLoS ONE 6, e16393 (2011).
Schwabe, R. F. & Jobin, C. The microbiome and cancer. Nat. Rev. Cancer 13, 800–812 (2013).
Rahib, L. et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 74, 2913–2921 (2014).
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 74, 12–49 (2024).
Cruz, M. S., Tintelnot, J. & Gagliani, N. Roles of microbiota in pancreatic cancer development and treatment. Gut Microbes 16, 2320280 (2024).
Da Silver Xavier, G. The cells of the islets of langerhans. J. Clin. Med. 7, 54 (2018).
Sedlack, A. J. H. et al. Update in the management of gastroenteropancreatic neuroendocrine tumors. Cancer 130, 3090–3105 (2024).
Zhang, C.-Y. et al. Investigating the causal relationship between gut microbiota and gastroenteropancreatic neuroendocrine neoplasms: a bidirectional Mendelian randomization study. Front. Microbiol. 15, 1420167 (2024).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Kurilshikov, A. et al. Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat. Genet. 53, 156–165 (2021).
Chen, Z., Wang, Z., Bao, H. & Ma, S. Gut microbiota and pancreatic cancer risk, and the mediating role of immune cells and inflammatory cytokines: a Mendelian randomization study. Front. Immunol. 15, 1408770 (2024).
Dorrestein, P. C., Mazmanian, S. K. & Knight, R. Finding the missing links among metabolites, microbes, and the host. Immunity 40, 824–832 (2014).
Nejman, D. et al. The human tumor microbiome is composed of tumor type-specific intracellular bacteria. Science 368, 973–980 (2020). A comprehensive profiling of the intratumoural microbiome of seven different tumour types, including PDAC, demonstrates the compositional differences between tumour microbiomes and that most bacteria are present intracellularly, specifically within tumour and immune cells.
Massironi, S. et al. Intratumor microbiome in neuroendocrine neoplasms: a new partner of tumor microenvironment? A pilot study. Cells 11, 692 (2022).
Underhill, D. M. & Iliev, I. D. The mycobiota: interactions between commensal fungi and the host immune system. Nat. Rev. Immunol. 14, 405–416 (2014).
Honkanen, J. et al. Fungal dysbiosis and intestinal inflammation in children with beta-cell autoimmunity. Front. Immunol. 11, 468 (2020).
Salamon, D. et al. Analysis of the gut mycobiome in adult patients with type 1 and type 2 diabetes using next-generation sequencing (NGS) with increased sensitivity-pilot study. Nutrients 13, 1066 (2021).
Steenblock, C. et al. Viral infiltration of pancreatic islets in patients with COVID-19. Nat. Commun. 12, 3534 (2021).
Dotta, F. et al. Coxsackie B4 virus infection of β cells and natural killer cell insulitis in recent-onset type 1 diabetic patients. Proc. Natl Acad. Sci. USA 104, 5115–5120 (2007).
Müller, J. A. et al. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat. Metab. 3, 149–165 (2021).
Isaacs, S. R. et al. Enteroviruses and risk of islet autoimmunity or type 1 diabetes: systematic review and meta-analysis of controlled observational studies detecting viral nucleic acids and proteins. Lancet Diabetes Endocrinol. 11, 578–592 (2023).
Hruban, R. H., Goggins, M., Parsons, J. & Kern, S. E. Progression model for pancreatic cancer. Clin. Cancer Res. 6, 2969–2972 (2000). Comprehensive review illustrating the model of progression of pancreatic cancer that is necessary for a general understanding of this disease.
Iacobuzio-Donahue, C. A., Velculescu, V. E., Wolfgang, C. L. & Hruban, R. H. Genetic basis of pancreas cancer development and progression: insights from whole-exome and whole-genome sequencing. Clin. Cancer Res. 18, 4257–4265 (2012).
Rawla, P., Sunkara, T. & Gaduputi, V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J. Oncol. 10, 10–27 (2019).
Jandhyala, S. M. et al. Altered intestinal microbiota in patients with chronic pancreatitis: implications in diabetes and metabolic abnormalities. Sci. Rep. 7, 43640 (2017).
Isaiah, A., Parambeth, J. C., Steiner, J. M., Lidbury, J. A. & Suchodolski, J. S. The fecal microbiome of dogs with exocrine pancreatic insufficiency. Anaerobe 45, 50–58 (2017).
Zhang, X. M. et al. Intestinal microbial community differs between acute pancreatitis patients and healthy volunteers. Biomed. Environ. Sci. 31, 81–86 (2018).
Hong, J. et al. Gut microbiome changes associated with chronic pancreatitis and pancreatic cancer: a systematic review and meta-analysis. Int. J. Surg. 110, 5781–5794 (2024).
Sonika, U. et al. Mechanism of increased intestinal permeability in acute pancreatitis: alteration in tight junction proteins. J. Clin. Gastroenterol. 51, 461–466 (2017).
Ammori, B. J. et al. Early increase in intestinal permeability in patients with severe acute pancreatitis: correlation with endotoxemia, organ failure, and mortality. J. Gastrointest. Surg. 3, 252–262 (1999).
Dougherty, M. W. & Jobin, C. Intestinal bacteria and colorectal cancer: etiology and treatment. Gut Microbes 15, 2185028 (2023).
Thomas, R. M. Microbial molecules, metabolites, and malignancy. Neoplasia 60, 101128 (2025).
Matthaei, H., Schulick, R. D., Hruban, R. H. & Maitra, A. Cystic precursors to invasive pancreatic cancer. Nat. Rev. Gastroenterol. Hepatol. 8, 141–150 (2011).
Basturk, O. et al. A revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am. J. Surg. Pathol. 39, 1730–1741 (2015).
Maker, A. V. et al. Cyst fluid biosignature to predict intraductal papillary mucinous neoplasms of the pancreas with high malignant potential. J. Am. Coll. Surg. 228, 721–729 (2019).
Matthaei, H. et al. miRNA biomarkers in cyst fluid augment the diagnosis and management of pancreatic cysts. Clin. Cancer Res. 18, 4713–4724 (2012).
Pust, M.-M. et al. Absence of a pancreatic microbiome in intraductal papillary mucinous neoplasm. Gut 73, 1131–1141 (2024).
Caporaso, J. G. et al. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Proc. Natl Acad. Sci. USA 108, 4516–4522 (2011).
Goodrich, J. K. et al. Conducting a microbiome study. Cell 158, 250–262 (2014). A critical manuscript outlining the necessary steps to design, carry out and analyse a microbiome study, regardless of hypothesis or disease type.
Li, S. et al. Pancreatic cyst fluid harbors a unique microbiome. Microbiome 5, 147 (2017).
Gaiser, R. A. et al. Enrichment of oral microbiota in early cystic precursors to invasive pancreatic cancer. Gut 68, 2186–2194 (2019).
Wang, B. et al. The roles and interactions of Porphyromonas gingivalis and fusobacterium nucleatum in oral and gastrointestinal carcinogenesis: a narrative review. Pathogens 13, 93 (2024).
Pushalkar, S. et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 8, 403–416 (2018).
Thomas, R. M. et al. Intestinal microbiota enhances pancreatic carcinogenesis in preclinical models. Carcinogenesis 39, 1068–1078 (2018).
Halimi, A. et al. Isolation of pancreatic microbiota from cystic precursors of pancreatic cancer with intracellular growth and DNA damaging properties. Gut Microbes 13, 1983101 (2021).
Hingorani, S. R. et al. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell 4, 437–450 (2003).
Hingorani, S. R. et al. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell 7, 469–483 (2005).
Hill, R. et al. PTEN loss accelerates KrasG12D-induced pancreatic cancer development. Cancer Res. 70, 7114–7124 (2010).
Saba, E. et al. Oral bacteria accelerate pancreatic cancer development in mice. Gut 73, 770–786 (2024).
Ma, H., Luo, W. & Gu, Y. Does oral microbiota have a close relationship with pancreatic cancer? a systematic review and meta-analysis. Ann. Surg. Oncol. 30, 8635–8641 (2023).
Storz, P. Acinar cell plasticity and development of pancreatic ductal adenocarcinoma. Nat. Rev. Gastroenterol. Hepatol. 14, 296–304 (2017).
Kleeff, J. et al. Pancreatic cancer. Nat. Rev. Dis. Primers 2, 16022 (2016).
McGuigan, A. et al. Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J. Gastroenterol. 24, 4846–4861 (2018).
Raderer, M. et al. Association between Helicobacter pylori infection and pancreatic cancer. Oncology 55, 16–19 (1998).
Stolzenberg-Solomon, R. Z. et al. Helicobacter pylori seropositivity as a risk factor for pancreatic cancer. J. Natl Cancer Inst. 93, 937–941 (2001).
Yu, G. et al. Seropositivity to Helicobacter pylori and risk of pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 22, 2416–2419 (2013).
Maisonneuve, P., Amar, S. & Lowenfels, A. B. Periodontal disease, edentulism, and pancreatic cancer: a meta-analysis. Ann. Oncol. 28, 985–995 (2017).
Cutler, C. W., Kalmar, J. R. & Genco, C. A. Pathogenic strategies of the oral anaerobe, Porphyromonas gingivalis. Trends Microbiol. 3, 45–51 (1995).
Ahn, J., Segers, S. & Hayes, R. B. Periodontal disease, Porphyromonas gingivalis serum antibody levels and orodigestive cancer mortality. Carcinogenesis 33, 1055–1058 (2012).
Michaud, D. S. et al. Plasma antibodies to oral bacteria and risk of pancreatic cancer in a large European prospective cohort study. Gut 62, 1764–1770 (2013).
Duan, D. et al. Advances in multi-omics integrated analysis methods based on the gut microbiome and their applications. Front. Microbiol. 15, 1509117 (2024).
Farrell, J. J. et al. Variations of oral microbiota are associated with pancreatic diseases including pancreatic cancer. Gut 61, 582–588 (2012). One of the earliest investigations demonstrating an association of a microbiota, in this case the salivary microbiota, with pancreatic cancer.
Ren, Z. et al. Gut microbial profile analysis by MiSeq sequencing of pancreatic carcinoma patients in China. Oncotarget 8, 95176–95191 (2017).
Chen, J., Zhao, K.-N. & Vitetta, L. Effects of intestinal microbial-elaborated butyrate on oncogenic signaling pathways. Nutrients 11, 1026 (2019).
Encarnação, J. C. et al. Butyrate, a dietary fiber derivative that improves irinotecan effect in colon cancer cells. J. Nutr. Biochem. 56, 183–192 (2018).
Zhu, X. et al. Microbial metabolite butyrate promotes anti-PD-1 antitumor efficacy by modulating T cell receptor signaling of cytotoxic CD8 T cell. Gut Microbes 15, 2249143 (2023).
Turner, B. G. et al. Diagnosis of pancreatic neoplasia with EUS and FNA: a report of accuracy. Gastrointest. Endosc. 71, 91–98 (2010).
Chen, G., Liu, S., Zhao, Y., Dai, M. & Zhang, T. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for pancreatic cancer: a meta-analysis. Pancreatology 13, 298–304 (2013).
Yao, D.-W., Qin, M.-Z., Jiang, H.-X. & Qin, S.-Y. Comparison of EUS−FNA and EUS−FNB for diagnosis of solid pancreatic mass lesions: a meta-analysis of prospective studies. Scand. J. Gastroenterol. 59, 972–979 (2024).
Geller, L. T. et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science 357, 1156–1160 (2017). This investigation demonstrates that resistance to the common pancreatic cancer chemotherapy gemcitabine might be secondary to the presence of intratumoural Gammaproteobacteria that possesses the more active form (‘long form’) of the bacterial enzyme cytidine deaminase.
Thomas, R. M. & Jobin, C. Microbiota in pancreatic health and disease: the next frontier in microbiome research. Nat. Rev. Gastroenterol. Hepatol. 17, 53–64 (2020).
Kohi, S. et al. Alterations in the duodenal fluid microbiome of patients with pancreatic cancer. Clin. Gastroenterol. Hepatol. 20, e196–e227 (2022).
Jackson, M. A. et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut 65, 749–756 (2016).
Aykut, B. et al. The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nature 574, 264–267 (2019).
Narunsky-Haziza, L. et al. Pan-cancer analyses reveal cancer-type-specific fungal ecologies and bacteriome interactions. Cell 185, 3789–3806.e17 (2022).
Alam, A. et al. Fungal mycobiome drives IL-33 secretion and type 2 immunity in pancreatic cancer. Cancer Cell 40, 153–167.e11 (2022).
Fletcher, A. A., Kelly, M. S., Eckhoff, A. M. & Allen, P. J. Revisiting the intrinsic mycobiome in pancreatic cancer. Nature 620, E1–E6 (2023).
Xu, F., Saxena, D., Pushalkar, S. & Miller, G. Reply to: revisiting the intrinsic mycobiome in pancreatic cancer. Nature 620, E7–E9 (2023).
Kartal, E. et al. A faecal microbiota signature with high specificity for pancreatic cancer. Gut 71, 1359–1372 (2022). This study demonstrates the feasibility of faecal microbiota testing to detect pancreatic cancer and, when the microbiome signature was combined with the currently available pancreatic cancer tumour marker CA19-9, an even higher diagnostic accuracy was reported.
Zhang, P. et al. Metagenomic analysis reveals altered gut virome and diagnostic potential in pancreatic cancer. J. Med. Virol. 96, e29809 (2024).
Atarashi, K. et al. Induction of colonic regulatory T cells by indigenous Clostridium species. Science 331, 337–341 (2011).
Nutsch, K. M. & Hsieh, C.-S. T cell tolerance and immunity to commensal bacteria. Curr. Opin. Immunol. 24, 385–391 (2012).
Zhu, Y.-H. et al. Immunosuppression, immune escape, and immunotherapy in pancreatic cancer: focused on the tumor microenvironment. Cell Oncol. 46, 17–48 (2023).
Ho, W. J., Jaffee, E. M. & Zheng, L. The tumour microenvironment in pancreatic cancer — clinical challenges and opportunities. Nat. Rev. Clin. Oncol. 17, 527–540 (2020).
Sethi, V. et al. Gut microbiota promotes tumor growth in mice by modulating immune response. Gastroenterology 155, 33–37.e6 (2018).
Yu, Q. et al. Intestinal microbiota modulates pancreatic carcinogenesis through intratumoral natural killer cells. Gut Microbes 14, 2112881 (2022).
Riquelme, E. et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell 178, 795–806.e12 (2019). Although pancreatic cancer survival is traditionally low, there are patients who are long-term survivors. This study reports that the tumour microbiome composition of short-term survivors is statistically different than long-term survivors through decreased α-diversity. This difference influences the host immune response and probably survival.
Turner, M. W. The role of mannose-binding lectin in health and disease. Mol. Immunol. 40, 423–429 (2003).
Garred, P., Larsen, F., Seyfarth, J., Fujita, R. & Madsen, H. O. Mannose-binding lectin and its genetic variants. Genes Immun. 7, 85–94 (2006).
Afshar-Kharghan, V. The role of the complement system in cancer. J. Clin. Invest. 127, 780–789 (2017).
Ikebe, M. et al. Lipopolysaccharide (LPS) increases the invasive ability of pancreatic cancer cells through the TLR4/MyD88 signaling pathway. J. Surg. Oncol. 100, 725–731 (2009).
Dai, Z.-L., Wu, G. & Zhu, W.-Y. Amino acid metabolism in intestinal bacteria: links between gut ecology and host health. Front. Biosci. 16, 1768–1786 (2011).
Lin, R., Liu, W., Piao, M. & Zhu, H. A review of the relationship between the gut microbiota and amino acid metabolism. Amino Acids 49, 2083–2090 (2017).
al-Waiz, M., Mikov, M., Mitchell, S. C. & Smith, R. L. The exogenous origin of trimethylamine in the mouse. Metab. Clin. Exp. 41, 135–136 (1992).
Mirji, G. et al. The microbiome-derived metabolite TMAO drives immune activation and boosts responses to immune checkpoint blockade in pancreatic cancer. Sci. Immunol. 7, eabn0704 (2022).
Heath-Pagliuso, S. et al. Activation of the Ah receptor by tryptophan and tryptophan metabolites. Biochemistry 37, 11508–11515 (1998).
Shinde, R. & McGaha, T. L. The aryl hydrocarbon receptor: connecting immunity to the microenvironment. Trends Immunol. 39, 1005–1020 (2018).
Xue, P., Fu, J. & Zhou, Y. The aryl hydrocarbon receptor and tumor immunity. Front. Immunol. 9, 286 (2018).
Hezaveh, K. et al. Tryptophan-derived microbial metabolites activate the aryl hydrocarbon receptor in tumor-associated macrophages to suppress anti-tumor immunity. Immunity 55, 324–340.e8 (2022).
Roager, H. M. & Licht, T. R. Microbial tryptophan catabolites in health and disease. Nat. Commun. 9, 3294 (2018).
Agrawal, R. & Natarajan, K. N. Oncogenic signaling pathways in pancreatic ductal adenocarcinoma. Adv. Cancer Res. 159, 251–283 (2023).
Yang, Q. et al. A review of gut microbiota-derived metabolites in tumor progression and cancer therapy. Adv. Sci. 10, e2207366 (2023).
D’Amico, D. et al. Impact of the natural compound urolithin A on health, disease, and aging. Trends Mol. Med. 27, 687–699 (2021).
Totiger, T. M. et al. Urolithin A, a novel natural compound to target PI3K/AKT/mTOR pathway in pancreatic cancer. Mol. Cancer Ther. 18, 301–311 (2019).
Morrison, D. J. & Preston, T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes 7, 189–200 (2016).
Corrêa-Oliveira, R., Fachi, J. L., Vieira, A., Sato, F. T. & Vinolo, M. A. R. Regulation of immune cell function by short-chain fatty acids. Clin. Transl. Immunol. 5, e73 (2016).
Bachem, A. et al. Microbiota-derived short-chain fatty acids promote the memory potential of antigen-activated CD8+ T cells. Immunity 51, 285–297.e5 (2019).
Coutza, C. et al. Systemic short chain fatty acids limit antitumor effect of CTLA-4 blockade in hosts with cancer. Nat. Commun. 11, 2165 (2020).
Nomura, M. et al. Association of short-chain fatty acids in the gut microbiome with clinical response to treatment with nivolumab or pembrolizumab in patients with solid cancer tumors. JAMA Netw. Open 3, e202895 (2020).
Ziemons, J. et al. Fecal levels of SCFA and BCFA during capecitabine in patients with metastatic or unresectable colorectal cancer. Clin. Exp. Med. 23, 3919–3933 (2023).
Sono, M. et al. Reduction of butyrate-producing bacteria in the gut microbiome of Japanese patients with pancreatic cancer. Pancreatology 24, 1031–1039 (2024).
Zhou, W. et al. The fecal microbiota of patients with pancreatic ductal adenocarcinoma and autoimmune pancreatitis characterized by metagenomic sequencing. J. Transl. Med. 19, 215 (2021).
Weir, T. L. et al. Stool microbiome and metabolome differences between colorectal cancer patients and healthy adults. PLoS ONE 8, e70803 (2013).
Wu, N. et al. Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microb. Ecol. 66, 462–470 (2013).
Mirzaei, R. et al. Role of microbiota-derived short-chain fatty acids in cancer development and prevention. Biomed. Pharmacother. 139, 111619 (2021).
Markowiak-Kopeć, P. & Śliżewska, K. The effect of probiotics on the production of short-chain fatty acids by human intestinal microbiome. Nutrients 12, 1107 (2020).
Yang, X. et al. Clostridium butyricum and its metabolite butyrate promote ferroptosis susceptibility in pancreatic ductal adenocarcinoma. Cell Oncol. 46, 1645–1658 (2023).
Irajizad, E. et al. A blood-based metabolomic signature predictive of risk for pancreatic cancer. Cell Rep. Med. 4, 101194 (2023).
Nagata, N. et al. Metagenomic identification of microbial signatures predicting pancreatic cancer from a multinational study. Gastroenterology 163, 222–238 (2022).
Wallace, B. D. et al. Alleviating cancer drug toxicity by inhibiting a bacterial enzyme. Science 330, 831–835 (2010).
de Castilhos, J. et al. Microbiome and pancreatic cancer: time to think about chemotherapy. Gut Microbes 16, 2374596 (2024).
Yang, W. et al. Intestinal microbiota-derived short-chain fatty acids regulation of immune cell IL-22 production and gut immunity. Nat. Commun. 11, 4457 (2020).
Ratajczak, W. et al. Immunomodulatory potential of gut microbiome-derived short-chain fatty acids (SCFAs). Acta Biochim. Pol. 66, 1–12 (2019).
Tintelnot, J. et al. Microbiota-derived 3-IAA influences chemotherapy efficacy in pancreatic cancer. Nature 615, 168–174 (2023).
Fu, S.-F. et al. Indole-3-acetic acid: a widespread physiological code in interactions of fungi with other organisms. Plant Signal. Behav. 10, e1048052 (2015).
Von Hoff, D. D. et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 369, 1691–1703 (2013).
Conroy, T. et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 364, 1817–1825 (2011).
Shiravand, Y. et al. Immune checkpoint inhibitors in cancer therapy. Curr. Oncol. 29, 3044–3060 (2022).
Vitiello, G. A., Cohen, D. J. & Miller, G. Harnessing the microbiome for pancreatic cancer immunotherapy. Trends Cancer 5, 670–676 (2019).
Sethi, V., Vitiello, G. A., Saxena, D., Miller, G. & Dudeja, V. The role of the microbiome in immunologic development and its implication for pancreatic cancer immunotherapy. Gastroenterology 156, 2097–2115.e2 (2019).
Rogers, S., Charles, A. & Thomas, R. M. The prospect of harnessing the microbiome to improve immunotherapeutic response in pancreatic cancer. Cancers 15, 5708 (2023).
Han, Z.-Y. et al. Probiotics functionalized with a gallium-polyphenol network modulate the intratumor microbiota and promote anti-tumor immune responses in pancreatic cancer. Nat. Commun. 15, 7096 (2024).
Ni, Y. et al. Distinct composition and metabolic functions of human gut microbiota are associated with cachexia in lung cancer patients. ISME J. 15, 3207–3220 (2021).
Yang-Jensen, S. K. et al. Intestinal host-microbe interactions fuel pulmonary inflammation in cigarette smoke exposed mice. Gut Microbes 17, 2519699 (2025).
Dilmore, A. H. et al. Medication use is associated with distinct microbial features in anxiety and depression. Mol. Pyschiatry 30, 2545–2557 (2025).
Szajewska, H. et al. Antibiotic-perturbed microbiota and the role of probiotics. Nat. Rev. Gastroenterol. Hepatol. 22, 155–172 (2025).
Mirzayi, C. et al. Reporting guidelines for human microbiome research: the STORMS checklist. Nat. Med. 27, 1885–1892 (2021).
Knight, R. et al. Best practices for analysing microbiomes. Nat. Rev. Microbiol. 16, 410–422 (2018).
Fierer, N. et al. Guidelines for preventing and reporting contamination in low-biomass microbiome studies. Nat. Microbiol. 10, 1570–1580 (2025).
Salter, S. J. et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 12, 87 (2014).
Caruso, V., Song, X., Asquith, M. & Karstens, L. Performance of microbiome sequence inference methods in environments with varying biomass. mSystems 4, e00163-18 (2019).
Eisenhofer, R. et al. Contamination in low microbial biomass microbiome studies: issues and recommendations. Trends Microbiol. 27, 105–117 (2019).
He, Y. et al. Regional variation limits applications of healthy gut microbiome reference ranges and disease models. Nat. Med. 24, 1532–1535 (2018).
Olsson, L. M. et al. Dynamics of the normal gut microbiota: a longitudinal one-year population study in Sweden. Cell Host Microbe 30, 726–739.e3 (2022).
Xu, Z., Malmer, D., Langille, M. G. I., Way, S. F. & Knight, R. Which is more important for classifying microbial communities: who’s there or what they can do? ISME J. 8, 2357–2359 (2014).
Abbas, S. et al. Bacteriophage therapy: a possible alternative therapy against antibiotic-resistant strains of Klebsiella pneumoniae. Front. Microbiol. 16, 1443430 (2025).
Yarahmadi, A. et al. Beyond antibiotics: exploring multifaceted approaches to combat bacterial resistance in the modern era: a comprehensive review. Front. Cell. Infect. Microbiol. 15, 1493915 (2025).
Li, Y., Li, X.-M., Duan, H.-Y., Yang, K. & Ye, J.-F. Advances and optimization strategies in bacteriophage therapy for treating inflammatory bowel disease. Front. Immunol. 15, 1398652 (2024).
Xiao, Y. et al. The role of bacteriophage in inflammatory bowel disease and its therapeutic potential. Crit. Rev. Microbiol. https://doi.org/10.1080/1040841X.2025.2492154 (2025).
Gilbert, J. A. et al. Clinical translation of microbiome research. Nat. Med. 31, 1099–1113 (2025).
Porcari, S. et al. International consensus statement on microbiome testing in clinical practice. Lancet Gastroenterol. Hepatol. 10, 154–167 (2025).
Tran, K. A. et al. Deep learning in cancer diagnosis, prognosis and treatment selection. Genome Med. 13, 152 (2021).
McCulloch, J. A. et al. Intestinal microbiota signatures of clinical response and immune-related adverse events in melanoma patients treated with anti-PD-1. Nat. Med. 28, 545–556 (2022).
Wu, G. et al. A core microbiome signature as an indicator of health. Cell 187, 6550–6565.e11 (2024).
Derosa, L. et al. Custom scoring based on ecological topology of gut microbiota associated with cancer immunotherapy outcome. Cell 187, 3373–3389.e16 (2024).
Lazaros, K. et al. Non-invasive biomarkers in the era of big data and machine learning. Sensors 25, 1396 (2025).
Arulvasan, W. et al. Optimized breath analysis: customized analytical methods and enhanced workflow for broader detection of VOCs. Metabolomics 21, 17 (2025).
Hutkins, R. et al. Classifying compounds as prebiotics — scientific perspectives and recommendations. Nat. Rev. Gastroenterol. Hepatol. 22, 54–70 (2025).
Armengaud, J. The dawn of the revolution that will allow us to precisely describe how microbiomes function. J. Proteom. 316, 105430 (2025).
Zaramela, L. S. et al. The sum is greater than the parts: exploiting microbial communities to achieve complex functions. Curr. Opin. Biotechnol. 67, 149–157 (2021).
Sharma, K. R., Colvis, C. M., Rodgers, G. P. & Sheeley, D. M. Illuminating the druggable genome: pathways to progress. Drug Discov. Today 29, 103805 (2024).
Villani, A. et al. A powerful machine learning approach to identify interactions of differentially abundant gut microbial subsets in patients with metastatic and non-metastatic pancreatic cancer. Gut Microbes 16, 2375483 (2024).
Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 37, 852–857 (2019).
Shalon, D. et al. Profiling the human intestinal environment under physiological conditions. Nature 617, 581–591 (2023).
Schmidt, F. et al. Noninvasive assessment of gut function using transcriptional recording sentinel cells. Science 376, eabm6038 (2022).
Author information
Authors and Affiliations
Contributions
R.M.T. wrote all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Vikas Dudeja, who co-reviewed with Tejeshwar Jain; Deepak Saxena; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinialTrials.gov: https://clinicaltrials.gov/
Glossary
- Abundance
-
Refers to the total amount of microorganisms in a particular sample. Also referred to as the microbial load, the abundance can be represented either as the absolute amount or as the relative abundance, which is the proportion of a particular organism or taxa to the total amount of investigated microorganisms.
- Bioinformatic pipelines
-
A series of data manipulations and workflow analysis to convert raw sequencing or other large biological data sets into an interpretable form such as tables or graphics.
- Commensal
-
In terms of microbiome research, commensal refers to organisms that live on and within the human body that benefit from the human host but provide no benefit or harm.
- Diversity
-
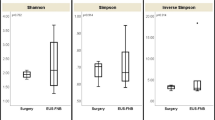
Refers to the number of different taxa within a specimen and can be reported as α-diversity, which refers to the number of different taxa within a particular specimen, or β-diversity, which refers to the similarity or dissimilarity between two different cohorts.
- Metabolomic
-
The study or analysis of small molecules or other metabolic processes derived from cellular physiology.
- Microbiome
-
A group of common microorganisms (bacteria, fungus, viruses or archaea) living in a particular environment and creating a unique community structure. Unique names have been given to microbiomes comprising specific microorganisms such as the mycobiome (fungi) or virome (viruses).
- Neoplasms
-
Any abnormal growth of cells that either do not possess the ability to spread elsewhere in the body (benign neoplasm) or do have such an ability (malignant neoplasm).
- Oncobiome
-
The field of research that is focused on the interplay between the human microbiome and cancer development.
- Pathobiont
-
In terms of microbiome research, pathobiont refers to microorganisms that live on and within the human body that can cause disease or harm to the host depending on genetic or environmental changes.
- Symbiotic
-
In terms of microbiome research, symbiotic refers to microorganisms that live on and within the human body in which both host and organisms benefit from the interaction.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thomas, R.M. Multifaceted effects of the microbiome in pancreatic cancer: from association to modulation. Nat Rev Gastroenterol Hepatol 22, 829–845 (2025). https://doi.org/10.1038/s41575-025-01119-y
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41575-025-01119-y