Abstract
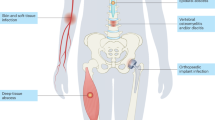
Invasive Staphylococcus aureus infections are common, causing high mortality, compounded by the propensity of the bacterium to develop drug resistance. S. aureus is an excellent case study of the potential for a bacterium to be commensal, colonizing, latent or disease-causing; these states defined by the interplay between S. aureus and host. This interplay is multidimensional and evolving, exemplified by the spread of S. aureus between humans and other animal reservoirs and the lack of success in vaccine development. In this Review, we examine recent advances in understanding the S. aureus–host interactions that lead to infections. We revisit the primary role of neutrophils in controlling infection, summarizing the discovery of new immune evasion molecules and the discovery of new functions ascribed to well-known virulence factors. We explore the intriguing intersection of bacterial and host metabolism, where crosstalk in both directions can influence immune responses and infection outcomes. This Review also assesses the surprising genomic plasticity of S. aureus, its dualism as a multi-mammalian species commensal and opportunistic pathogen and our developing understanding of the roles of other bacteria in shaping S. aureus colonization.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lowy, F. D. Staphylococcus aureus infections. N. Engl. J. Med. 339, 520–532 (1998).
Wertheim, H. F. et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 5, 751–762 (2005).
Williams, R. E. Healthy carriage of Staphylococcus aureus: its prevalence and importance. Bacteriol. Rev. 27, 56–71 (1963).
Krismer, B., Weidenmaier, C., Zipperer, A. & Peschel, A. The commensal lifestyle of Staphylococcus aureus and its interactions with the nasal microbiota. Nat. Rev. Microbiol. 15, 675–687 (2017). Excellent review on the nasal microbiome and the interaction with S. aureus.
Clarridge, J. E. III, Harrington, A. T., Roberts, M. C., Soge, O. O. & Maquelin, K. Impact of strain typing methods on assessment of relationship between paired nares and wound isolates of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 51, 224–231 (2013).
Raineri, E. J. M., Altulea, D. & van Dijl, J. M. Staphylococcal trafficking and infection-from ‘nose to gut’ and back. FEMS Microbiol. Rev. 46, fuab041 (2022).
Spaan, A. N., van Strijp, J. A. G. & Torres, V. J. Leukocidins: staphylococcal bi-component pore-forming toxins find their receptors. Nat. Rev. Microbiol. 15, 435–447 (2017). Comprehensive review of the staphylococcal leukocidins.
Thammavongsa, V., Kim, H. K., Missiakas, D. & Schneewind, O. Staphylococcal manipulation of host immune responses. Nat. Rev. Microbiol. 13, 529–543 (2015).
Montgomery, C. P., David, M. Z. & Daum, R. S. Host factors that contribute to recurrent staphylococcal skin infection. Curr. Opin. Infect. Dis. 28, 253–258 (2015).
Kallen, A. J. et al. Health care-associated invasive MRSA infections, 2005–2008. JAMA 304, 641–648 (2010).
Jansen, K. U., Girgenti, D. Q., Scully, I. L. & Anderson, A. S. Vaccine review: ‘Staphyloccocus aureus vaccines: problems and prospects’. Vaccine 31, 2723–2730 (2013).
Wollenberg, M. S. et al. Propionibacterium-produced coproporphyrin III induces Staphylococcus aureus aggregation and biofilm formation. mBio 5, e01286-14 (2014).
Costello, E. K. et al. Bacterial community variation in human body habitats across space and time. Science 326, 1694–1697 (2009).
Torres Salazar, B. O., Heilbronner, S., Peschel, A. & Krismer, B. Secondary metabolites governing microbiome interaction of Staphylococcal pathogens and commensals. Micro. Physiol. 31, 198–216 (2021).
Lister, J. L. & Horswill, A. R. Staphylococcus aureus biofilms: recent developments in biofilm dispersal. Front. Cell Infect. Microbiol. 4, 178 (2014).
Archer, N. K. et al. Staphylococcus aureus biofilms: properties, regulation, and roles in human disease. Virulence 2, 445–459 (2011).
Bhattacharya, M. et al. Staphylococcus aureus biofilms release leukocidins to elicit extracellular trap formation and evade neutrophil-mediated killing. Proc. Natl Acad. Sci. USA 115, 7416–7421 (2018).
Chambers, H. F. & Deleo, F. R. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat. Rev. Microbiol. 7, 629–641 (2009).
Turner, N. A. et al. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat. Rev. Microbiol. 17, 203–218 (2019).
Howden, B. P., Davies, J. K., Johnson, P. D., Stinear, T. P. & Grayson, M. L. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin. Microbiol. Rev. 23, 99–139 (2010).
Gao, W. et al. The RpoB H481Y rifampicin resistance mutation and an active stringent response reduce virulence and increase resistance to innate immune responses in Staphylococcus aureus. J. Infect. Dis. 207, 929–939 (2013).
Proctor, R. A. et al. Small colony variants: a pathogenic form of bacteria that facilitates persistent and recurrent infections. Nat. Rev. Microbiol. 4, 295–305 (2006).
Moller, A. G., Petit, R. A. III & Read, T. D. Species-scale genomic analysis of Staphylococcus aureus genes influencing phage host range and their relationships to virulence and antibiotic resistance genes. mSystems 7, e0108321 (2022).
Howden, B. P. et al. Evolution of multidrug resistance during Staphylococcus aureus infection involves mutation of the essential two component regulator WalKR. PLoS Pathog. 7, e1002359 (2011).
Mwangi, M. M. et al. Tracking the in vivo evolution of multidrug resistance in Staphylococcus aureus by whole-genome sequencing. Proc. Natl Acad. Sci. USA 104, 9451–9456 (2007).
Gao, W. et al. Large tandem chromosome expansions facilitate niche adaptation during persistent infection with drug-resistant Staphylococcus aureus. Microb. Genom. 1, e000026 (2015).
Panton, P. N. & Valentine, F. C. O. Staphylococcal toxin. Lancet 219, 506–508 (1932).
Cheung, G. Y. C., Bae, J. S. & Otto, M. Pathogenicity and virulence of Staphylococcus aureus. Virulence 12, 547–569 (2021).
Curnutte, J. T., Whitten, D. M. & Babior, B. M. Defective superoxide production by granulocytes from patients with chronic granulomatous disease. N. Engl. J. Med. 290, 593–597 (1974).
Spaan, A. N., Surewaard, B. G., Nijland, R. & van Strijp, J. A. Neutrophils versus Staphylococcus aureus: a biological tug of war. Annu. Rev. Microbiol. 67, 629–650 (2013).
Stapels, D. A. et al. Staphylococcus aureus secretes a unique class of neutrophil serine protease inhibitors. Proc. Natl Acad. Sci. USA 111, 13187–13192 (2014).
Kretschmer, D. et al. Staphylococcus aureus depends on eap proteins for preventing degradation of its phenol-soluble modulin toxins by neutrophil serine proteases. Front. Immunol. 12, 701093 (2021).
Stapels, D. A. et al. Staphylococcus aureus protects its immune-evasion proteins against degradation by neutrophil serine proteases. Cell Microbiol. 18, 536–545 (2016).
Ploscariu, N. T., de Jong, N. W. M., van Kessel, K. P. M., van Strijp, J. A. G. & Geisbrecht, B. V. Identification and structural characterization of a novel myeloperoxidase inhibitor from Staphylococcus delphini. Arch. Biochem. Biophys. 645, 1–11 (2018).
de Jong, N. W. M. et al. Immune evasion by a staphylococcal inhibitor of myeloperoxidase. Proc. Natl Acad. Sci. USA 114, 9439–9444 (2017).
Loffler, B. et al. Staphylococcus aureus Panton-Valentine leukocidin is a very potent cytotoxic factor for human neutrophils. PloS Pathog. 6, e1000715 (2010).
Vrieling, M. et al. Population analysis of Staphylococcus aureus reveals a cryptic, highly prevalent superantigen SelW that contributes to the pathogenesis of bacteremia. mBio 11, e02082-20 (2020).
Wilson, G. J. et al. A novel core genome-encoded superantigen contributes to lethality of community-associated MRSA necrotizing pneumonia. PloS Pathog. 7, e1002271 (2011).
Tuffs, S. W. et al. The Staphylococcus aureus superantigen SelX is a bifunctional toxin that inhibits neutrophil function. PloS Pathog. 13, e1006461 (2017).
Foster, T. J., Geoghegan, J. A., Ganesh, V. K. & Hook, M. Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus aureus. Nat. Rev. Microbiol. 12, 49–62 (2014).
Corrigan, R. M., Miajlovic, H. & Foster, T. J. Surface proteins that promote adherence of Staphylococcus aureus to human desquamated nasal epithelial cells. BMC Microbiol. 9, 22 (2009).
Cheng, A. G. et al. Genetic requirements for Staphylococcus aureus abscess formation and persistence in host tissues. FASEB J. 23, 3393–3404 (2009).
Askarian, F. et al. Serine-aspartate repeat protein D increases Staphylococcus aureus virulence and survival in blood. Infect. Immun. 85, e00559-16 (2017).
Zhang, Y. et al. Staphylococcus aureus SdrE captures complement factor H’s C-terminus via a novel ‘close, dock, lock and latch’ mechanism for complement evasion. Biochem. J. 474, 1619–1631 (2017).
Speziale, P. & Pietrocola, G. The multivalent role of fibronectin-binding proteins A and B (FnBPA and FnBPB) of Staphylococcus aureus in host infections. Front. Microbiol. 11, 2054 (2020).
Pietrocola, G. et al. Fibronectin-binding protein B (FnBPB) from Staphylococcus aureus protects against the antimicrobial activity of histones. J. Biol. Chem. 294, 3588–3602 (2019).
Thammavongsa, V., Missiakas, D. M. & Schneewind, O. Staphylococcus aureus degrades neutrophil extracellular traps to promote immune cell death. Science 342, 863–866 (2013).
Soh, K. Y., Loh, J. M. S. & Proft, T. Cell wall-anchored 5ʹ-nucleotidases in Gram-positive cocci. Mol. Microbiol. 113, 691–698 (2020).
Berends, E. T. M. et al. Staphylococcus aureus impairs the function of and kills human dendritic cells via the LukAB toxin. mBio 10, e01918-18 (2019).
Badarau, A., Trstenjak, N. & Nagy, E. Structure and function of the two-component cytotoxins of Staphylococcus aureus — learnings for designing novel therapeutics. Adv. Exp. Med. Biol. 966, 15–35 (2017).
Perelman, S. S. et al. Genetic variation of staphylococcal LukAB toxin determines receptor tropism. Nat. Microbiol. 6, 731–745 (2021).
Spaan, A. N. et al. The staphylococcal toxin Panton-Valentine leukocidin targets human C5a receptors. Cell Host Microbe 13, 584–594 (2013).
Haapasalo, K. et al. Staphylococcus aureus toxin LukSF dissociates from its membrane receptor target to enable renewed ligand sequestration. FASEB J. 33, 3807–3824 (2019).
Tromp, A. T. et al. Human CD45 is an F-component-specific receptor for the staphylococcal toxin Panton-Valentine leukocidin. Nat. Microbiol. 3, 708–717 (2018).
Knop, J. et al. Staphylococcus aureus infection in humanized mice: a new model to study pathogenicity associated with human immune response. J. Infect. Dis. 212, 435–444 (2015).
Prince, A., Wang, H., Kitur, K. & Parker, D. Humanized mice exhibit increased susceptibility to Staphylococcus aureus pneumonia. J. Infect. Dis. 215, 1386–1395 (2017).
Tseng, C. W. et al. Increased susceptibility of humanized NSG mice to Panton-Valentine leukocidin and Staphylococcus aureus skin infection. PLoS Pathog. 11, e1005292 (2015).
Muthukrishnan, G. et al. Humanized mice exhibit exacerbated abscess formation and osteolysis during the establishment of implant-associated Staphylococcus aureus osteomyelitis. Front. Immunol. 12, 651515 (2021).
Chow, S. H. et al. Targeting NLRP3 and staphylococcal pore-forming toxin receptors in human-induced pluripotent stem cell-derived macrophages. J. Leukoc. Biol. 108, 967–981 (2020).
Lees, J. A. & Bentley, S. D. Bacterial GWAS: not just gilding the lily. Nat. Rev. Microbiol. 14, 406 (2016).
Young, B. C. et al. Panton-Valentine leucocidin is the key determinant of Staphylococcus aureus pyomyositis in a bacterial GWAS. eLife 8, e42486 (2019). Statistical genomics study linking a S. aureus virulence factor to a clinical manifestation.
Koymans, K. J. et al. Staphylococcal superantigen-like protein 1 and 5 (SSL1 & SSL5) limit neutrophil chemotaxis and migration through MMP-inhibition. Int. J. Mol. Sci. 17, 1072 (2016).
Bestebroer, J. et al. Staphylococcal SSL5 inhibits leukocyte activation by chemokines and anaphylatoxins. Blood 113, 328–337 (2009).
Tang, A. et al. Staphylococcus aureus superantigen-like protein SSL1: a toxic protease. Pathogens 8, 2 (2019).
Koymans, K. J. et al. The TLR2 antagonist Staphylococcal superantigen-like protein 3 acts as a virulence factor to promote bacterial pathogenicity in vivo. J. Innate Immun. 9, 561–573 (2017).
Zhao, Y. et al. Staphylococcal superantigen-like protein 13 activates neutrophils via formyl peptide receptor 2. Cell Microbiol. 20, e12941 (2018).
Diebolder, C. A. et al. Complement is activated by IgG hexamers assembled at the cell surface. Science 343, 1260–1263 (2014).
Becker, S., Frankel, M. B., Schneewind, O. & Missiakas, D. Release of protein A from the cell wall of Staphylococcus aureus. Proc. Natl Acad. Sci. USA 111, 1574–1579 (2014).
O’Halloran, D. P., Wynne, K. & Geoghegan, J. A. Protein A is released into the Staphylococcus aureus culture supernatant with an unprocessed sorting signal. Infect. Immun. 83, 1598–1609 (2015).
Falugi, F., Kim, H. K., Missiakas, D. M. & Schneewind, O. Role of protein A in the evasion of host adaptive immune responses by Staphylococcus aureus. mBio 4, e00575-13 (2013).
Cruz, A. R. et al. Staphylococcal protein A inhibits complement activation by interfering with IgG hexamer formation. Proc. Natl Acad. Sci. USA 118, e2016772118 (2021).
Hong, X. et al. Staphylococcal protein A promotes colonization and immune evasion of the epidemic healthcare-associated MRSA ST239. Front. Microbiol. 7, 951 (2016).
Smith, E. J. et al. The immune evasion protein Sbi of Staphylococcus aureus occurs both extracellularly and anchored to the cell envelope by binding lipoteichoic acid. Mol. Microbiol. 83, 789–804 (2012).
Dunphy, R. W. et al. Staphylococcal complement evasion protein Sbi stabilises C3d dimers by inducing an N-terminal helix swap. Front. Immunol. 13, 892234 (2022).
Dasari, P. et al. The protease SplB of Staphylococcus aureus targets host complement components and inhibits complement-mediated bacterial opsonophagocytosis. J. Bacteriol. 204, e0018421 (2022).
Bhattacharya, M. et al. Leukocidins and the nuclease nuc prevent neutrophil-mediated killing of Staphylococcus aureus biofilms. Infect. Immun. 88, e00372-20 (2020).
Schilcher, K. & Horswill, A. R. Staphylococcal biofilm development: structure, regulation, and treatment strategies. Microbiol. Mol. Biol. Rev. 84, e00026-19 (2020). Comprehensive review of S. aureus biofilms.
Ricciardi, B. F. et al. Staphylococcus aureus evasion of host immunity in the setting of prosthetic joint infection: biofilm and beyond. Curr. Rev. Musculoskelet. Med. 11, 389–400 (2018).
Arciola, C. R., Campoccia, D. & Montanaro, L. Implant infections: adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 16, 397–409 (2018).
Heim, C. E., Vidlak, D. & Kielian, T. Interleukin-10 production by myeloid-derived suppressor cells contributes to bacterial persistence during Staphylococcus aureus orthopedic biofilm infection. J. Leukoc. Biol. 98, 1003–1013 (2015).
Heim, C. E. et al. IL-12 promotes myeloid-derived suppressor cell recruitment and bacterial persistence during Staphylococcus aureus orthopedic implant infection. J. Immunol. 194, 3861–3872 (2015).
Heim, C. E. et al. Myeloid-derived suppressor cells contribute to Staphylococcus aureus orthopedic biofilm infection. J. Immunol. 192, 3778–3792 (2014).
Heim, C. E., West, S. C., Ali, H. & Kielian, T. Heterogeneity of Ly6G(+) Ly6C(+) myeloid-derived suppressor cell infiltrates during Staphylococcus aureus biofilm infection. Infect. Immun. 86, e00684-18 (2018).
Yamada, K. J. et al. Monocyte metabolic reprogramming promotes pro-inflammatory activity and Staphylococcus aureus biofilm clearance. PLoS Pathog. 16, e1008354 (2020).
Gabrilovich, D. I. & Nagaraj, S. Myeloid-derived suppressor cells as regulators of the immune system. Nat. Rev. Immunol. 9, 162–174 (2009).
O’Neill, L. A., Kishton, R. J. & Rathmell, J. A guide to immunometabolism for immunologists. Nat. Rev. Immunol. 16, 553–565 (2016).
Tannahill, G. M. et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature 496, 238–242 (2013).
Lampropoulou, V. et al. Itaconate links inhibition of succinate dehydrogenase with macrophage metabolic remodeling and regulation of inflammation. Cell Metab. 24, 158–166 (2016).
Hooftman, A. et al. The immunomodulatory metabolite itaconate modifies NLRP3 and inhibits inflammasome activation. Cell Metab. 32, 468–478.e7 (2020).
Qin, W. et al. S-glycosylation-based cysteine profiling reveals regulation of glycolysis by itaconate. Nat. Chem. Biol. 15, 983–991 (2019).
Heim, C. E. et al. Lactate production by Staphylococcus aureus biofilm inhibits HDAC11 to reprogramme the host immune response during persistent infection. Nat. Microbiol. 5, 1271–1284 (2020). Sophisticated host–pathogen study using at-scale transposon mutagenesis to reveal the role mechanism of S. aureus lactate in regulation of IL-10 expression.
Tomlinson, K. L. & Riquelme, S. A. Host–bacteria metabolic crosstalk drives S. aureus biofilm. Microb. Cell 8, 106–107 (2021).
Tomlinson, K. L. et al. Staphylococcus aureus induces an itaconate-dominated immunometabolic response that drives biofilm formation. Nat. Commun. 12, 1399 (2021).
Michelucci, A. et al. Immune-responsive gene 1 protein links metabolism to immunity by catalyzing itaconic acid production. Proc. Natl Acad. Sci. USA 110, 7820–7825 (2013).
Arts, R. J. et al. Glutaminolysis and fumarate accumulation integrate immunometabolic and epigenetic programs in trained immunity. Cell Metab. 24, 807–819 (2016).
Chan, L. C. et al. Innate immune memory contributes to host defense against recurrent skin and skin structure infections caused by methicillin-resistant Staphylococcus aureus. Infect. Immun. 85, e00876-16 (2017).
Chan, L. C. et al. Protective immunity in recurrent Staphylococcus aureus infection reflects localized immune signatures and macrophage-conferred memory. Proc. Natl Acad. Sci. USA 115, E11111–E11119 (2018).
Acker, K. P. et al. Strains of Staphylococcus aureus that colonize and infect skin harbor mutations in metabolic genes. iScience 19, 281–290 (2019).
Wong Fok Lung, T. et al. Staphylococcus aureus small colony variants impair host immunity by activating host cell glycolysis and inducing necroptosis. Nat. Microbiol. 5, 141–153 (2020).
Proctor, R. A., van Langevelde, P., Kristjansson, M., Maslow, J. N. & Arbeit, R. D. Persistent and relapsing infections associated with small-colony variants of Staphylococcus aureus. Clin. Infect. Dis. 20, 95–102 (1995).
Kriegeskorte, A. et al. Staphylococcus aureus small colony variants show common metabolic features in central metabolism irrespective of the underlying auxotrophism. Front. Cell Infect. Microbiol. 4, 141 (2014).
Gabryszewski, S. J. et al. Metabolic adaptation in methicillin-resistant Staphylococcus aureus pneumonia. Am. J. Respir. Cell Mol. Biol. 61, 185–197 (2019).
Guerillot, R. et al. Unstable chromosome rearrangements in Staphylococcus aureus cause phenotype switching associated with persistent infections. Proc. Natl Acad. Sci. USA 116, 20135–20140 (2019). Identification of a reversible genome rearrangement contributing to the SCV phenotype in S. aureus.
Richardson, E. J. et al. Gene exchange drives the ecological success of a multi-host bacterial pathogen. Nat. Ecol. Evol. 2, 1468–1478 (2018). Excellent demonstration of bacterial population genomics to reveal the extent to which humans are shaping the evolution of S. aureus and exchange between different animal hosts.
Price, L. B. et al. Staphylococcus aureus CC398: host adaptation and emergence of methicillin resistance in livestock. mBio 3, e00305-11 (2012).
Hau, S. J., Sun, J., Davies, P. R., Frana, T. S. & Nicholson, T. L. Comparative prevalence of immune evasion complex genes associated with beta-hemolysin converting bacteriophages in MRSA ST5 isolates from swine, swine facilities, humans with swine contact, and humans with no swine contact. PLoS ONE 10, e0142832 (2015).
Sahibzada, S. et al. Transmission of highly virulent community-associated MRSA ST93 and livestock-associated MRSA ST398 between humans and pigs in Australia. Sci. Rep. 7, 5273 (2017).
Spoor, L. E. et al. Livestock origin for a human pandemic clone of community-associated methicillin-resistant Staphylococcus aureus. mBio 4, e00356-13 (2013).
Larsen, J. et al. Emergence of methicillin resistance predates the clinical use of antibiotics. Nature 602, 135–141 (2022). Large-scale genomic study identifying an animal source for antimicrobial-resistant S. aureus in humans.
Hallatschek, O., Hersen, P., Ramanathan, S. & Nelson, D. R. Genetic drift at expanding frontiers promotes gene segregation. Proc. Natl Acad. Sci. USA 104, 19926–19930 (2007).
Nei, M. Selectionism and neutralism in molecular evolution. Mol. Biol. Evol. 22, 2318–2342 (2005).
McVicker, G. et al. Clonal expansion during Staphylococcus aureus infection dynamics reveals the effect of antibiotic intervention. PLoS Pathog. 10, e1003959 (2014).
Didelot, X., Walker, A. S., Peto, T. E., Crook, D. W. & Wilson, D. J. Within-host evolution of bacterial pathogens. Nat. Rev. Microbiol. 14, 150–162 (2016).
Sheppard, S. K., Guttman, D. S. & Fitzgerald, J. R. Population genomics of bacterial host adaptation. Nat. Rev. Genet. 19, 549–565 (2018). Comprehensive review of bacterial host species adaptation.
Guinane, C. M. et al. Evolutionary genomics of Staphylococcus aureus reveals insights into the origin and molecular basis of ruminant host adaptation. Genome Biol. Evol. 2, 454–466 (2010).
Viana, D. et al. A single natural nucleotide mutation alters bacterial pathogen host tropism. Nat. Genet. 47, 361–366 (2015).
Bacigalupe, R., Tormo-Mas, M. A., Penades, J. R. & Fitzgerald, J. R. A multihost bacterial pathogen overcomes continuous population bottlenecks to adapt to new host species. Sci. Adv. 5, eaax0063 (2019). Experimental study demonstrating the capacity of S. aureus to acquire beneficial mutations alleviating evolutionary bottlenecks and enabling its adaptation to different hosts.
Zhou, W. et al. WGS analysis of ST9-MRSA-XII isolates from live pigs in China provides insights into transmission among porcine, human and bovine hosts. J. Antimicrob. Chemother. 73, 2652–2661 (2018).
Haag, A. F., Fitzgerald, J. R. & Penades, J. R. Staphylococcus aureus in animals. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.GPP3-0060-2019 (2019).
Vrieling, M. et al. Bovine Staphylococcus aureus secretes the leukocidin LukMF’ to kill migrating neutrophils through CCR1. mBio 6, e00335 (2015).
Matuszewska, M., Murray, G. G. R., Harrison, E. M., Holmes, M. A. & Weinert, L. A. The evolutionary genomics of host specificity in Staphylococcus aureus. Trends Microbiol. 28, 465–477 (2020).
Park, S. & Ronholm, J. Staphylococcus aureus in agriculture: lessons in evolution from a multispecies pathogen. Clin. Microbiol. Rev. 34, e00182-20 (2021).
de Jong, N. W. M. et al. Identification of a staphylococcal complement inhibitor with broad host specificity in equid Staphylococcus aureus strains. J. Biol. Chem. 293, 4468–4477 (2018).
Petit, R. A. III & Read, T. D. Staphylococcus aureus viewed from the perspective of 40,000+ genomes. Peer J. 6, e5261 (2018).
Lindsay, J. A. Genomic variation and evolution of Staphylococcus aureus. Int. J. Med. Microbiol. 300, 98–103 (2010).
Malachowa, N. & DeLeo, F. R. Mobile genetic elements of Staphylococcus aureus. Cell Mol. Life Sci. 67, 3057–3071 (2010).
Golubchik, T. et al. Within-host evolution of Staphylococcus aureus during asymptomatic carriage. PLoS ONE 8, e61319 (2013).
Everitt, R. G. et al. Mobile elements drive recombination hotspots in the core genome of Staphylococcus aureus. Nat. Commun. 5, 3956 (2014).
Prunier, A.-L. et al. High rate of macrolide resistance in Staphylococcus aureus strains from patients with cystic fibrosis reveals high proportions of hypermutable strains. J. Infect. Dis. 187, 1709–1716 (2003).
Giulieri, S. G. et al. Niche-specific genome degradation and convergent evolution shaping Staphylococcus aureus adaptation during severe infections. eLife 11, e77195 (2022). Population genomics conducted on a very large clinical cohort to reveal with unprecedented resolution the bacterial genome-wide changes that are associated with the transition from colonizing to invasive S. aureus infections.
Giulieri, S. G. et al. Genomic exploration of sequential clinical isolates reveals a distinctive molecular signature of persistent Staphylococcus aureus bacteraemia. Genome Med. 10, 65 (2018).
Klemm, E. J. et al. Emergence of host-adapted Salmonella Enteritidis through rapid evolution in an immunocompromised host. Nat. Microbiol. 1, 15023 (2016).
Batut, B., Knibbe, C., Marais, G. & Daubin, V. Reductive genome evolution at both ends of the bacterial population size spectrum. Nat. Rev. Microbiol. 12, 841–850 (2014).
Hall, M. D. et al. Improved characterisation of MRSA transmission using within-host bacterial sequence diversity. eLife 8, 46402 (2019).
Long, D. R. et al. Polyclonality, shared strains, and convergent evolution in chronic CF S. aureus airway infection. Am. J. Respir. Crit. Care Med. 203, 1127–1137 (2021).
Young, B. C. et al. Evolutionary dynamics of Staphylococcus aureus during progression from carriage to disease. Proc. Natl Acad. Sci. USA 109, 4550–4555 (2012).
Young, B. C. et al. Severe infections emerge from commensal bacteria by adaptive evolution. eLife 6, e30637 (2017).
Altman, D. R. et al. Genome plasticity of agr-defective Staphylococcus aureus during clinical infection. Infect. Immun. 86, e00331-18 (2018).
Das, S. et al. Natural mutations in a Staphylococcus aureus virulence regulator attenuate cytotoxicity but permit bacteremia and abscess formation. Proc. Natl Acad. Sci. USA 113, E3101–E3110 (2016).
Paudel, A., Panthee, S., Hamamoto, H., Grunert, T. & Sekimizu, K. YjbH regulates virulence genes expression and oxidative stress resistance in Staphylococcus aureus. Virulence 12, 470–480 (2021).
Jousselin, A., Kelley, W. L., Barras, C., Lew, D. P. & Renzoni, A. The Staphylococcus aureus Thiol/oxidative stress global regulator Spx controls trfA, a gene implicated in cell wall antibiotic resistance. Antimicrob. Agents Chemother. 57, 3283–3292 (2013).
Lopatkin, A. J. et al. Clinically relevant mutations in core metabolic genes confer antibiotic resistance. Science 371, eaba0862 (2021).
Elgrail, M. M. et al. Convergent evolution of antibiotic tolerance in patients with persistent methicillin-resistant Staphylococcus aureus bacteremia. Infect. Immun. 90, e0000122 (2022).
Giulieri, S. G. et al. Comprehensive genomic investigation of adaptive mutations driving the low-level oxacillin resistance phenotype in Staphylococcus aureus. mBio 11, e02882-20 (2020).
Howden, B. P., Johnson, P. D., Ward, P. B., Stinear, T. P. & Davies, J. K. Isolates with low-level vancomycin resistance associated with persistent methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob. Agents Chemother. 50, 3039–3047 (2006).
Loss, G. et al. Staphylococcus aureus small colony variants (SCVs): news from a chronic prosthetic joint infection. Front. Cell Infect. Microbiol. 9, 363 (2019).
Bär, J. et al. Quantification of within-patient Staphylococcus aureus phenotypic heterogeneity as a proxy for presence of persisters across clinical presentations. Clin. Microbiol. Infect. 28, 1022.e1–1022.e7 (2022).
Laabei, M. et al. Evolutionary trade-offs underlie the multi-faceted virulence of Staphylococcus aureus. PLoS Biol. 13, e1002229 (2015).
Xiong, Y. Q. et al. Phenotypic and genotypic characteristics of persistent methicillin-resistant Staphylococcus aureus bacteremia in vitro and in an experimental endocarditis model. J. Infect. Dis. 199, 201–208 (2009).
Scott, W. K. et al. Human genetic variation in GLS2 is associated with development of complicated Staphylococcus aureus bacteremia. PLoS Genet. 14, e1007667 (2018).
Spaan, A. N. et al. Human OTULIN haploinsufficiency impairs cell-intrinsic immunity to staphylococcal alpha-toxin. Science 376, eabm6380 (2022). This is the first evidence of a human heterozygous gene deficiency predisposing patients to severe S. aureus infection.
Chang, Y. L. et al. Human DNA methylation signatures differentiate persistent from resolving MRSA bacteremia. Proc. Natl Acad. Sci. USA 118, e2000663118 (2021).
Ford, C. A., Hurford, I. M. & Cassat, J. E. Antivirulence strategies for the treatment of Staphylococcus aureus infections: a mini review. Front. Microbiol. 11, 632706 (2020).
Francois, B. et al. Safety and tolerability of a single administration of AR-301, a human monoclonal antibody, in ICU patients with severe pneumonia caused by Staphylococcus aureus: first-in-human trial. Intensive Care Med. 44, 1787–1796 (2018).
Magyarics, Z. et al. Randomized, double-blind, placebo-controlled, single-ascending-dose study of the penetration of a monoclonal antibody combination (ASN100) targeting Staphylococcus aureus cytotoxins in the lung epithelial lining fluid of healthy volunteers. Antimicrob. Agents Chemother. 63, e00350-19 (2019).
Chan, R. et al. Identification of biologic agents to neutralize the bicomponent leukocidins of Staphylococcus aureus. Sci. Transl Med. 11, eaat0882 (2019).
Mansson, M. et al. Inhibition of virulence gene expression in Staphylococcus aureus by novel depsipeptides from a marine photobacterium. Mar. Drugs 9, 2537–2552 (2011).
Gao, P., Davies, J. & Kao, R. Y. T. Dehydrosqualene desaturase as a novel target for anti-virulence therapy against Staphylococcus aureus. mBio 8, e01224-17 (2017).
Chen, X., Schneewind, O. & Missiakas, D. Engineered human antibodies for the opsonization and killing of Staphylococcus aureus. Proc. Natl Acad. Sci. USA 119, e2114478119 (2022).
Miller, L. S., Fowler, V. G., Shukla, S. K., Rose, W. E. & Proctor, R. A. Development of a vaccine against Staphylococcus aureus invasive infections: evidence based on human immunity, genetics and bacterial evasion mechanisms. FEMS Microbiol. Rev. 44, 123–153 (2020).
Tsai, C. M. et al. Non-protective immune imprint underlies failure of Staphylococcus aureus IsdB vaccine. Cell Host Microbe 30, 1163–1172 (2022).
Nakatsuji, T. et al. Development of a human skin commensal microbe for bacteriotherapy of atopic dermatitis and use in a phase 1 randomized clinical trial. Nat. Med. 27, 700–709 (2021). Clinical study of bacteriotherapy highlighting that the inhibition of PSM production by commensal S. hominis decreases S. aureus colonization in atopic dermatitis patients.
Liu, Y. et al. Skin microbiota analysis-inspired development of novel anti-infectives. Microbiome 8, 85 (2020).
Piewngam, P. & Otto, M. Probiotics to prevent Staphylococcus aureus disease? Gut Microbes 11, 94–101 (2020).
Olagnier, D. et al. SARS-CoV2-mediated suppression of NRF2-signaling reveals potent antiviral and anti-inflammatory activity of 4-octyl-itaconate and dimethyl fumarate. Nat. Commun. 11, 4938 (2020).
Horn, C. M. & Kielian, T. Crosstalk between Staphylococcus aureus and innate immunity: focus on immunometabolism. Front. Immunol. 11, 621750 (2020).
Prince, A. & Wong Fok Lung, T. Consequences of metabolic interactions during Staphylococcus aureus infection. Toxins 12, 581 (2020).
Thurlow, L. R. et al. Staphylococcus aureus biofilms prevent macrophage phagocytosis and attenuate inflammation in vivo. J. Immunol. 186, 6585–6596 (2011).
Pleasance, E. et al. Whole genome and transcriptome analysis enhances precision cancer treatment options. Ann. Oncol. 33, 939–949 (2022).
Recker, M. et al. Clonal differences in Staphylococcus aureus bacteraemia-associated mortality. Nat. Microbiol. 2, 1381–1388 (2017).
Young, B. C. et al. Antimicrobial resistance determinants are associated with Staphylococcus aureus bacteraemia and adaptation to the healthcare environment: a bacterial genome-wide association study. Microb. Genom. 7, 000700 (2021).
Lilje, B. et al. Whole-genome sequencing of bloodstream Staphylococcus aureus isolates does not distinguish bacteraemia from endocarditis. Microb. Genom. https://doi.org/10.1099/mgen.0.000138 (2017).
Denamur, E. et al. Genome wide association study of Escherichia coli bloodstream infection isolates identifies genetic determinants for the portal of entry but not fatal outcome. PLoS Genet. 18, e1010112 (2022).
Wozniak, J. M. et al. Mortality risk profiling of Staphylococcus aureus bacteremia by multi-omic serum analysis reveals early predictive and pathogenic signatures. Cell 182, 1311–1327 (2020).
Acknowledgements
This work was supported by the National Health and Medical Research Council Australia through Investigator Grants to B.P.H. (GNT1196103) and T.P.S. (GNT1194325).
Author information
Authors and Affiliations
Contributions
B.P.H., T.P.S., S.G.G., S.L.B., L.K.S., J.Y.H.L., A.H., I.R.M. and T.W.F.L. researched data for the article. B.P.H., T.P.S., S.G.G., S.L.B., J.Y.H.L., A.H., I.R.M. and T.W.F.L. substantially contributed to discussion of content. B.P.H. and T.P.S. led the writing of the article with contributions from S.G.G., J.Y.H.L., A.H., I.R.M. and T.W.F.L. B.P.H., T.P.S., S.G.G., L.K.S., A.H., I.R.M. and T.W.F.L. reviewed and edited the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Jos van Strijp, Timothy Foster and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Accessory genome
-
Genes usually associated with mobile genetic elements that are present in only a subset of S. aureus strains. The accessory genome is one cause of variability in strain behaviour.
- Biofilms
-
A sessile microbial community usually enclosed by a protective extracellular matrix and attached to a surface or other cells.
- Bottlenecks
-
When a population (for example, bacterial population) is significantly reduced in size, limiting genetic diversity.
- Carbon catabolite repression
-
(CCR). A bacterial global regulatory process that results in the selective use of substrates from a mixture of carbon sources.
- Chronic granulomatous diseases
-
Rare X-linked recessive inherited immune deficiencies caused by defects in the enzyme, NADPH oxidase resulting in phagocytic dysfunction.
- Colonization
-
The presence of S. aureus on a body site such as the skin, gut or anterior nares, without causing disease.
- Core genome
-
Represents genes that are present in all S. aureus strains.
- Efferocytosis
-
A process of phagocytic engulfment of dead or dying cells.
- Evasion
-
Strategies used by bacteria to evade killing by the immune system.
- Genetic drift
-
A change in the frequency of an existing genetic variant in a population owing to random chance.
- Genome-wide association studies
-
The use of statistical genomics methods to identify the genetic variants linked to a particular phenotype.
- Insertion sequences
-
A short segment of DNA that can move within the S. aureus chromosome as a simple transposable element and contribute to bacterial adaptation.
- Invasion
-
The ability of a bacterial pathogen to spread to other locations in the host by invading host cells, such as the transition from the anterior nares (colonization) to the bloodstream (invasion).
- Leukotoxins
-
Toxin proteins that penetrate lipid bilayers to form pores.
- Lipopolysaccharide
-
Important outer membrane component of Gram-negative bacterial cell walls that acts as an endotoxin.
- Machine learning
-
The application of computer systems using statistical models and algorithms to draw conclusions from data.
- Microbial surface components recognizing adhesive matrix molecules
-
(MSCRAMMs). Adhesin proteins that are important in the initial binding of S. aureus to host tissues.
- Mobile genetic elements
-
Sequences of genetic material that can change places in the S. aureus chromosome or move between bacterial chromosomes.
- Persistence
-
Broadly refers to the ability of bacterial cells, including S. aureus, to cause persistent infection, despite the activity of the immune system or antibiotic therapy.
- Pyomyositis
-
Deep infection in the skeletal muscles, usually associated with abscess formation.
- Recurrent
-
The propensity for S. aureus infection to recur after initial successful therapy through surgery and/or antibiotics.
- Small colony variant
-
(SCV). A slow-growing (small colony) population of S. aureus that is associated with persistent and recurrent infections.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Howden, B.P., Giulieri, S.G., Wong Fok Lung, T. et al. Staphylococcus aureus host interactions and adaptation. Nat Rev Microbiol 21, 380–395 (2023). https://doi.org/10.1038/s41579-023-00852-y
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41579-023-00852-y
This article is cited by
-
Methicillin-resistant and susceptible Staphylococcus aureus: tolerance, immune evasion and treatment
Nature Reviews Microbiology (2026)
-
MXene-incorporated interconnected porous heterostructure for Staphylococcus aureus capture and surface enhanced Raman scattering analysis
Microchimica Acta (2026)
-
Glutathione reductase modulates endogenous oxidative stress and affects growth and virulence in Avibacterium paragallinarum
Veterinary Research (2025)
-
Glucose-induced active lysogeny of prophage ΦSa3XN promotes Staphylococcus aureus virulence
Virology Journal (2025)
-
Ultrahigh-throughput screening of heterogeneous vancomycin-intermediate Staphylococcus aureus based on fluorescence-activated droplet sorting
BMC Medicine (2025)