Abstract
The timely and rational institution of therapy is a key step towards reducing the global burden of chronic kidney disease (CKD). CKD is a heterogeneous entity with varied aetiologies and diverse trajectories, which include risk of kidney failure but also cardiovascular events and death. Developments in the past decade include substantial progress in CKD risk prediction, driven in part by the accumulation of electronic health records data. In addition, large randomized clinical trials have demonstrated the effectiveness of sodium–glucose co-transporter 2 inhibitors, glucagon-like peptide 1 receptor agonists and mineralocorticoid receptor antagonists in reducing adverse events in CKD, greatly expanding the options for effective therapy. Alongside angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, these classes of medication have been proposed to be the four pillars of CKD pharmacotherapy. However, all of these drug classes are underutilized, even in individuals at high risk. Leveraging prognostic estimates to guide therapy could help clinicians to prescribe CKD-related therapies to those who are most likely to benefit from their use. Risk-based CKD management thus aligns patient risk and care, allowing the prioritization of absolute benefit in determining therapeutic selection and timing. Here, we discuss CKD prognosis tools, evidence-based management and prognosis-guided therapies.
Key points
-
Widely validated risk tools can quantify the individual absolute risk of chronic kidney disease (CKD) progression, kidney failure, cardiovascular disease and death.
-
Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), sodium–glucose co-transporter 2 (SGLT2) inhibitors, glucagon-like peptide 1 receptor agonists (GLP1RAs) and mineralocorticoid receptor antagonists (MRAs) are highly effective and safe medicines that reduce CKD progression, cardiovascular events and mortality. Although underutilized, these medications are increasingly recognized as the pillars supporting CKD therapy.
-
Combination therapy offers kidney, cardiovascular and overall survival benefits, along with safety advantages.
-
Risk-based CKD care aligns treatment intensity to patient risk and considers medication selection and timing. The largest absolute benefit is expected in patients with the highest risk of adverse outcomes.
-
For people at the highest risk, clinicians should consider initiation of SGLT2 inhibitors, GLP1RAs, ACE inhibitors or ARBs, and MRAs in an accelerated fashion to achieve the largest absolute risk reductions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395, 709–733 (2020).
2023 USRDS annual data report: epidemiology of kidney disease in the United States. United States Renal Data System https://adr.usrds.org/2023 (2023).
Foreman, K. J. et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet 392, 2052–2090 (2018).
Alfego, D. et al. Chronic kidney disease testing among at-risk adults in the U.S. remains low: real-world evidence from a national laboratory database. Diabetes Care 44, 2025–2032 (2021).
Stempniewicz, N. et al. Chronic kidney disease testing among primary care patients with type 2 diabetes across 24 U.S. health care organizations. Diabetes Care 44, 2000–2009 (2021).
Chu, C. D. et al. Estimated prevalence and testing for albuminuria in US adults at risk for chronic kidney disease. JAMA Netw. Open. 6, e2326230 (2023).
Shin, J.-I. et al. Albuminuria testing in hypertension and diabetes: an individual-participant data meta-analysis in a global consortium. Hypertension 78, 1042–1052 (2021).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 105, S117–S314 (2024).
Writing Group for the CKD Prognosis Consortium. Estimated glomerular filtration rate, albuminuria, and adverse outcomes: an individual-participant data meta-analysis. JAMA 330, 1266–1277 (2023).
Levey, A. S. et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 80, 17–28 (2011).
Potok, O. A. et al. Patients’, nephrologists,’ and predicted estimations of ESKD risk compared with 2-year incidence of ESKD. Clin. J. Am. Soc. Nephrol. 14, 206–212 (2019).
Grams Morgan, E. et al. Kidney-failure risk projection for the living kidney-donor candidate. N. Engl. J. Med. 374, 411–421 (2016).
National Institute for Health and Care Excellence (NICE). Chronic Kidney Disease: Assessment and Management (2021).
Tangri, N. et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA 305, 1553–1559 (2011).
Tangri, N. et al. Multinational assessment of accuracy of equations for predicting risk of kidney failure: a meta-analysis. JAMA 315, 164–174 (2016).
Grams, M. E. et al. Proteins associated with risk of kidney function decline in the general population. J. Am. Soc. Nephrol. 32, 2291–2302 (2021).
Naranjo, F. S. et al. Estimating kidney failure risk using electronic medical records. Kidney360 2, 415–424 (2021).
Grams, M. E. et al. The Kidney Failure Risk Equation: evaluation of novel input variables including eGFR estimated using the CKD-EPI 2021 equation in 59 cohorts. J. Am. Soc. Nephrol. 34, 482–494 (2023).
Neuen, B. L. et al. Timing of cardio-kidney protection with SGLT2 inhibitors: insights from four large-scale placebo-controlled outcome trials. Circulation 150, 343–345 (2024).
Levey, A. S. et al. GFR decline as an end point for clinical trials in CKD: a scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am. J. Kidney Dis. 64, 821–835 (2014).
Levey, A. S. et al. Change in albuminuria and GFR as end points for clinical trials in early stages of CKD: a scientific workshop sponsored by the National Kidney Foundation in collaboration with the US Food and Drug Administration and European Medicines Agency. Am. J. Kidney Dis. 75, 84–104 (2020).
Grams, M. E. et al. Development and validation of prediction models of adverse kidney outcomes in the population with and without diabetes. Diabetes Care 45, 2055–2063 (2022).
Ndumele, C. E. et al. Cardiovascular–kidney–metabolic health: a presidential advisory from the American Heart Association. Circulation 148, 1606–1635 (2023).
Khan, S. S. et al. Development and validation of the American Heart Association’s PREVENT equations. Circulation 149, 430–449 (2024).
Hippisley-Cox, J., Coupland, C. & Brindle, P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 357, j2099 (2017).
Grams, M. E. et al. Predicting timing of clinical outcomes in patients with chronic kidney disease and severely decreased glomerular filtration rate. Kidney Int. 93, 1442–1451 (2018).
Ramspek, C. L. et al. Kidney failure prediction models: a comprehensive external validation study in patients with advanced CKD. J. Am. Soc. Nephrol. 32, 1174–1186 (2021).
Ramspek, C. L., de Jong, Y., Dekker, F. W. & van Diepen, M. Towards the best kidney failure prediction tool: a systematic review and selection aid. Nephrol. Dial. Transplant. 35, 1527–1538 (2020).
Johnson, E. S., Thorp, M. L., Platt, R. W. & Smith, D. H. Predicting the risk of dialysis and transplant among patients with CKD: a retrospective cohort study. Am. J. Kidney Dis. 52, 653–660 (2008).
Schroeder, E. B. et al. Predicting 5-year risk of RRT in stage 3 or 4 CKD: development and external validation. Clin. J. Am. Soc. Nephrol. 12, 87–94 (2017).
Zacharias, H. U. et al. A predictive model for progression of CKD to kidney failure based on routine laboratory tests. Am. J. Kidney Dis. 79, 217–230.e1 (2022).
Ferguson, T. et al. Development and external validation of a machine learning model for progression of CKD. Kidney Int. Rep. 7, 1772–1781 (2022).
Tangri, N. et al. Machine learning for prediction of chronic kidney disease progression: validation of the Klinrisk model in the CANVAS Program and CREDENCE trial. Diabetes Obes. Metab. 26, 3371–3380 (2024).
Liu, P. et al. Predicting the risks of kidney failure and death in adults with moderate to severe chronic kidney disease: multinational, longitudinal, population based, cohort study. BMJ 385, e078063 (2024).
Liu, H. et al. Epigenomic and transcriptomic analyses define core cell types, genes and targetable mechanisms for kidney disease. Nat. Genet. 54, 950–962 (2022).
Khan, A. et al. Genome-wide polygenic score to predict chronic kidney disease across ancestries. Nat. Med. 28, 1412–1420 (2022).
Gorski, M. et al. Meta-analysis uncovers genome-wide significant variants for rapid kidney function decline. Kidney Int. 99, 926–939 (2021).
Gorski, M. et al. Genetic loci and prioritization of genes for kidney function decline derived from a meta-analysis of 62 longitudinal genome-wide association studies. Kidney Int. 102, 624–639 (2022).
Bakshi, A. et al. Association of polygenic scores with chronic kidney disease phenotypes in a longitudinal study of older adults. Kidney Int. 103, 1156–1166 (2023).
Liu, L. & Kiryluk, K. Genome-wide polygenic risk predictors for kidney disease. Nat. Rev. Nephrol. 14, 723–724 (2018).
Wong, K. et al. Effects of rare kidney diseases on kidney failure: a longitudinal analysis of the UK National Registry of Rare Kidney Diseases (RaDaR) cohort. Lancet 403, 1279–1289 (2024).
Barbour, S. J. et al. Evaluating a new international risk-prediction tool in IgA nephropathy. JAMA Intern. Med. 179, 942–952 (2019).
Barbour, S. J. et al. Application of the international IgA nephropathy prediction tool one or two years post-biopsy. Kidney Int. 102, 160–172 (2022).
Irazabal, M. V. et al. Imaging classification of autosomal dominant polycystic kidney disease: a simple model for selecting patients for clinical trials. J. Am. Soc. Nephrol. 26, 160–172 (2015).
Cornec-Le Gall, E. et al. The PROPKD score: a new algorithm to predict renal survival in autosomal dominant polycystic kidney disease. J. Am. Soc. Nephrol. 27, 942–951 (2016).
Chebib, F. T. et al. A practical guide for treatment of rapidly progressive ADPKD with tolvaptan. J. Am. Soc. Nephrol. 29, 2458–2470 (2018).
Inker, L. A. et al. New creatinine- and cystatin C-based equations to estimate GFR without race. N. Engl. J. Med. 385, 1737–1749 (2021).
Pottel, H. et al. Cystatin C-based equation to estimate GFR without the inclusion of race and sex. N. Engl. J. Med. 388, 333–343 (2023).
Schaeffner, E. S. et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Ann. Intern. Med. 157, 471–481 (2012).
Inker, L. A. et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 367, 20–29 (2012).
Anderson, A. H. et al. Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am. J. Kidney Dis. 60, 250–261 (2012).
Shlipak, M. G. et al. Cystatin C versus creatinine in determining risk based on kidney function. N. Engl. J. Med. 369, 932–943 (2013).
Fu, E. L. et al. Accuracy of GFR estimating equations in patients with discordances between creatinine and cystatin C-based estimations. J. Am. Soc. Nephrol. 34, 1241–1251 (2023).
Farrington, D. K. et al. Discrepancies between cystatin C-based and creatinine-based eGFR. Clin. J. Am. Soc. Nephrol. 18, 1143–1152 (2023).
Hanna, P. E. et al. Medication-related adverse events and discordancies in cystatin C-based vs serum creatinine-based estimated glomerular filtration rate in patients with cancer. JAMA Netw. Open. 6, e2321715 (2023).
Carrero, J.-J. et al. Discordances between creatinine- and cystatin C-based estimated GFR and adverse clinical outcomes in routine clinical practice. Am. J. Kidney Dis. 82, 534–542 (2023).
Provenzano, M. et al. Albuminuria-lowering effect of dapagliflozin, eplerenone, and their combination in patients with chronic kidney disease: a randomized crossover clinical trial. J. Am. Soc. Nephrol. 33, 1569–1580 (2022).
Heerspink, H. J. L. et al. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 383, 1436–1446 (2020).
Bakris, G. L. et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N. Engl. J. Med. 383, 2219–2229 (2020).
Holtkamp, F. A. et al. An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int. 80, 282–287 (2011).
Wright, J. T. et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK tTrial. JAMA 288, 2421–2431 (2002).
Blum, M. F. et al. Dihydropyridine calcium channel blockers and kidney outcomes. J. Gen. Intern. Med. https://doi.org/10.1007/s11606-024-08762-2 (2024).
American Diabetes Association Professional Practice Committee. 11. Chronic kidney disease and risk management: standards of care in diabetes—2024. Diabetes Care 47, S219–S230 (2023).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71, 1269–1324 (2018).
Lamb, E. J., MacKenzie, F. & Stevens, P. E. How should proteinuria be detected and measured? Ann. Clin. Biochem. 46, 205–217 (2009).
Ballantyne, F. C., Gibbons, J. & O’Reilly, D. S. Urine albumin should replace total protein for the assessment of glomerular proteinuria. Ann. Clin. Biochem. 30, 101–103 (1993).
Brenner, B. M. et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N. Engl. J. Med. 345, 861–869 (2001).
Lewis, E. J. et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N. Engl. J. Med. 345, 851–860 (2001).
GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia). Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet 349, 1857–1863 (1997).
Jafar, T. H. et al. Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann. Intern. Med. 135, 73–87 (2001).
Hou, F. F. et al. Renoprotection of Optimal Antiproteinuric Doses (ROAD) study: a randomized controlled study of benazepril and losartan in chronic renal insufficiency. J. Am. Soc. Nephrol. 18, 1889 (2007).
Heart Outcomes Prevention Evaluation Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet 355, 253–259 (2000).
Mann, J. F. E. et al. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann. Intern. Med. 134, 629–636 (2001).
Solomon, S. D. et al. Renal function and effectiveness of angiotensin-converting enzyme inhibitor therapy in patients with chronic stable coronary disease in the Prevention of Events with ACE inhibition (PEACE) trial. Circulation 114, 26–31 (2006).
Xie, X. et al. Renin–angiotensin system inhibitors and kidney and cardiovascular outcomes in patients with CKD: a Bayesian network meta-analysis of randomized clinical trials. Am. J. Kidney Dis. 67, 728–741 (2016).
Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting–enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N. Engl. J. Med. 342, 145–153 (2000).
Palmer, B. F. & Clegg, D. J. Kidney-protective effects of SGLT2 inhibitors. Clin. J. Am. Soc. Nephrol. 18, 279 (2023).
Perkovic, V. et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 380, 2295–2306 (2019).
EMPA-KIDNEY Collaborative Group. Empagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 388, 117–127 (2023).
Wanner, C. et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N. Engl. J. Med. 375, 323–334 (2016).
Neal, B. et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N. Engl. J. Med. 377, 644–657 (2017).
Yen, F.-S. et al. Sodium–glucose cotransporter-2 inhibitors and the risk for dialysis and cardiovascular disease in patients with stage 5 chronic kidney disease. Ann. Intern. Med. 177, 693–700 (2024).
Marx, N., Husain, M., Lehrke, M., Verma, S. & Sattar, N. GLP-1 receptor agonists for the reduction of atherosclerotic cardiovascular risk in patients with type 2 diabetes. Circulation 146, 1882–1894 (2022).
Sattar, N. et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 9, 653–662 (2021).
Perkovic, V. et al. Effects of semaglutide on chronic kidney disease in patients with type 2 diabetes. N. Engl. J. Med. 391, 109–121 (2024).
Colhoun, H. M. et al. Long-term kidney outcomes of semaglutide in obesity and cardiovascular disease in the SELECT trial. Nat. Med. 30, 2058–2066 (2024).
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145, e895–e1032 (2022).
Pitt, B. et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N. Engl. J. Med. 385, 2252–2263 (2021).
Heerspink, H. J. L. et al. Design and baseline characteristics of the finerenone, in addition to standard of care, on the progression of kidney disease in patients with non-diabetic chronic kidney disease (FIND-CKD) randomized trial. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfae132 (2024).
US National Library of Medicine ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05047263 (2024).
Heerspink, H. J. L. et al. Atrasentan and renal events in patients with type 2 diabetes and chronic kidney disease (SONAR): a double-blind, randomised, placebo-controlled trial. Lancet 393, 1937–1947 (2019).
Rovin, B. H. et al. Efficacy and safety of sparsentan versus irbesartan in patients with IgA nephropathy (PROTECT): 2-year results from a randomised, active-controlled, phase 3 trial. Lancet 402, 2077–2090 (2023).
Rheault, M. N. et al. Sparsentan versus Irbesartan in focal segmental glomerulosclerosis. N. Engl. J. Med. 389, 2436–2445 (2023).
Tuttle, K. R. et al. Efficacy and safety of aldosterone synthase inhibition with and without empagliflozin for chronic kidney disease: a randomised, controlled, phase 2 trial. Lancet 403, 379–390 (2024).
Apperloo, E. M. et al. Efficacy and safety of SGLT2 inhibitors with and without glucagon-like peptide 1 receptor agonists: a SMART-C collaborative meta-analysis of randomised controlled trials. Lancet Diabetes Endocrinol. 12, 545–557 (2024).
Neuen, B. L. et al. Cardiovascular, kidney and safety outcomes with GLP-1 receptor agonists alone and in combination with SGLT2 inhibitors in type 2 diabetes: a systematic review and meta-analysis. Circulation 150, 1781–1790 (2024).
Neuen, B. L. et al. Estimated lifetime cardiovascular, kidney, and mortality benefits of combination treatment with SGLT2 inhibitors, GLP-1 receptor agonists, and nonsteroidal MRA compared with conventional care in patients with type 2 diabetes and albuminuria. Circulation 149, 450–462 (2024).
Rossing, P. et al. Finerenone in patients with chronic kidney disease and type 2 diabetes by sodium–glucose cotransporter 2 inhibitor treatment: the FIDELITY analysis. Diabetes Care 45, 2991–2998 (2022).
Rossing, P. et al. Finerenone in patients across the spectrum of chronic kidney disease and type 2 diabetes by glucagon‐like peptide‐1 receptor agonist use. Diabetes Obes. Metab. 25, 407–416 (2023).
Chung, E. Y. et al. Aldosterone antagonists in addition to renin angiotensin system antagonists for preventing the progression of chronic kidney disease. Cochrane Database Syst. Rev. 10, CD007004 (2020).
Desai, A. S. et al. Incident hyperkalemia, hypokalemia, and clinical outcomes during spironolactone treatment of heart failure with preserved ejection fraction: analysis of the TOPCAT trial. J. Card. Fail. 24, 313–320 (2018).
Agarwal, R. et al. Hyperkalemia risk with finerenone: results from the FIDELIO-DKD trial. J. Am. Soc. Nephrol. 33, 225–237 (2022).
Neuen, B. L. et al. Sodium-glucose cotransporter 2 inhibitors and risk of hyperkalemia in people with type 2 diabetes: a meta-analysis of individual participant data from randomized, controlled trials. Circulation 145, 1460–1470 (2022).
Ferreira, J. P. et al. Mineralocorticoid receptor antagonists and empagliflozin in patients with heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 79, 1129–1137 (2022).
Fletcher, R. A. et al. Effect of SGLT2 inhibitors on discontinuation of renin-angiotensin system blockade: a joint analysis of the CREDENCE and DAPA-CKD trials. J. Am. Soc. Nephrol. 34, 1965–1975 (2023).
Heerspink, H. J. L., Kohan, D. E. & de Zeeuw, D. New insights from SONAR indicate adding sodium glucose co-transporter 2 inhibitors to an endothelin receptor antagonist mitigates fluid retention and enhances albuminuria reduction. Kidney Int. 99, 346–349 (2021).
US National Library of Medicine ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06268873 (2024).
US National Library of Medicine ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06087835 (2024).
US National Library of Medicine ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06531824 (2024).
Baigent, C. et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet 377, 2181–2192 (2011).
Palmer, S. C. et al. Benefits and harms of statin therapy for persons with chronic kidney disease: a systematic review and meta-analysis. Ann. Intern. Med. 157, 263–275 (2012).
Upadhyay, A. et al. Lipid-lowering therapy in persons with chronic kidney disease: a systematic review and meta-analysis. Ann. Intern. Med. 157, 251–262 (2012).
Hou, W. et al. Effect of statin therapy on cardiovascular and renal outcomes in patients with chronic kidney disease: a systematic review and meta-analysis. Eur. Heart J. 34, 1807–1817 (2013).
SPRINT Research Group et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116 (2015).
Klahr, S. et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. N. Engl. J. Med. 330, 877–884 (1994).
Appel, L. J. et al. Intensive blood-pressure control in hypertensive chronic kidney disease. N. Engl. J. Med. 363, 918–929 (2010).
Ruospo, M. et al. Glucose targets for preventing diabetic kidney disease and its progression. Cochrane Database Syst. Rev. 6, CD010137 (2017).
American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes—2024. Diabetes Care 47, S158–S178 (2023).
Hostetter, T. H. et al. Chronic effects of dietary protein in the rat with intact and reduced renal mass. Kidney Int. 30, 509–517 (1986).
Hahn, D., Hodson, E. M. & Fouque, D. Low protein diets for non-diabetic adults with chronic kidney disease. Cochrane Database Syst. Rev. 10, CD001892 (2018).
Jiang, S., Fang, J. & Li, W. Protein restriction for diabetic kidney disease. Cochrane Database Syst. Rev. 1, CD014906 (2023).
Kelly, J. T. et al. Healthy dietary patterns and risk of mortality and ESRD in CKD: a meta-analysis of cohort studies. Clin. J. Am. Soc. Nephrol. CJASN 12, 272–279 (2017).
Bernier-Jean, A. et al. Dietary plant and animal protein intake and decline in estimated glomerular filtration rate among elderly women: a 10-year longitudinal cohort study. Nephrol. Dial. Transplant. 36, 1640–1647 (2021).
Haring, B. et al. Dietary protein sources and risk for incident chronic kidney disease: results from the atherosclerosis risk in communities (ARIC) study. J. Ren. Nutr. 27, 233–242 (2017).
Lew, Q.-L. J. et al. Red meat intake and risk of ESRD. J. Am. Soc. Nephrol. 28, 304–312 (2017).
McMahon, E. J., Campbell, K. L., Bauer, J. D., Mudge, D. W. & Kelly, J. T. Altered dietary salt intake for people with chronic kidney disease. Cochrane Database Syst. Rev. 6, CD010070 (2021).
Lambers Heerspink, H. J. et al. Moderation of dietary sodium potentiates the renal and cardiovascular protective effects of angiotensin receptor blockers. Kidney Int. 82, 330–337 (2012).
Neal, B. et al. Effect of salt substitution on cardiovascular events and death. N. Engl. J. Med. 385, 1067–1077 (2021).
Kieneker, L. M. et al. Low potassium excretion but not high sodium excretion is associated with increased risk of developing chronic kidney disease. Kidney Int. 90, 888–896 (2016).
Kim, H. W. et al. Urinary potassium excretion and progression of CKD. Clin. J. Am. Soc. Nephrol. 14, 330–340 (2019).
He, J. et al. Urinary sodium and potassium excretion and CKD progression. J. Am. Soc. Nephrol. 27, 1202–1212 (2016).
Leonberg-Yoo, A. K., Tighiouart, H., Levey, A. S., Beck, G. J. & Sarnak, M. J. Urine potassium excretion, kidney failure, and mortality in CKD. Am. J. Kidney Dis. 69, 341–349 (2017).
Goraya, N., Simoni, J., Jo, C.-H. & Wesson, D. E. Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney Int. 86, 1031–1038 (2014).
Gutiérrez, O. M. et al. Dietary patterns and risk of death and progression to ESRD in individuals with CKD: a cohort study. Am. J. Kidney Dis. 64, 204–213 (2014).
Kim, H. & Rebholz, C. M. Plant-based diets for kidney disease prevention and treatment. Curr. Opin. Nephrol. Hypertens. 33, 593–602 (2024).
Hultin, S. et al. A systematic review and meta-analysis on effects of bicarbonate therapy on kidney outcomes. Kidney Int. Rep. 6, 695–705 (2021).
American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: standards of care in diabetes—2024. Diabetes Care 47, S179–S218 (2023).
Marx, N. et al. 2023 ESC guidelines for the management of cardiovascular disease in patients with diabetes: developed by the task force on the management of cardiovascular disease in patients with diabetes of the European Society of Cardiology (ESC). Eur. Heart J. 44, 4043–4140 (2023).
Shin, J.-I. et al. Prescription patterns for sodium glucose cotransporter-2 inhibitors in US health systems. J. Am. Coll. Cardiol. 84, 683–693 (2024).
Joglar, J. A. et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 149, e1–e156 (2024).
Neuen, B. L. et al. Relative and absolute risk reductions in cardiovascular and kidney outcomes with canagliflozin across KDIGO risk categories: findings from the CANVAS program. Am. J. Kidney Dis. 77, 23–34.e1 (2021).
Moura, F. A. et al. Risk assessment of kidney disease progression and efficacy of SGLT2 inhibition in patients with type 2 diabetes. Diabetes Care 46, 1807–1815 (2023).
Waijer, S. W. et al. Effect of dapagliflozin on kidney and cardiovascular outcomes by baseline KDIGO risk categories: a post hoc analysis of the DAPA-CKD trial. Diabetologia 65, 1085–1097 (2022).
Bhandari, S. et al. Renin–angiotensin system inhibition in advanced chronic kidney disease. N. Engl. J. Med. 387, 2021–2032 (2022).
Qiao, Y. et al. Association between renin–angiotensin system blockade discontinuation and all-cause mortality among persons with low estimated glomerular filtration rate. JAMA Intern. Med. 180, 718–726 (2020).
Fu, E. L. et al. Stopping renin–angiotensin system inhibitors in patients with advanced CKD and risk of adverse outcomes: a nationwide study. J. Am. Soc. Nephrol. 32, 424–435 (2021).
Hou, F. F. et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N. Engl. J. Med. 354, 131–140 (2006).
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 39, 3021–3104 (2018).
Hypertension in adults: diagnosis and management. National Institute for Health and Care Excellence https://www.nice.org.uk/guidance/ng136 (2023).
Qaseem, A. et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann. Intern. Med. 166, 430–437 (2017).
Williamson, J. D. et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA 315, 2673–2682 (2016).
Ascher, S. B. et al. Incorporating individual-level treatment effects and outcome preferences into personalized blood pressure target recommendations. J. Am. Heart Assoc. 13, e033995 (2024).
Mebazaa, A. et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet 400, 1938–1952 (2022).
Neuen, B. L., Tuttle, K. R., Bakris, G. & Vaduganathan, M. Reframing chronicity with urgency in chronic kidney disease management. Clin. J. Am. Soc. Nephrol. 19, 1209 (2024).
Tang, A. B. et al. Interventions for optimization of guideline-directed medical therapy: a systematic review. JAMA Cardiol. 9, 397–404 (2024).
Neuen, B. L., Tuttle, K. R. & Vaduganathan, M. Accelerated risk-based implementation of guideline-directed medical therapy for type 2 diabetes and chronic kidney disease. Circulation 149, 1238–1240 (2024).
Chen, T. K., Hoenig, M. P., Nitsch, D. & Grams, M. E. Advances in the management of chronic kidney disease. BMJ 383, e074216 (2023).
Acknowledgements
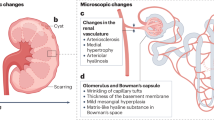
The authors thank K. Pandit, C. Flaherty and Y. Sang for their assistance in the design of figures for this manuscript before submission.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content, and reviewed or edited the manuscript before submission. M.F.B. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
B.L.N. has received fees for travel support, advisory boards, scientific presentations and steering committee roles from AstraZeneca, Alexion, Bayer, Boehringer and Ingelheim, Janssen, Novo Nordisk and Travere Therapeutics. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Peter Rossing, Paul Stevens and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Blum, M.F., Neuen, B.L. & Grams, M.E. Risk-directed management of chronic kidney disease. Nat Rev Nephrol 21, 287–298 (2025). https://doi.org/10.1038/s41581-025-00931-8
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41581-025-00931-8
This article is cited by
-
Urine as a source of biomarkers and biological knowledge in chronic kidney disease
Nature Reviews Nephrology (2026)
-
Multifactorial chronic kidney disease and the kidney capacity–workload balance
Nature Reviews Nephrology (2026)
-
Combination therapy with mineralocorticoid receptor antagonists and SGLT2 inhibitors versus SGLT2 inhibitor monotherapy in chronic kidney disease: an updated meta-analysis of randomized controlled trials
BMC Nephrology (2025)