Abstract
When kidney function is compromised, myriad metabolites and peptides — uraemic retention molecules (URMs) — accumulate in the body and compromise homeostasis. Over 150 molecules have been classified as URMs but omics approaches are revealing many more. When URMs exert pathophysiological effects and/or are associated with relevant adverse patient outcomes, they are called uraemic toxins. The origins of uraemic toxins and their contributions to post-translational modification of proteins are important current areas of research. Although most research has thus far focused on uraemic toxins, new studies have also identified URMs with the potential to counteract harmful biological changes that might thus confer a beneficial effect. To tackle the growing burden of chronic kidney disease, preventive therapeutic measures must target the disease early in its course and a balanced view of uraemic retention is needed to understand the role of URMs in kidney disease progression. Knowledge of the origin of the solutes, their kinetics, context-dependent biological profile and the involvement of transporter-mediated interorgan communication by small molecules — termed ‘remote sensing and signalling’ — is indispensable to facilitate the development of interventions that can promote or restore homeostasis in people with kidney dysfunction.
Key points
-
Uraemic retention molecules, which accumulate as kidney function declines, are key mediators in the pathophysiology of chronic kidney disease.
-
Uraemic retention molecules can be deleterious for the whole organism (termed uraemic toxins) but can also have beneficial effects.
-
Identification of uraemic toxin receptors and downstream affected signalling pathways is key to understanding their pathological effects and developing targeted therapeutic strategies.
-
Chronic kidney disease is associated with alterations in protein post-translational modifications, which can transform physiological molecules into mediators of pathology.
-
Various promising therapeutic approaches to reducing uraemic toxicity, including drug therapy, nutritional approaches, new dialysis membrane materials, as well as bioartificial and wearable artificial kidneys, are currently being investigated.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Zoccali, C. et al. The systemic nature of CKD. Nat. Rev. Nephrol. 13, 344–358 (2017).
Afkarian, M. et al. Kidney disease and increased mortality risk in type 2 diabetes. J. Am. Soc. Nephrol. 24, 302–308 (2013).
Wan, E. Y. F. et al. Burden of CKD and cardiovascular disease on life expectancy and health service utilization: a cohort study of Hong Kong Chinese hypertensive patients. J. Am. Soc. Nephrol. 30, 1991–1999 (2019).
Kalantar-Zadeh, K. et al. Patient-centred approaches for the management of unpleasant symptoms in kidney disease. Nat. Rev. Nephrol. 18, 185–198 (2022).
Foley, R. N., Parfrey, P. S. & Sarnak, M. J. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am. J. Kidney Dis. 32, S112–S119 (1998).
Matsushita, K. et al. Epidemiology and risk of cardiovascular disease in populations with chronic kidney disease. Nat. Rev. Nephrol. 18, 696–707 (2022).
Modi, Z. J. et al. Risk of cardiovascular disease and mortality in young adults with end-stage renal disease: an analysis of the US renal data system. JAMA Cardiol. 4, 353–362 (2019).
NCD_Alliance. Home / WHY NCDs / NCDs / Chronic Kidney Disease. ncdalliance.org https://ncdalliance.org/why-ncds/ncds/chronic-kidney-disease (2017).
Rosner, M. H. et al. Classification of uremic toxins and their role in kidney failure. Clin. J. Am. Soc. Nephrol. 16, 1918–1928 (2021).
Jaksch On uræmia. Chic. Med. J. 18, 396–397 (1861).
Balestri, P. L., Biagini, M., Rindi, P. & Giovannetti, S. Uremic toxins. Arch. Intern. Med. 126, 843–845 (1970).
Desi, I., Feher, E., Szold, A., Weisz, P. & Kadas, T. [Determination of toxicity of uremic blood treated with ion exchange resins]. Z. Gesamte Inn. Med. 12, 1127–1130 (1957).
Babb, A. L., Ahmad, S., Bergström, J. & Scribner, B. H. The middle molecule hypothesis in perspective. Am. J. Kidney Dis. 1, 46–50 (1981).
Thomas, M., Moriyama, K. & Ledebo, I. AN69: evolution of the world’s first high permeability membrane. Contrib. Nephrol. 173, 119–129 (2011).
Gejyo, F. et al. A new form of amyloid protein associated with chronic hemodialysis was identified as β2-microglobulin. Biochem. Biophys. Res. Commun. 129, 701–706 (1985).
Kasanen, A. Serum indican and endogenous indican clearance in renal insufficiency. Ann. Med. Intern. Fenn. Suppl. 46, 1–71 (1957).
Niwa, T. & Ise, M. Indoxyl sulfate, a circulating uremic toxin, stimulates the progression of glomerular sclerosis. J. Lab. Clin. Med. 124, 96–104 (1994).
Vanholder, R., Glorieux, G., De Smet, R. & Lameire, N. New insights in uremic toxins. Kidney Int. Suppl. 63, S6–S10.
Vanholder, R. et al. Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int. 63, 1934–1943 (2003).
Duranton, F. et al. Normal and pathologic concentrations of uremic toxins. J. Am. Soc. Nephrol. 23, 1258–1270 (2012).
Hocher, B. & Adamski, J. Metabolomics for clinical use and research in chronic kidney disease. Nat. Rev. Nephrol. 13, 269–284 (2017).
Vanholder, R. et al. Metabolomics to identify unclassified uremic toxins: a comprehensive literature review. Kidney Med. 7, 100955 (2025).
Luo, S. et al. Serum metabolomic alterations associated with proteinuria in CKD. Clin. J. Am. Soc. Nephrol. 14, 342–353 (2019).
Titan, S. M. et al. Metabolomics biomarkers and the risk of overall mortality and ESRD in CKD: results from the Progredir cohort. PLoS ONE 14, e0213764 (2019).
Wang, Z. et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472, 57–63 (2011).
Wen, D. et al. Metabolite profiling of CKD progression in the chronic renal insufficiency cohort study. JCI insight 7, e161696 (2022).
Lee, A. M. et al. Circulating metabolomic associations with neurocognitive outcomes in pediatric CKD. Clin. J. Am. Soc. Nephrol. 19, 13–25 (2024).
Kikuchi, K. et al. Gut microbiome-derived phenyl sulfate contributes to albuminuria in diabetic kidney disease. Nat. Commun. 10, 1835 (2019).
Gajjala, P. R., Fliser, D., Speer, T., Jankowski, V. & Jankowski, J. Emerging role of post-translational modifications in chronic kidney disease and cardiovascular disease. Nephrol. Dial. Transplant. 30, 1814–1824 (2015).
Noels, H. et al. Post-translational modifications in kidney diseases and associated cardiovascular risk. Nat. Rev. Nephrol. 20, 495–512 (2024).
Meijers, B., Glorieux, G., Poesen, R. & Bakker, S. J. Nonextracorporeal methods for decreasing uremic solute concentration: a future way to go? Semin. Nephrol. 34, 228–243 (2014).
Mishima, E. et al. Evaluation of the impact of gut microbiota on uremic solute accumulation by a CE-TOFMS-based metabolomics approach. Kidney Int. 92, 634–645 (2017).
Evenepoel, P, Meijers, B. K., Bammens, B. R. & Verbeke, K. Uremic toxins originating from colonic microbial metabolism. Kidney Int. 76 (Supp. 114), S12–S19 (2009).
Wikoff, W. R., Nagle, M. A., Kouznetsova, V. L., Tsigelny, I. F. & Nigam, S. K. Untargeted metabolomics identifies enterobiome metabolites and putative uremic toxins as substrates of organic anion transporter 1 (Oat1). J. Proteome Res. 10, 2842–2851 (2011).
Vanholder, R., Nigam, S. K., Burtey, S. & Glorieux, G. What if not all metabolites from the uremic toxin generating pathways are toxic? A hypothesis. Toxins 14, 221 (2022).
Ahn, S. Y. & Nigam, S. K. Toward a systems level understanding of organic anion and other multispecific drug transporters: a remote sensing and signaling hypothesis. Mol. Pharmacol. 76, 481–490 (2009).
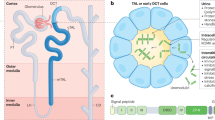
Nigam, S. K. & Bush, K. T. Uraemic syndrome of chronic kidney disease: altered remote sensing and signalling. Nat. Rev. Nephrol. 15, 301–316 (2019).
Sun, C. Y. et al. Protein-bound uremic toxins induce tissue remodeling by targeting the EGF receptor. J. Am. Soc. Nephrol. 26, 281–290 (2015).
Shepard, B. D. & Pluznick, J. L. How does your kidney smell? Emerging roles for olfactory receptors in renal function. Pediatr. Nephrol. 31, 715–723 (2016).
Wu, W. et al. Shared ligands between organic anion transporters (OAT1 and OAT6) and odorant receptors. Drug Metab. Dispos. 43, 1855–1863 (2015).
Mihaila, S. M. et al. Drugs commonly applied to kidney patients may compromise renal tubular uremic toxins excretion. Toxins 12, 391 (2020).
Mutsaers, H. A. et al. Uremic toxins inhibit transport by breast cancer resistance protein and multidrug resistance protein 4 at clinically relevant concentrations. PLoS ONE 6, e18438 (2011).
Nigam, S. K. What do drug transporters really do? Nat. Rev. Drug. Discov. 14, 29–44 (2015).
Kimura, N., Masuda, S., Katsura, T. & Inui, K. Transport of guanidine compounds by human organic cation transporters, hOCT1 and hOCT2. Biochem. Pharmacol. 77, 1429–1436 (2009).
Kuo, K. L., Zhu, H., McNamara, P. J. & Leggas, M. Localization and functional characterization of the rat Oatp4c1 transporter in an in vitro cell system and rat tissues. PLoS ONE 7, e39641 (2012).
Schophuizen, C. M. et al. Cationic uremic toxins affect human renal proximal tubule cell functioning through interaction with the organic cation transporter. Pflugers Arch. 465, 1701–1714 (2013).
Taghikhani, E., Maas, R., Fromm, M. F. & König, J. The renal transport protein OATP4C1 mediates uptake of the uremic toxin asymmetric dimethylarginine (ADMA) and efflux of cardioprotective L-homoarginine. PLoS ONE 14, e0213747 (2019).
Pengrattanachot, N. et al. Atorvastatin attenuates obese-induced kidney injury and impaired renal organic anion transporter 3 function through inhibition of oxidative stress and inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 1866, 165741 (2020).
Zhang, J., Wang, H., Fan, Y., Yu, Z. & You, G. Regulation of organic anion transporters: Role in physiology, pathophysiology, and drug elimination. Pharmacol. Ther. 217, 107647 (2021).
Santana Machado, T. et al. Indoxyl sulfate upregulates liver P-glycoprotein expression and activity through aryl hydrocarbon receptor signaling. J. Am. Soc. Nephrol. 29, 906–918 (2018).
Bhatnagar, V. et al. Analysis of ABCG2 and other urate transporters in uric acid homeostasis in chronic kidney disease: potential role of remote sensing and signaling. Clin. Kidney J. 9, 444–453 (2016).
Ermakov, V. S., Granados, J. C. & Nigam, S. K. Remote effects of kidney drug transporter OAT1 on gut microbiome composition and urate homeostasis. JCI insight 8, e172341 (2023).
Morimoto, K. et al. Intestinal secretion of indoxyl sulfate as a possible compensatory excretion pathway in chronic kidney disease. Biopharm. Drug Dispos. 39, 328–334 (2018).
Jansen, J. et al. Remote sensing and signaling in kidney proximal tubules stimulates gut microbiome-derived organic anion secretion. Proc. Natl Acad. Sci. USA 116, 16105–16110 (2019).
Makhloufi, C. et al. Female AhR knockout mice develop a minor renal insufficiency in an adenine-diet model of chronic kidney disease. Int. J. Mol. Sci. 21, 2483 (2020).
Gou, X., Ran, F., Yang, J., Ma, Y. & Wu, X. Construction and evaluation of a novel organic anion transporter 1/3 CRISPR/Cas9 double-knockout rat model. Pharmaceutics 14, 2307 (2022).
Lauriola, M. et al. Dietary protein intake and the tubular handling of indoxyl sulfate. Nephrol. Dial. Transplant. 40, 739–750 (2025).
Castillo-Rodríguez, E. et al. Inflammatory cytokines as uremic toxins: “Ni Son Todos Los Que Estan, Ni Estan Todos Los Que Son”. Toxins 9, 114 (2017).
Gryp, T., Vanholder, R., Vaneechoutte, M. & Glorieux, G. p-Cresyl sulfate. Toxins 9, 52 (2017).
Kuczera, P., Adamczak, M. & Wiecek, A. Fibroblast growth factor-23-a potential uremic toxin. Toxins 8, 369 (2016).
Leong, S. C. & Sirich, T. L. Indoxyl sulfate-review of toxicity and therapeutic strategies. Toxins 8, 358 (2016).
Vanholder, R., Gryp, T. & Glorieux, G. Urea and chronic kidney disease: the comeback of the century? (in uraemia research). Nephrol. Dial. Transplant. 33, 4–12 (2018).
Vanholder, R., Pletinck, A., Schepers, E. & Glorieux, G. Biochemical and clinical impact of organic uremic retention solutes: a comprehensive update. Toxins 10, 33 (2018).
Matsuki, H. et al. Chronic kidney disease causes blood-brain barrier breakdown via urea-activated matrix metalloproteinase-2 and insolubility of tau protein. Aging 15, 10972–10995 (2023).
Huang, B. Y. et al. High urea induces anxiety disorders associated with chronic kidney disease by promoting abnormal proliferation of OPC in amygdala. Eur. J. Pharmacol. 957, 175905 (2023).
Levassort, H. et al. Urea level and depression in patients with chronic kidney disease. Toxins 16, 326 (2024).
Xie, Y. et al. Higher blood urea nitrogen is associated with increased risk of incident diabetes mellitus. Kidney Int. 93, 741–752 (2018).
Laville, S. M. et al. Urea levels and cardiovascular disease in patients with chronic kidney disease. Nephrol. Dialysis Transplant. 38, 184–192 (2023).
Kuma, A. et al. Inhibition of urea transporter ameliorates uremic cardiomyopathy in chronic kidney disease. FASEB J. 34, 8296–8309 (2020).
Jaisson, S., Pietrement, C. & Gillery, P. Carbamylation-derived products: bioactive compounds and potential biomarkers in chronic renal failure and atherosclerosis. Clin. Chem. 57, 1499–1505 (2011).
Wu, S. J. et al. Serum uric acid levels and health outcomes in CKD: a prospective cohort study. Nephrol. Dial. Transplant. 39, 510–519 (2024).
Badve, S. V. et al. Effects of allopurinol on the progression of chronic kidney disease. N. Engl. J. Med. 382, 2504–2513 (2020).
Doria, A. et al. Serum urate lowering with allopurinol and kidney function in type 1 diabetes. N. Engl. J. Med. 382, 2493–2503 (2020).
Heerspink, H. J. L. et al. Combination treatment with verinurad and allopurinol in CKD: a randomized placebo and active controlled trial. J. Am. Soc. Nephrol. 35, 594–606 (2024).
Triches, C. B., Quinto, M., Mayer, S., Batista, M. & Zanella, M. T. Relation of asymmetrical dimethylarginine levels with renal outcomes in hypertensive patients with and without type 2 diabetes mellitus. J. Diabetes Complications 32, 316–320 (2018).
Kobayashi, S. et al. Asymmetric dimethylarginine (ADMA) as a novel risk factor for progression of coronary artery calcification in patients with chronic kidney disease. J. Clin. Med. 14, 1051 (2025).
Emrich, I. E. et al. Symmetric dimethylarginine (SDMA) outperforms asymmetric dimethylarginine (ADMA) and other methylarginines as predictor of renal and cardiovascular outcome in non-dialysis chronic kidney disease. Clin. Res. Cardiol. 107, 201–213 (2018).
Eyileten, C. et al. High concentration of symmetric dimethylarginine is associated with low platelet reactivity and increased bleeding risk in patients with acute coronary syndrome. Thromb. Res. 213, 195–202 (2022).
Hannemann, J. et al. Symmetric dimethylarginine predicts previously undetected atrial fibrillation in patients with ischemic stroke. J. Am. Heart Assoc. 13, e034994 (2024).
Koppe, L. et al. The protein-bound uremic toxin p-cresyl-sulfate promotes intracellular ROS production and lipid peroxidation in 3T3-L1 adipose cells. Biochimie 189, 137–143 (2021).
Peng, Y. S., Syu, J. P., Wang, S. D., Pan, P. C. & Kung, H. N. BSA-bounded p-cresyl sulfate potentiates the malignancy of bladder carcinoma by triggering cell migration and EMT through the ROS/Src/FAK signaling pathway. Cell Biol. Toxicol. 36, 287–300 (2020).
Stafim da Cunha, R. et al. Uremic toxins activate CREB/ATF1 in endothelial cells related to chronic kidney disease. Biochem. Pharmacol. 198, 114984 (2022).
Chen, C. et al. Damage of uremic myocardium by p-cresyl sulfate and the ameliorative effect of Klotho by regulating SIRT6 ubiquitination. Toxicol. Lett. 367, 19–31 (2022).
Rodrigues, S. D. et al. Uremic toxins promote accumulation of oxidized protein and increased sensitivity to hydrogen peroxide in endothelial cells by impairing the autophagic flux. Biochem. Biophys. Res. Commun. 523, 123–129 (2020).
Opdebeeck, B. et al. Indoxyl sulfate and p-cresyl sulfate promote vascular calcification and associate with glucose intolerance. J. Am. Soc. Nephrol. 30, 751–766 (2019).
Shiba, T. et al. p-Cresyl sulfate decreases peripheral B cells in mice with adenine-induced renal dysfunction. Toxicol. Appl. Pharmacol. 342, 50–59 (2018).
Glorieux, G. et al. Free p-cresyl sulfate shows the highest association with cardiovascular outcome in chronic kidney disease. Nephrol. Dial. Transplant. 36, 998–1005 (2021).
Verbeke, F., Vanholder, R., Van Biesen, W. & Glorieux, G. Contribution of hypoalbuminemia and anemia to the prognostic value of plasma p-cresyl sulfate and p-cresyl glucuronide for cardiovascular outcome in chronic kidney disease. J. Pers. Med. 12, 1239 (2022).
Yang, K. et al. Indoxyl sulfate induces platelet hyperactivity and contributes to chronic kidney disease-associated thrombosis in mice. Blood 129, 2667–2679 (2017).
Hamano, H. et al. The uremic toxin indoxyl sulfate interferes with iron metabolism by regulating hepcidin in chronic kidney disease. Nephrol. Dial. Transplant. 33, 586–597 (2018).
Ribeiro, A. et al. Uremic toxin indoxyl sulfate promotes macrophage-associated low-grade inflammation and epithelial cell senescence. Int. J. Mol. Sci. 24, 8031 (2023).
Rodrigues, G. G. C. et al. Indoxyl sulfate contributes to uremic sarcopenia by inducing apoptosis in myoblasts. Arch. Med. Res. 51, 21–29 (2020).
Łukawski, K., Raszewski, G. & Czuczwar, S. J. Effects of the uremic toxin indoxyl sulfate on seizure activity, learning and brain oxidative stress parameters in mice. Neurosci. Lett. 820, 137594 (2024).
Bobot, M. et al. Uremic toxic blood-brain barrier disruption mediated by AhR activation leads to cognitive impairment during experimental renal dysfunction. J. Am. Soc. Nephrol. 31, 1509–1521 (2020).
Capasso, G. et al. Drivers and mechanisms of cognitive decline in chronic kidney disease. Nat. Rev. Nephrol. 21, 536–552 (2025).
Ichisaka, Y. et al. The role of indoxyl sulfate in exacerbating colorectal cancer during chronic kidney disease progression: insights into the Akt/β-catenin/c-Myc and AhR/c-Myc pathways in HCT-116 colorectal cancer cells. Toxins 17, 17 (2025).
Saito, S., Koya, Y., Kajiyama, H., Yamashita, M. & Nawa, A. Indoxyl sulfate promotes metastatic characteristics of ovarian cancer cells via aryl hydrocarbon receptor-mediated downregulation of the Mas receptor. Lab. Invest. 103, 100025 (2023).
Lou, F. et al. Dysbiotic oral microbiota-derived kynurenine, induced by chronic restraint stress, promotes head and neck squamous cell carcinoma by enhancing CD8+ T cell exhaustion. Gut 74, 935–947 (2025).
Pawlak, K., Myśliwiec, M. & Pawlak, D. Kynurenine pathway — a new link between endothelial dysfunction and carotid atherosclerosis in chronic kidney disease patients. Adv. Med. Sci. 55, 196–203 (2010).
Mohiti, S., Alizadeh, E., Bisgaard, L. S., Ebrahimi-Mameghani, M. & Christoffersen, C. The AhR/P38 MAPK pathway mediates kynurenine-induced cardiomyocyte damage: the dual role of resveratrol in apoptosis and autophagy. Biomed. Pharmacother. 186, 118015 (2025).
Carrillo-Mora, P. et al. Kynurenines and inflammation: a remarkable axis for multiple sclerosis treatment. Pharmaceuticals 17, 983 (2024).
Isakova, T. et al. Fibroblast growth factor 23 and risks of mortality and end-stage renal disease in patients with chronic kidney disease. JAMA 305, 2432–2439 (2011).
Lau, W. L., Kalantar-Zadeh, K., Kovesdy, C. P. & Mehrotra, R. Alkaline phosphatase: better than PTH as a marker of cardiovascular and bone disease? Hemodial. Int. 18, 720–724 (2014).
Fuchs, M. A. A. et al. Fibroblast growth factor 23 and fibroblast growth factor receptor 4 promote cardiac metabolic remodeling in chronic kidney disease. Kidney Int. 107, 852–868 (2025).
Leifheit-Nestler, M. et al. Fibroblast growth factor 23 is induced by an activated renin-angiotensin-aldosterone system in cardiac myocytes and promotes the pro-fibrotic crosstalk between cardiac myocytes and fibroblasts. Nephrol. Dial. Transplant. 33, 1722–1734 (2018).
Saito, T. et al. Fibroblast growth factor 23 exacerbates cardiac fibrosis in deoxycorticosterone acetate-salt mice with hypertension. Lab. Invest. 103, 100003 (2023).
Guo, L. W., Wang, Y. K., Li, S. J., Yin, G. T. & Li, D. Elevated fibroblast growth factor 23 impairs endothelial function through the NF-κB signaling pathway. J. Atheroscler. Thromb. 30, 138–149 (2023).
Vergara, N. et al. The direct effect of fibroblast growth factor 23 on vascular smooth muscle cell phenotype and function. Nephrol. Dial. Transplant. 38, 322–343 (2023).
Yang, K. et al. Fibroblast growth factor 23 weakens chemotaxis of human blood neutrophils in microfluidic devices. Sci. Rep. 7, 3100 (2017).
Chen, S. M. et al. Hydrogen sulfide attenuates β2-microglobulin-induced cognitive dysfunction: involving recovery of hippocampal autophagic flux. Front. Behav. Neurosci. 13, 244 (2019).
Andoh, T., Maki, T., Li, S. & Uta, D. β2-microglobulin elicits itch-related responses in mice through the direct activation of primary afferent neurons expressing transient receptor potential vanilloid 1. Eur. J. Pharmacol. 810, 134–140 (2017).
Li, S., Andoh, T., Zhang, Q., Uta, D. & Kuraishi, Y. β2-microglobulin, interleukin-31, and arachidonic acid metabolites (leukotriene B4 and thromboxane A2) are involved in chronic renal failure-associated itch-associated responses in mice. Eur. J. Pharmacol. 847, 19–25 (2019).
Knopp, T. et al. Myeloid cell-derived interleukin-6 induces vascular dysfunction and vascular and systemic inflammation. Eur. Heart J. Open 4, oeae046 (2024).
Keefe, J. A. et al. Macrophage-mediated interleukin-6 signaling drives ryanodine receptor-2 calcium leak in postoperative atrial fibrillation. J. Clin. Invest. 135, e187711 (2025).
Pergola, P. E. et al. Ziltivekimab for treatment of anemia of inflammation in patients on hemodialysis: results from a phase 1/2 multicenter, randomized, double-blind, placebo-controlled trial. J. Am. Soc. Nephrol. 32, 211–222 (2021).
Durlacher-Betzer, K. et al. Interleukin-6 contributes to the increase in fibroblast growth factor 23 expression in acute and chronic kidney disease. Kidney Int. 94, 315–325 (2018).
Velloso, F. J., Zaritsky, R., Houbeika, R. Y., Rios, N. & Levison, S. W. Interleukin-6 produces behavioral deficits in pre-pubescent mice independent of neuroinflammation. Brain, Behav. Immun. 126, 275–288 (2025).
Keshari, S. et al. IL-6/p-BTK/p-ERK signaling mediates calcium phosphate-induced pruritus. FASEB J. 33, 12036–12046 (2019).
Meyer, T. W. & Hostetter, T. H. Uremia. N. Engl. J. Med. 357, 1316–1325 (2007).
Hénaut, L., Mary, A., Chillon, J. M., Kamel, S. & Massy, Z. A. The impact of uremic toxins on vascular smooth muscle cell function. Toxins 10, 218 (2018).
Evenepoel, P., Stenvinkel, P., Shanahan, C. & Pacifici, R. Inflammation and gut dysbiosis as drivers of CKD-MBD. Nat. Rev. Nephrol. 19, 646–657 (2023).
Kolachalama, V. B. et al. Uremic solute-aryl hydrocarbon receptor-tissue factor axis associates with thrombosis after vascular injury in humans. J. Am. Soc. Nephrol. 29, 1063–1072 (2018).
Arinze, N. V. et al. Tryptophan metabolites suppress the Wnt pathway and promote adverse limb events in chronic kidney disease. J. Clin. Invest. 132, e142260 (2022).
Hung, S. C. et al. Indoxyl sulfate suppresses endothelial progenitor cell-mediated neovascularization. Kidney Int. 89, 574–585 (2016).
Chermiti, R., Burtey, S. & Dou, L. Role of uremic toxins in vascular inflammation associated with chronic kidney disease. J. Clin. Med. 13, 7149 (2024).
Santana Machado, T., Cerini, C. & Burtey, S. Emerging roles of aryl hydrocarbon receptors in the altered clearance of drugs during chronic kidney disease. Toxins 11, 209 (2019).
Bock, K. W. Aryl hydrocarbon receptor (AHR)-mediated inflammation and resolution: non-genomic and genomic signaling. Biochem. Pharmacol. 182, 114220 (2020).
Ravid, J. D., Kamel, M. H. & Chitalia, V. C. Uraemic solutes as therapeutic targets in CKD-associated cardiovascular disease. Nat. Rev. Nephrol. 17, 402–416 (2021).
Addi, T. et al. Mechanisms of tissue factor induction by the uremic toxin indole-3 acetic acid through aryl hydrocarbon receptor/nuclear factor-kappa B signaling pathway in human endothelial cells. Arch. Toxicol. 93, 121–136 (2019).
Merchak, A. R. et al. The activity of the aryl hydrocarbon receptor in T cells tunes the gut microenvironment to sustain autoimmunity and neuroinflammation. PLoS Biol. 21, e3002000 (2023).
Lamas, B. et al. Aryl hydrocarbon receptor ligand production by the gut microbiota is decreased in celiac disease leading to intestinal inflammation. Sci. Transl. Med. 12, eaba0624 (2020).
Wiggins, B. G. et al. Endothelial sensing of AHR ligands regulates intestinal homeostasis. Nature 621, 821–829 (2023).
Schnabl, B., Damman, C. J. & Carr, R. M. Metabolic dysfunction-associated steatotic liver disease and the gut microbiome: pathogenic insights and therapeutic innovations. J. Clin. Investig. 135, e186423 (2025).
Dou, L. et al. Aryl hydrocarbon receptor is activated in patients and mice with chronic kidney disease. Kidney Int. 93, 986–999 (2018).
Evenepoel, P., Bover, J. & Ureña Torres, P. Parathyroid hormone metabolism and signaling in health and chronic kidney disease. Kidney Int. 90, 1184–1190 (2016).
Sinha, A. K. et al. Dietary fibre directs microbial tryptophan metabolism via metabolic interactions in the gut microbiota. Nat. Microbiol. 9, 1964–1978 (2024).
Seymour, B. J. et al. Microbiota-dependent indole production stimulates the development of collagen-induced arthritis in mice. J. Clin. Invest. 134, e167671 (2023).
Vaziri, N. D., Oveisi, F., Wierszbiezki, M., Shaw, V. & Sporty, L. D. Serum melatonin and 6-sulfatoxymelatonin in end-stage renal disease: effect of hemodialysis. Artif. Organs 17, 764–769 (1993).
Takahashi, R. et al. The significance of NAD + metabolites and nicotinamide N-methyltransferase in chronic kidney disease. Sci. Rep. 12, 6398 (2022).
Walker, J. A. et al. Indoleamine 2,3-dioxygenase-1, a novel therapeutic target for post-vascular injury thrombosis in CKD. J. Am. Soc. Nephrol. 32, 2834–2850 (2021).
Mair, R. D., Sirich, T. L., Plummer, N. S. & Meyer, T. W. Characteristics of colon-derived uremic solutes. Clin. J. Am. Soc. Nephrol. 13, 1398–1404 (2018).
Nemet, I. et al. Microbe-derived uremic solutes enhance thrombosis potential in the host. mBio 14, e0133123 (2023).
Nemet, I. et al. Atlas of gut microbe-derived products from aromatic amino acids and risk of cardiovascular morbidity and mortality. Eur. Heart J. 44, 3085–3096 (2023).
Tang, W. H. et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ. Res. 116, 448–455 (2015).
Chapron, A. et al. Does secretory clearance follow glomerular filtration rate in chronic kidney diseases? Reconsidering the intact nephron hypothesis. Clin. Transl. Sci. 10, 395–403 (2017).
Lowenstein, J. & Grantham, J. J. Residual renal function: a paradigm shift. Kidney Int. 91, 561–565 (2017).
Cohen, G. et al. Review on uraemic toxins III: recommendations for handling uraemic retention solutes in vitro — towards a standardized approach for research on uraemia. Nephrol. Dial. Transplant. 22, 3381–3390 (2007).
Schulman, G. et al. Randomized placebo-controlled EPPIC trials of AST-120 in CKD. J. Am. Soc. Nephrol. 26, 1732–1746 (2015).
Su, P. Y. et al. Efficacy of AST-120 for patients with chronic kidney disease: a network meta-analysis of randomized controlled trials. Front. Pharmacol. 12, 676345 (2021).
Pietrement, C., Gorisse, L., Jaisson, S. & Gillery, P. Chronic increase of urea leads to carbamylated proteins accumulation in tissues in a mouse model of CKD. PLoS ONE 8, e82506 (2013).
Verbrugge, F. H., Tang, W. H. & Hazen, S. L. Protein carbamylation and cardiovascular disease. Kidney Int. 88, 474–478 (2015).
Miyata, T., Kurokawa, K. & van Ypersele de Strihou, C. Relevance of oxidative and carbonyl stress to long-term uremic complications. Kidney Int. Suppl. 76, S120–S125 (2000).
Soulage, C. O. et al. Two toxic lipid aldehydes, 4-hydroxy-2-hexenal (4-HHE) and 4-hydroxy-2-nonenal (4-HNE), accumulate in patients with chronic kidney disease. Toxins 12, 567 (2020).
Agalou, S., Ahmed, N., Babaei-Jadidi, R., Dawnay, A. & Thornalley, P. J. Profound mishandling of protein glycation degradation products in uremia and dialysis. J. Am. Soc. Nephrol. 16, 1471–1485 (2005).
Rabbani, N., Sebekova, K., Sebekova, K. Jr., Heidland, A. & Thornalley, P. J. Accumulation of free adduct glycation, oxidation, and nitration products follows acute loss of renal function. Kidney Int. 72, 1113–1121 (2007).
Liu, Z., Yang, J., Du, M. & Xin, W. Functioning and mechanisms of PTMs in renal diseases. Front. Pharmacol. 14, 1238706 (2023).
Hermann, J., Schurgers, L. & Jankowski, V. Identification and characterization of post-translational modifications: clinical implications. Mol. Aspects Med. 86, 101066 (2022).
Bradley, D. The evolution of post-translational modifications. Curr. Opin. Genet. Dev. 76, 101956 (2022).
Delporte, C. et al. Myeloperoxidase-catalyzed oxidation of cyanide to cyanate: a potential carbamylation route involved in the formation of atherosclerotic plaques? J. Biol. Chem. 293, 6374–6386 (2018).
Jankowski, V. et al. Carbamylated sortilin associates with cardiovascular calcification in patients with chronic kidney disease. Kidney Int. 101, 574–584 (2022).
Speer, T. et al. Carbamylated low-density lipoprotein induces endothelial dysfunction. Eur. Heart J. 35, 3021–3032 (2014).
Kalim, S. et al. Protein carbamylation and chronic kidney disease progression in the Chronic Renal Insufficiency Cohort Study. Nephrol. Dial. Transplant. 37, 139–147 (2021).
Tang, M. et al. The impact of carbamylation and anemia on HbA1c’s association with renal outcomes in patients with diabetes and chronic kidney disease. Diabetes Care 46, 130–137 (2023).
Rueth, M. et al. Guanidinylations of albumin decreased binding capacity of hydrophobic metabolites. Acta Physiol. 215, 13–23 (2015).
Apostolov, E. O., Ray, D., Savenka, A. V., Shah, S. V. & Basnakian, A. G. Chronic uremia stimulates LDL carbamylation and atherosclerosis. J. Am. Soc. Nephrol. 21, 1852–1857 (2010).
Bonnin-Marquez, A. et al. Guanidinylation compromises the anti-inflammatory and anti-oxidative properties of apolipoprotein A-I in chronic kidney disease progression. Kidney Int. 107, 916–929 (2025).
Schunk, S. J. et al. Guanidinylated apolipoprotein C3 (ApoC3) associates with kidney and vascular injury. J. Am. Soc. Nephrol. 32, 3146–3160 (2021).
Zewinger, S. et al. Apolipoprotein C3 induces inflammation and organ damage by alternative inflammasome activation. Nat. Immunol. 21, 30–41 (2020).
Schuett, K. et al. Clot structure: a potent mortality risk factor in patients on hemodialysis. J. Am. Soc. Nephrol. 28, 1622–1630 (2017).
Jankowski, V., Lellig, M. & Jankowski, J. WCN24-66 Post-translational guanidinylation of the HDL protein ApoA-1. Kidney Int. Rep. 9, S658 (2024).
Tölle, M. et al. High-density lipoprotein loses its anti-inflammatory capacity by accumulation of pro-inflammatory-serum amyloid A. Cardiovasc. Res. 94, 154–162 (2012).
Ebert, T. et al. Inflammation and oxidative stress in chronic kidney disease and dialysis patients. Antioxid. Redox Signal. 35, 1426–1448 (2021).
Juan, C. A., Pérez de la Lastra, J. M., Plou, F. J. & Pérez-Lebeña, E. The chemistry of reactive oxygen species (ROS) revisited: outlining their role in biological macromolecules (DNA, lipids and proteins) and induced pathologies. Int. J. Mol. Sci. 22, 4642 (2021).
Florens, N. et al. CKD increases carbonylation of HDL and is associated with impaired antiaggregant properties. J. Am. Soc. Nephrol. 31, 1462–1477 (2020).
Hoffman, S. et al. Thiol redox chemistry: role of protein cysteine oxidation and altered redox homeostasis in allergic inflammation and asthma. J. Cell. Biochem. 116, 884–892 (2015).
Amiya, E. Interaction of hyperlipidemia and reactive oxygen species: Insights from the lipid-raft platform. World J. Cardiol. 8, 689–694 (2016).
Reyes, C. et al. Loxin reduced the inflammatory response in the liver and the aortic fatty streak formation in mice fed with a high-fat diet. Int. J. Mol. Sci. 23, 7329 (2022).
Zhang, Q. et al. High glucose/ox-LDL induced hepatic sinusoidal capillarization via αvβ5/FAK/ERK signaling pathway. Biochem. Biophys. Res. Commun. 513, 1055–1062 (2019).
Besler, C., Lüscher, T. F. & Landmesser, U. Molecular mechanisms of vascular effects of high-density lipoprotein: alterations in cardiovascular disease. EMBO Mol. Med. 4, 251–268 (2012).
Nakajima, T. et al. Localization of oxidized HDL in atheromatous plaques and oxidized HDL binding sites on human aortic endothelial cells. Ann. Clin. Biochem. 37, 179–186 (2000).
Thorne, R. F., Mhaidat, N. M., Ralston, K. J. & Burns, G. F. CD36 is a receptor for oxidized high density lipoprotein: implications for the development of atherosclerosis. FEBS Lett. 581, 1227–1232 (2007).
Glorieux, G., Gryp, T. & Perna, A. Gut-derived metabolites and their role in immune dysfunction in chronic kidney disease. Toxins 12, 245 (2020).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 105, S117–S314 (2024).
Billing, A. M. et al. Metabolic communication by SGLT2 inhibition. Circulation 149, 860–884 (2024).
He, L. et al. Canagliflozin attenuates kidney injury, gut-derived toxins, and gut microbiota imbalance in high-salt diet-fed Dahl salt-sensitive rats. Ren. Fail. 46, 2300314 (2024).
Matsui, A. et al. Canagliflozin protects the cardiovascular system through effects on the gut environment in non-diabetic nephrectomized rats. Clin. Exp. Nephrol. 27, 295–308 (2023).
Mishima, E. et al. Canagliflozin reduces plasma uremic toxins and alters the intestinal microbiota composition in a chronic kidney disease mouse model. Am. J. Physiol. Renal Physiol. 315, F824–F833 (2018).
Sokolov, V. et al. Differentiating the sodium-glucose cotransporter 1 inhibition capacity of canagliflozin vs. dapagliflozin and empagliflozin using quantitative systems pharmacology modeling. CPT Pharmacometrics Syst. Pharmacol. 9, 222–229 (2020).
Sun, C. Y., Chang, S. C. & Wu, M. S. Uremic toxins induce kidney fibrosis by activating intrarenal renin-angiotensin-aldosterone system associated epithelial-to-mesenchymal transition. PLoS ONE 7, e34026 (2012).
Iguchi, A. et al. Effect of sucroferric oxyhydroxide on gastrointestinal microbiome and uremic toxins in patients with chronic kidney disease undergoing hemodialysis. Clin. Exp. Nephrol. 24, 725–733 (2020).
Lau, W. L. et al. The phosphate binder ferric citrate alters the gut microbiome in rats with chronic kidney disease. J. Pharmacol. Exp. Ther. 367, 452–460 (2018).
Laville, S. M. et al. Intestinal chelators, sorbants, and gut-derived uremic toxins. Toxins 13, 91 (2021).
Aronov, P. A. et al. Colonic contribution to uremic solutes. J. Am. Soc. Nephrol. 22, 1769–1776 (2011).
Lee, J. et al. Antibiotic-induced intestinal microbiota depletion can attenuate the acute kidney injury to chronic kidney disease transition via NADPH oxidase 2 and trimethylamine-N-oxide inhibition. Kidney Int. 105, 1239–1253 (2024).
Nazzal, L. et al. Effect of vancomycin on the gut microbiome and plasma concentrations of gut-derived uremic solutes. Kidney Int. Rep. 6, 2122–2133 (2021).
Sumida, K., Lau, W. L., Kalantar-Zadeh, K. & Kovesdy, C. P. Novel intestinal dialysis interventions and microbiome modulation to control uremia. Curr. Opin. Nephrol. Hypertens. 31, 82–91 (2022).
Roager, H. M. et al. Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Nat. Microbiol. 1, 16093 (2016).
Kim, K., Cho, W. H., Hwang, S. D., Lee, S. W. & Song, J. H. Association between constipation and incident chronic kidney disease in the UK Biobank study. Sci. Rep. 14, 32106 (2024).
Sumida, K. et al. Constipation and incident CKD. J. Am. Soc. Nephrol. 28, 1248–1258 (2017).
Sumida, K. et al. Laxative use in patients with advanced chronic kidney disease transitioning to dialysis. Nephrol. Dial. Transplant. 36, 2018–2026 (2021).
Nanto-Hara, F. et al. The guanylate cyclase C agonist linaclotide ameliorates the gut-cardio-renal axis in an adenine-induced mouse model of chronic kidney disease. Nephrol. Dial. Transplant. 35, 250–264 (2020).
Sueyoshi, M. et al. Effects of lactulose on renal function and gut microbiota in adenine-induced chronic kidney disease rats. Clin. Exp. Nephrol. 23, 908–919 (2019).
Benech, N. & Koppe, L. Is there a place for faecal microbiota transplantation in chronic kidney disease? Nephrol. Dial. Transplant. 37, 2303–2306 (2022).
Schulman, G. et al. The effects of AST-120 on chronic kidney disease progression in the United States of America: a post hoc subgroup analysis of randomized controlled trials. BMC Nephrol. 17, 141 (2016).
Abe, H. & Otsuka, M. Comparison of physico-chemical characteristics among three pharmaceutical spherical carbon adsorbents. Colloids Surf. B Biointerfaces 100, 90–94 (2012).
Kato, S. et al. Zirconium-based metal-organic frameworks for the removal of protein-bound uremic toxin from human serum albumin. J. Am. Chem. Soc. 141, 2568–2576 (2019).
Wei, J. et al. Efficient selective removal of uremic toxin precursor by olefin-linked covalent organic frameworks for nephropathy treatment. Nat. Commun. 14, 2805 (2023).
Wang, Z. et al. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell 163, 1585–1595 (2015).
Graboski, A. L. et al. Mechanism-based inhibition of gut microbial tryptophanases reduces serum indoxyl sulfate. Cell Chem. Biol. 30, 1402–1413.e7 (2023).
Shashar, M. et al. Targeting STUB1-tissue factor axis normalizes hyperthrombotic uremic phenotype without increasing bleeding risk. Sci. Transl. Med. 9, eaam8475 (2017).
Stockinger, B., Shah, K. & Wincent, E. AHR in the intestinal microenvironment: safeguarding barrier function. Nat. Rev. Gastroenterol. Hepatol. 18, 559–570 (2021).
Cotillard, A. et al. Dietary intervention impact on gut microbial gene richness. Nature 500, 585–588 (2013).
De Filippo, C. et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl Acad. Sci. USA 107, 14691–14696 (2010).
Gill, S. R. et al. Metagenomic analysis of the human distal gut microbiome. Science 312, 1355–1359 (2006).
Ikizler, T. A. et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am. J. Kidney Dis. 76, S1–s107 (2020).
Kalantar-Zadeh, K. & Fouque, D. Nutritional management of chronic kidney disease. N. Engl. J. Med. 377, 1765–1776 (2017).
Koppe, L. & Soulage, C. O. The impact of dietary nutrient intake on gut microbiota in the progression and complications of chronic kidney disease. Kidney Int. 102, 728–739 (2022).
Carrero, J. J. et al. Plant-based diets to manage the risks and complications of chronic kidney disease. Nat. Rev. Nephrol. 16, 525–542 (2020).
Koppe, L., Fouque, D. & Soulage, C. O. The role of gut microbiota and diet on uremic retention solutes production in the context of chronic kidney disease. Toxins 10, 155 (2018).
Letourneau, P., Bataille, S., Chauveau, P., Fouque, D. & Koppe, L. Source and composition in amino acid of dietary proteins in the primary prevention and treatment of CKD. Nutrients 12, 3892 (2020).
Koppe, L., Cassani de Oliveira, M. & Fouque, D. Ketoacid analogues supplementation in chronic kidney disease and future perspectives. Nutrients 11, 2071 (2019).
Stanford, J. et al. High-diversity plant-based diet and gut microbiome, plasma metabolome, and symptoms in adults with CKD. Clin. J. Am. Soc. Nephrol. 20, 619–631 (2025).
Stanford, J. et al. Associations among plant-based diet quality, uremic toxins, and gut microbiota profile in adults undergoing hemodialysis therapy. J. Ren. Nutr. 31, 177–188 (2021).
Hu, E. A. et al. Adherence to healthy dietary patterns and risk of CKD progression and all-cause mortality: findings from the CRIC (Chronic Renal Insufficiency Cohort) study. Am. J. Kidney Dis. 77, 235–244 (2021).
Kelly, J. T. et al. Healthy dietary patterns and risk of mortality and ESRD in CKD: a meta-analysis of cohort studies. Clin. J. Am. Soc. Nephrol. 12, 272–279 (2017).
Podadera-Herreros, A. et al. Long-term consumption of a Mediterranean diet or a low-fat diet on kidney function in coronary heart disease patients: the CORDIOPREV randomized controlled trial. Clin. Nutr. 41, 552–559 (2022).
Yoshifuji, A. et al. Gut Lactobacillus protects against the progression of renal damage by modulating the gut environment in rats. Nephrol. Dial. Transplant. 31, 401–412 (2016).
Barba, C. et al. A low aromatic amino-acid diet improves renal function and prevent kidney fibrosis in mice with chronic kidney disease. Sci. Rep. 11, 19184 (2021).
Lobel, L., Cao, Y. G., Fenn, K., Glickman, J. N. & Garrett, W. S. Diet posttranslationally modifies the mouse gut microbial proteome to modulate renal function. Science 369, 1518–1524 (2020).
Wang, X. et al. Aberrant gut microbiota alters host metabolome and impacts renal failure in humans and rodents. Gut 69, 2131–2142 (2020).
Mafra, D. et al. Food as medicine: targeting the uraemic phenotype in chronic kidney disease. Nat. Rev. Nephrol. 17, 153–171 (2021).
Whelan, K., Bancil, A. S., Lindsay, J. O. & Chassaing, B. Ultra-processed foods and food additives in gut health and disease. Nat. Rev. Gastroenterol. Hepatol. 21, 406–427 (2024).
Koppe, L. & Fouque, D. Microbiota and prebiotics modulation of uremic toxin generation. Panminerva Med. 59, 173–187 (2017).
Koppe, L., Mafra, D. & Fouque, D. Probiotics and chronic kidney disease. Kidney Int. 88, 958–966 (2015).
Cooper, T. E. et al. Synbiotics, prebiotics and probiotics for people with chronic kidney disease. Cochrane Database Syst. Rev. 10, CD013631 (2023).
Liu, C., Yang, L., Wei, W. & Fu, P. Efficacy of probiotics/synbiotics supplementation in patients with chronic kidney disease: a systematic review and meta-analysis of randomized controlled trials. Front. Nutr. 11, 1434613 (2024).
Liu, J. et al. Biotic supplements in patients with chronic kidney disease: meta-analysis of randomized controlled trials. J. Ren. Nutr. 32, 10–21 (2022).
Ribeiro, F. P. B., de Luna Freire, M. O., de Oliveira Coutinho, D., de Santana Cirilo, M. A. & de Brito Alves, J. L. Gut dysbiosis and probiotic therapy in chronic kidney disease: a comprehensive review. Probiotics Antimicrob. Proteins 17, 1797–1819 (2025).
Voroneanu, L. et al. Gut microbiota in chronic kidney disease: from composition to modulation towards better outcomes-a systematic review. J. Clin. Med. 12, 1948 (2023).
More, S. et al. Evaluation of existing guidelines for their adequacy for the food and feed risk assessment of microorganisms obtained through synthetic biology. EFSA 20, e07479 (2022).
Cao, J. et al. Lactobacillus paracasei X11 ameliorates hyperuricemia and modulates gut microbiota in mice. Front. Immunol. 13, 940228 (2022).
Li, H. B. et al. Faecalibacterium prausnitzii Attenuates CKD via Butyrate-Renal GPR43 Axis. Circulation Res. 131, e120–e134 (2022).
Zhu, H. et al. The probiotic L. casei Zhang slows the progression of acute and chronic kidney disease. Cell Metab. 33, 2091–2093 (2021).
Magnani, S. & Atti, M. Uremic toxins and blood purification: a review of current evidence and future perspectives. Toxins 13, 246 (2021).
de Vries, J. C. et al. Evidence on continuous flow peritoneal dialysis: a review. Semin. Dial. 35, 481–497 (2022).
Sánchez-Ospina, D. et al. Displacing the burden: a review of protein-bound uremic toxin clearance strategies in chronic kidney disease. J. Clin. Med. 13, 1428 (2024).
Blankestijn, P. J. et al. Effect of hemodiafiltration or hemodialysis on mortality in kidney failure. N. Engl. J. Med. 389, 700–709 (2023).
Grooteman, M. P. et al. Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes. J. Am. Soc. Nephrol. 23, 1087–1096 (2012).
van Gelder, M. K. et al. Protein-bound uremic toxins in hemodialysis patients relate to residual kidney function, are not influenced by convective transport, and do not relate to outcome. Toxins 12, 234 (2020).
Fiorentino, M., La Fergola, F. & De Rosa, S. Medium cut-off dialyzer for middle molecular uremic toxins in AKI and chronic dialysis. J. Nephrol. 37, 23–37 (2024).
Maduell, F. et al. Comparison of four medium cut-off dialyzers. Clin. Kidney J. 15, 2292–2299 (2022).
Eloot, S. et al. Impact of hemodialysis duration on the removal of uremic retention solutes. Kidney Int. 73, 765–770 (2008).
Furue, M. & Tsuji, G. Chloracne and hyperpigmentation caused by exposure to hazardous aryl hydrocarbon receptor ligands. Int. J. Environ. Res. Public. Health 16, 4864 (2019).
GBD 2021 Forecasting Collaborators Burden of disease scenarios for 204 countries and territories, 2022–2050: a forecasting analysis for the global burden of disease study 2021. Lancet 403, 2204–2256 (2024).
Ramada, D. L. et al. Portable, wearable and implantable artificial kidney systems: needs, opportunities and challenges. Nat. Rev. Nephrol. 19, 481–490 (2023).
Ghosh, A. et al. Effective clearance of uremic toxins using functionalised silicon Nanoporous membranes. Biomed. Microdevices 23, 4 (2021).
Zhang, Q., Lu, X., Yang, S., Zhang, Q. & Zhao, L. Preparation of anticoagulant polyvinylidene fluoride hollow fiber hemodialysis membranes. Biomed. Tech. 62, 57–65 (2017).
Kim, D. & Stamatialis, D. High flux mixed matrix membrane with low albumin leakage for blood plasma detoxification. J. Membr. Sci. 609, 118187 (2020).
Maheshwari, V., Tao, X., Thijssen, S. & Kotanko, P. Removal of protein-bound uremic toxins using binding competitors in hemodialysis: a narrative review. Toxins 13, 622 (2021).
Shi, Y. et al. Removal of protein-bound uremic toxins by liposome-supported peritoneal dialysis. Perit. Dial. Int. 39, 509–518 (2019).
Raillon, L. A. et al. Medium chain fatty acids are potent binding competitors to improve protein-bound uremic toxin clearance during hemodialysis. Kidney Int. 108, 411–426 (2025).
Devlin, A. S. et al. Modulation of a circulating uremic solute via rational genetic manipulation of the gut microbiota. Cell Host Microbe 20, 709–715 (2016).
Lubkowicz, D., Hava, D. L., Lewis, K. & Isabella, V. M. Rational engineering of Escherichia coli Nissle 1917 as live biotherapeutic to degrade uremic toxin precursors. ACS Synth. Biol. 13, 1077–1084 (2024).
De Chiara, F., Ferret-Miñana, A., Fernández-Costa, J. M. & Ramón-Azcón, J. The tissue engineering revolution: from bench research to clinical reality. Biomedicines 12, 453 (2024).
Freedman, B. S. & Dekel, B. Engraftment of kidney organoids in vivo. Curr. Transplant. Rep. 10, 29–39 (2023).
Milani, N., Parrott, N., Galetin, A., Fowler, S. & Gertz, M. In silico modeling and simulation of organ-on-a-chip systems to support data analysis and a priori experimental design. CPT Pharmacometrics Syst. Pharmacol. 13, 524–543 (2024).
Lopes, M. B. et al. The omics-driven machine learning path to cost-effective precision medicine in chronic kidney disease. Proteomics 11–12, e202400108 (2025).
Aiyegbusi, O. L. et al. Measurement properties of patient-reported outcome measures (PROMs) used in adult patients with chronic kidney disease: a systematic review. PLoS ONE 12, e0179733 (2017).
Tong, A. et al. Implementing core outcomes in kidney disease: report of the standardized outcomes in nephrology (SONG) implementation workshop. Kidney Int. 94, 1053–1068 (2018).
Aranda-Rivera, A. K., Cruz-Gregorio, A., Aparicio-Trejo, O. E. & Pedraza-Chaverri, J. Mitochondrial redox signaling and oxidative stress in kidney diseases. Biomolecules 11, 1144 (2021).
Kehm, R., Baldensperger, T., Raupbach, J. & Höhn, A. Protein oxidation — formation mechanisms, detection and relevance as biomarkers in human diseases. Redox Biol. 42, 101901 (2021).
Suzuki, Y. J. Oxidant-mediated protein amino acid conversion. Antioxidants 8, 50 (2019).
Acknowledgements
The authors thank the members of the EUTox work group for their ideas, research, discussions and efforts in standardizing uraemic toxin-related research: A. Argiles, Montpellier, France; J. Beige, Leipzig, Germany; P. Brunet, Marseille, France; J.-M. Chillon, Amiens, France; G. Cohen, Vienna, Austria; O. Abou Deif, Hamburg, Germany; D. Fliser, Homburg/Saar, Germany; I. Fridolin, Tallinn, Estonia; V. Jankowski, Aachen, Germany; Z. A. Massy, Paris, France; H. Mischak, Hannover, Germany; A. Ortiz, Madrid, Spain; A. Perna, Naples, Italy; J. Mariano Rodriguez-Portillo, Cordoba, Spain; J. Schanstra, Toulouse, France; J. Siwy, Hannover, Germany; G. Spasovski, Skopje, Republic of North Macedonia; D. Stamatialis, Twente, The Netherlands; B. G. Stegmayr, Umea, Sweden; P. Stenvinkel, Stockholm, Sweden; R. Stojanov, Skopje, Republic of North Macedonia; A. Vlahou, Athens, Greece; and A. Wiecek, Katowice, Poland. All authors are members of the EUTox work group. J.J. is supported by grants from the Interdisciplinary Center for Clinical Research within the Faculty of Medicine at the RWTH Aachen University and the ‘Deutsche Forschungsgemeinschaft‘ (DFG, German Research Foundation) by the Transregional Collaborative Research Centre (Project-ID 322900939), INST 948/4S-1, CRU 5011 (Project-ID 445703531) and IZKF FACROSS and Phase Transition in Disease (1-1) of the University of Aachen (Germany) Cost-Action CA 21165, ERA-PerMed (ERA-PERMED2022-202-KidneySign).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content and wrote, reviewed or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The EUTox Work Group (of which all authors are members) receives unrestricted grants from Fresenius Medical Care, Baxter Healthcare and B. Braun Avitum AG. S.B. received honoraria for conferences from Astra-Zeneca, Amgen, Lilly and Vifor CLS. L.K. has received grants from Fresenius Kabi, Nestlé, Lallemand, AstraZeneca, and consultancy or speaker fees or travel support from AstraZeneca, Lilly, Baxter, Bayer and Fresenius Kabi.
Peer review
Peer review information
Nature Reviews Nephrology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Glorieux, G., Burtey, S., Evenepoel, P. et al. A guide to uraemic toxicity. Nat Rev Nephrol 22, 50–68 (2026). https://doi.org/10.1038/s41581-025-01006-4
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41581-025-01006-4
This article is cited by
-
Developmentally dynamic chromatin state at loci regulating organ crosstalk by remote sensing and signaling
Epigenetics & Chromatin (2025)