Abstract
Healthcare-associated infections (HAIs) pose a significant challenge in resource-limited settings, such as Somalia, where hand hygiene is recognized as a primary preventive measure. This study assessed hand hygiene beliefs and practices among healthcare workers (HCWs) at a tertiary hospital in Mogadishu, Somalia. A cross-sectional study was conducted from April to June 2024 involving 304 randomly selected HCWs at the Mogadishu Somali-Turkiye Recep Tayyip Erdogan Training and Research Hospital. Data was collected using the Hand Hygiene Beliefs Scale (HHBS) and Hand Hygiene Practices Inventory (HHPI). Data were analyzed using descriptive statistics and a Generalized Linear Model (GLM) to identify significant factors associated with belief and practice scores, with significance set at . The findings revealed a strong belief in hand hygiene but only moderate adherence to practices. The multivariable GLM analysis indicated that for hand hygiene beliefs, holding a Master’s degree degree \((\beta=-0.257,p=0.041)\) and having 10–15 years of experience \((\beta=-0.391, p=0.001)\) were significantly associated with lower practice scores. A significant discrepancy exists between hand hygiene beliefs and practices, influenced heavily by educational level, profession, and years of experience. Enhancing patient safety requires targeted, systemic interventions, such as peer-mentoring for nurses, refresher training for mid-career professionals, and specialized monitoring in high-risk departments to bridge the gap between belief and clinical application.
Similar content being viewed by others
Data availability
The data used in this study shall be available upon reasonable request from the corresponding author.
References
Price, L. et al. Effectiveness of National and subnational infection prevention and control interventions in high-income and upper-middle-income countries: a systematic review. Lancet Infect. Dis. 18, e159–e171. https://doi.org/10.1016/S1473-3099(17)30479-6 (2018).
Kumar, A. et al. Assessment of healthcare worker’s hand hygiene and infection prevention practices of their personal belongings in a healthcare setting: a survey in pre COVID-19 era and literature review on standard disinfection practices. J. Prev. Med. Hyg. 62, E104. https://doi.org/10.15167/2421-4248/jpmh2021.62.1.1742 (2021).
Oy, S. et al. Developing an infection prevention and control intervention to reduce hospital-acquired infections in Cambodia and Lao people’s Democratic republic: the HAI-PC study protocol. Front. Public. Health. 11, 1239228. https://doi.org/10.3389/fpubh.2023.1239228 (2023).
Allegranzi, B. et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377, 228–241. https://doi.org/10.1016/S0140-6736(10)61458-4 (2011).
Gidey, K., Gidey, M. T., Hailu, B. Y., Gebreamlak, Z. B. & Niriayo, Y. L. Clinical and economic burden of healthcare-associated infections: A prospective cohort study. PLoS One. 18, e0282141. https://doi.org/10.1371/journal.pone.0282141 (2023).
Ng, W. K., Shaban, R. Z. & van de Mortel, T. Healthcare professionals’ hand hygiene knowledge and beliefs in the united Arab Emirates. J. Infect. Prev. 18, 134–142. https://doi.org/10.1177/1757177416677851 (2017).
Sands, M. & Aunger, R. Determinants of hand hygiene compliance among nurses in US hospitals: A formative research study. PLoS One. 15, e0230573. https://doi.org/10.1371/journal.pone.0230573 (2020).
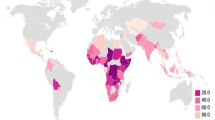
Loftus, M. J. et al. Hand hygiene in low-and middle-income countries. Int. J. Infect. Dis. 86, 25–30. https://doi.org/10.1016/j.ijid.2019.06.002 (2019).
Chakma, S. K. et al. Effectiveness of a hand hygiene training intervention in improving knowledge and compliance rate among healthcare workers in a respiratory disease hospital. Heliyon 2024;10. https://doi.org/10.1016/j.heliyon.2024.e27286
Ni, L. et al. An interventional implementation project: hand hygiene improvement. Ann. Transl Med. 2020;8. https://doi.org/10.21037/atm-20-5480
Hasan, Y. S. A. & Hussein, S. A. Nursing on the brink: somalia’s silent health crisis. Ethics Med. Public. Health. 33, 101093. https://doi.org/10.1016/j.jemep.2025.101093 (2025).
Jalei, A. A., Hassan, Y. S. A., Omar, A. I. & Ali, M. A. Patient satisfaction and health services in two public hospitals in Mogadishu, somalia: a cross-sectional study. Front. Health Serv. 2025;5. https://doi.org/10.3389/frhs.2025.1552322
Said, A. S. & Kicha, D. I. Implementing health system and the new federalism in somalia: challenges and opportunities. Front. Public. Health. 12, 1205327. https://doi.org/10.3389/fpubh.2024.1205327 (2024).
Wetzker, W. et al. Compliance with hand hygiene: reference data from the National hand hygiene campaign in Germany. J. Hosp. Infect. 92, 328–331. https://doi.org/10.1016/j.jhin.2016.01.022 (2016).
Steere, A. C. & Mallison, G. F. Handwashing practices for the prevention of nosocomial infections. Ann. Intern. Med. 83, 683–690. https://doi.org/10.7326/0003-4819-83-5-683 (1975).
Hassan, Y. S. A., Hassan, S. A. & Ahmed, N. R. Uptake of hepatitis B vaccination and associated factors among health sciences students, Mogadishu, Somalia. Front. Public. Health 2023;11. https://doi.org/10.3389/fpubh.2023.1203519
Sample Size Calculator - SurveyMonkey. n.d. accessed October 24, (2024). https://www.surveymonkey.com/mp/sample-size-calculator/
Karadağ, M., Yıldırım, N. & İşeri, Ö. The validity and reliability study of hand hygiene belief scale and hand hygiene practices inventory. Cukurova Med. J. 41, 271–284. https://doi.org/10.17826/cutf.237742 (2016).
van de Mortel, T. Development of a questionnaire to assess health care students’ hand hygiene knowledge, beliefs and practices. Australian J. Adv. Nurs. The. 26, 9–16. https://doi.org/10.37464/2009.263.1757 (2009).
Engdaw, G. T., Gebrehiwot, M. & Andualem, Z. Hand hygiene compliance and associated factors among health care providers in central Gondar zone public primary hospitals, Northwest Ethiopia. Antimicrob. Resist. Infect. Control. 8, 1–7. https://doi.org/10.1186/s13756-019-0634-z (2019).
Drey, N. et al. Applying thematic synthesis to interpretation and commentary in epidemiological studies: identifying what contributes to successful interventions to promote hand hygiene in patient care. BMJ Qual. Saf. 29, 756–763. https://doi.org/10.1136/bmjqs-2019-009833 (2020).
Umar, H. et al. Hand hygiene compliance and associated factor among nurses working in public hospitals of Hararghe zones, oromia region, Eastern Ethiopia. Front. Public. Health. 10, 1032167. https://doi.org/10.3389/fpubh.2022.1032167 (2022).
Tadesse, M., Shimelash, A. & Tegegne, E. Level of hand hygiene compliance and its associated factors among health care workers at Eka Kotebe general Hospital, addis Ababa, Ethiopia. Environ. Health Insights. 16, 117863022211136. https://doi.org/10.1177/11786302221113673 (2022).
Battistella, G., Berto, G. & Bazzo, S. Developing professional habits of hand hygiene in intensive care settings: an action-research intervention. Intensive Crit. Care Nurs. 38, 53–59. https://doi.org/10.1016/j.iccn.2016.08.003 (2017).
Acknowledgements
The authors sincerely thank all individuals and teams contributing to the data collection process. Furthermore, the authors thank Abdifatah Abdullahi Jalei for his valuable support and constructive feedback during the review of the methodological section and the preparation of the manuscript. Lastly, the authors are profoundly grateful to all participants for their time and significant contributions, without which this research would not have been feasible.
Author information
Authors and Affiliations
Contributions
Figen Balcioglu contributed to the conceptualization, methodology, supervision, and preparation of the original draft of the study. Marian Muse Osman was involved in investigation, formal analysis, manuscript review and editing. Tigad Abdisad ALI handled data curation, investigation, and project administration. Suad Abdikarim ISSE participated in data collection and contributed to the review and editing of the manuscript. Ahmed DOGAN was responsible for software, validation, and visualization. Ali Kutta Celik contributed to the formal analysis, provided resources, and assisted with the review and editing. Fadumo Nur Adan supported the investigation and data curation. Fartuun Ahmed Mahmud contributed to project administration and supervision. Yahye Sheikh Abdulle Hassan led the conceptualization, performed all data analysis, conducted formal analysis, supervised, and served as the corresponding author.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Balcioğlu, F., Osman, M.M., Ali, T.A. et al. Evaluation of hand hygiene belief and practice among healthcare workers at tertiary hospital, mogadishu, somalia: a cross-sectional study. Sci Rep (2026). https://doi.org/10.1038/s41598-025-34843-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-34843-1