Abstract
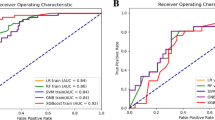
To determine whether there are radiomic ultrasound features of early pregnancy when viability is unknown, which in combination with clinical features, may predict subsequent loss. Multi-centre retrospective cohort study, which included 500 cases of pregnancies of unknown viability (PUV) collected from January 2021 to January 2023. Longitudinal ultrasound images were identified from Queen Charlotte’s and Chelsea Hospital (QCCH), London (n = 400, split 8:2 for training and validation) and St Mary’s Hospital (SMH), London (test data set n = 100). Images were extracted and segmented to include firstly the gestation sac and secondly the sac endometrial border. A segmentation model was developed using a deep learning (DL) model (multi-task nnUNet v2) and standard Dice Coefficient (DICE) was used to measure performance. A prediction model, using clinical and radiomic features, was developed by comparing several machine learning (ML) methods. The area under the ROC curve (AUC), F1-score, and recall were used to assess model performance. The QCCH and SMH data sets were in the majority well matched and consisted of 53.3% and 53.0% miscarriage cases by the end of first trimester, respectively. The DL segmentation model for gestation sac achieved a mean DICE score of 0.950 and 0.940 in the training and test data sets respectively. The segmentation model for the sac endometrial border achieved a mean DICE score of 0.917 (QCCH) and 0.922 (SMH). The best performing PUV outcome classification model (XGBoost and LASSO) for predicting miscarriage (PUVPS model); achieved an AUC of 1.00 (F1-score 1.00), 0.92 (F1-score 0.79) and 0.84 (F1-score 0.76) in the QCCH training, QCCH validation and SMH test set respectively. We have developed an end-to-end radiomics-based model to segment and predict early pregnancy outcomes. The main limitation of this study is its sample size, which can make a ML model prone to overfitting. This study sets the stage for future trials to prospectively evaluate the performance of the PUVPS model, in a large multi-centre cohort, which can then be used to help patients navigate the uncertainty of a PUV early pregnancy classification.
Similar content being viewed by others
Data availability
The anonymised adnexal image datasets and corresponding clinical metadata used for model development and validation in this study are not publicly available due to privacy and ethical considerations. However, thesedatasets can be made accessible to qualified researchers upon reasonable request to the corresponding author.
References
Farren, J. et al. Posttraumatic stress, anxiety and depression following miscarriage and ectopic pregnancy: a multicenter, prospective, cohort study. Am. J. Obstet. Gynecol. 222 (4), 367e1–e22 (2020).
Kong, G. W. et al. Clinical and psychological impact after surgical, medical or expectant management of first-trimester miscarriage–a randomised controlled trial. Aust N Z. J. Obstet. Gynaecol. 53 (2), 170–177 (2013).
Rai, R. & Regan, L. Recurrent miscarriage. Lancet 368 (9535), 601–611 (2006).
Mulik, V., Bethel, J. & Bhal, K. A retrospective population-based study of primigravid women on the potential effect of threatened miscarriage on obstetric outcome. J. Obstet. Gynaecol. 24 (3), 249–253 (2004).
NICE. Ectopic pregnancy and miscarriage: diagnosis and initial management. NG 126: National Institute Clinical Excellence (2019).
Bottomley, C. et al. Accurate prediction of pregnancy viability by means of a simple scoring system. Hum. Reprod. 28 (1), 68–76 (2013).
Liu, L. et al. Intelligent quality assessment of ultrasound images for fetal nuchal translucency measurement during the first trimester of pregnancy based on deep learning models. BMC Pregnancy Childbirth. 25 (1), 741 (2025).
Hunter, B. et al. Radiomics-based decision support tool assists radiologists in small lung nodule classification and improves lung cancer early diagnosis. Br. J. Cancer. 129 (12), 1949–1955 (2023).
Crispin-Ortuzar, M. et al. Integrated radiogenomics models predict response to neoadjuvant chemotherapy in high grade serous ovarian cancer. Nat. Commun. 14 (1), 6756 (2023).
Amiri, M. & Ramezani Tehrani, F. Potential adverse effects of female and male obesity on fertility: A narrative review. Int. J. Endocrinol. Metab. 18 (3), e101776 (2020).
Boxem, A. J. et al. Preconception and Early-Pregnancy body mass index in women and Men, time to Pregnancy, and risk of miscarriage. JAMA Netw. Open. 7 (9), e2436157–e (2024).
Murugesu, S. et al. Does advanced paternal age affect outcomes following assisted reproductive technology? A systematic review and meta-analysis. Reprod. Biomed. Online. 45 (2), 283–331 (2022).
Barcroft, J. F. et al. Machine learning and radiomics for segmentation and classification of adnexal masses on ultrasound. NPJ Precis Oncol. 8 (1), 41 (2024).
Falco, P. et al. Sonography of pregnancies with first-trimester bleeding and a small intrauterine gestational sac without a demonstrable embryo. Ultrasound Obstet. Gynecol. 21 (1), 62–65 (2003).
Liu, C., Wei, X. & Wang, F. The predictive value of ultrasound markers for pregnancy outcomes in recurrent pregnancy loss: a retrospective study. Sci. Rep. 14 (1), 16657 (2024).
Bottomley, C. et al. The optimal timing of an ultrasound scan to assess the location and viability of an early pregnancy. Hum. Reprod. 24 (8), 1811–1817 (2009).
Al-Memar, M. et al. Using simple clinical and ultrasound variables to develop a model to predict first trimester pregnancy viability. Eur. J. Obstet. Gynecol. Reprod. Biol. 292, 187–193 (2024).
Magnus, M. C., Wilcox, A. J., Morken, N. H., Weinberg, C. R. & Håberg, S. E. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ 364, l869 (2019).
Elmerdahl Frederiksen, L. et al. Maternal age and the risk of fetal aneuploidy: A nationwide cohort study of more than 500 000 Singleton pregnancies in Denmark from 2008 to 2017. Acta Obstet. Gynecol. Scand. 103 (2), 351–359 (2024).
Bottomley, C. et al. A model and scoring system to predict outcome of intrauterine pregnancies of uncertain viability. Ultrasound Obstet. Gynecol. 37 (5), 588–595 (2011).
Guha, S. et al. External validation of models and simple scoring systems to predict miscarriage in intrauterine pregnancies of uncertain viability. Hum. Reprod. 28 (11), 2905–2911 (2013).
Wan, O. Y. K. et al. External validation of a simple scoring system to predict pregnancy viability in women presenting to an early pregnancy assessment clinic. Hong Kong Med. J. 26 (2), 102–110 (2020).
Elson, J. et al. Prediction of early pregnancy viability in the absence of an ultrasonically detectable embryo. Ultrasound Obstet. Gynecol. 21 (1), 57–61 (2003).
Lautmann, K. et al. Clinical use of a model to predict the viability of early intrauterine pregnancies when no embryo is visible on ultrasound. Hum. Reprod. 26 (11), 2957–2963 (2011).
Chen, Y. et al. Deep learning radiomics of preoperative breast MRI for prediction of axillary lymph node metastasis in breast cancer. J. Digit. Imaging. 36 (4), 1323–1331 (2023).
Laqua, F. C. et al. Transfer-Learning deep radiomics and Hand-Crafted radiomics for classifying lymph nodes from Contrast-Enhanced computed tomography in lung cancer. Cancers (Basel) ; 15(10). (2023).
Quan, M. Y. et al. Deep learning radiomics model based on breast ultrasound video to predict HER2 expression status. Front. Endocrinol. (Lausanne). 14, 1144812 (2023).
Lawson, K., Bourne, T. & Bottomley, C. Psychological impact of simple scoring system for predicting early pregnancy outcome in pregnancy of uncertain viability: randomized controlled trial. Ultrasound Obstet. Gynecol. 61 (5), 624–631 (2023).
Funding
SM was supported by Imperial Health Charity and NIHR Imperial BRC. TB is supported by the National Institute for Health Research(NIHR) Biomedical Research Centre based at Imperial College Healthcare NHS Trust and Imperial College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The Tommy’s National Centre for Miscarriage Research at Imperial College NHS Trust is supported by the Tommy’s charity. EA receives funding from the Imperial College Biomedical Research Centre and Experimental Cancer Medicines Centre, paid to his institution. Tom Bourne and Eric Aboagye provided joint supervision for this work.
Author information
Authors and Affiliations
Contributions
S.M., K.L-R., E.A. and T.B. were involved in the study design. S.M., J.B. and M.P. collected the data. S.M. and K.L-R. analysed and interpreted the data. S.M. undertook literature review and wrote the initial draft. S.M. and K.L-R. undertook statistical and machine-learning analysis. T.B. and S.S. provided clinical advice. All authors reviewed, contributed to, and approved the manuscript. All authors had access to the data. S.M., K.L-R., E.A. and T.B. were responsible for the decision to submit the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Health Research Authority, Research Ethics Committee (HRA REC Reference 22/HRA/4847). All methods were performed in accordance with the guidelines and regulations outlined within the approved study protocol. Due to the retrospective nature of the study, written informed consent was not required based on national research guidance, confirmed by the Research Governance and Integrity Team Imperial College London and approved by the HRA REC committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murugesu, S., Linton-Reid, K., Barcroft, J. et al. Radiomics analysis of early pregnancy ultrasound images to predict viability at the end of first trimester. Sci Rep (2026). https://doi.org/10.1038/s41598-026-35158-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-35158-5