Abstract
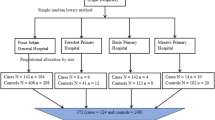
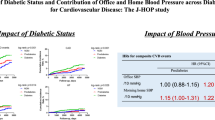
The risk of cardiovascular diseases (CVDs) is significantly increased when diabetes mellitus and hypertension coexist. Improving the clinical management of people with hypertension requires understanding the prevalence of diabetes in these patients. We conducted a cross-sectional analysis of 5,935 adults with hypertension who participated in the STEPwise approach to non-communicable diseases (NCD) risk factor surveillance (STEPS) 2021 of Iran. Diabetes mellitus was defined as fasting plasma glucose ≥ 126 mg/dL or current use of anti-hyperglycemic medication. Prediabetes was defined as 100 ≤ FPG < 126 without current anti-hyperglycemic medication use. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, or a history of anti-hypertensive treatment. Using logistic regression, we found characteristics associated with diabetes prevalence, while linear regression assessed the impact of diabetes status on systolic and diastolic blood pressure. Survey weights were utilized to ensure representativeness. Among individuals with hypertension, 25.3% (95% CI: 23.69–26.92) had diabetes, and 29.7% (95% CI: 27.93–31.45) had prediabetes. Of the diabetic patients, 20.7% achieved good glycemic control, 50.3% had uncontrolled diabetes, 7.8% were untreated, and 21.2% were undiagnosed. Diabetes was significantly more prevalent in those with cardiovascular disease (adjusted odds ratio (AOR) = 1.45, 95% CI: 1.14–1.84), chronic renal disease (1.74, 1.42–2.14), and dyslipidemia (1.83, 1.23–2.72). A positive family history of diabetes was significantly strong predictor (3.06, 2.53–3.69). Older age, urban residency, higher waist circumference, better diet quality, and hypertension treatment were also associated with increased diabetes risk. DBP was significantly lower in individuals with controlled diabetes (expected mean difference (EMD)= -2.52, 95% CI: -4.6 to -0.44) and treated but uncontrolled diabetes (EMD − 2.13, -3.77 to -0.48), while SBP was significantly higher in individuals with undiagnosed diabetes (EMD 4.76, 0.28–9.24). Diabetes and prediabetes are common among people with hypertension, with significant gaps in glycemic control. Early detection and improved management of both blood pressure and blood sugar levels are essential to reduce the burden of CVDs. Public health initiatives must prioritize targeted interventions for high-risk groups to effectively enhance diabetes management among individuals with hypertension.
Similar content being viewed by others
Data availability
The data of this study are available from the corresponding author on reasonable request.
Abbreviations
- ACE:
-
Angiotensin-Converting Enzyme
- ARB:
-
Angiotensin Receptor Blocker
- AOR:
-
Adjusted Odds Ratio
- BMI:
-
Body Mass Index
- CKD:
-
Chronic Kidney Disease
- CI:
-
Confidence Interval
- CVDs:
-
Cardiovascular Diseases
- CHD:
-
Coronary Heart Disease
- DBP:
-
Diastolic Blood Pressure
- DPP-4:
-
Dipeptidyl Peptidase-4
- eGFR:
-
Estimated Glomerular Filtration Rate
- EMD:
-
Expected mean difference
- FBS:
-
Fasting Blood Sugar
- FPG:
-
Fasting Plasma Glucose
- GLP-1 RA:
-
Glucagon-Like Peptide-1 Receptor Agonist
- HbA1c:
-
Glycosylated Hemoglobin
- HDL-C:
-
High-Density Lipoprotein Cholesterol
- HTN:
-
Hypertension
- LDL-C:
-
Low-Density Lipoprotein Cholesterol
- MR:
-
Mendelian Randomization
- NCD:
-
Non-Communicable Diseases
- NCEP ATP III:
-
National Cholesterol Education Program, Adult Treatment Panel III
- OGTT:
-
Oral Glucose Tolerance Test
- SBP:
-
Systolic Blood Pressure
- SGLT2-i:
-
Sodium-Glucose Cotransporter-2 Inhibitor
- TC:
-
Total Cholesterol
- TG:
-
Triglycerides
- UACR:
-
Urine Albumin-to-Creatinine Ratio
- WHO:
-
World Health Organization
- GPAQ:
-
Global Physical Activity Questionnaire
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76 (25), 2982–3021 (2020).
Zhou, B. et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398 (10304), 957–980 (2021).
Zhou, B. et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 389 (10064), 37–55 (2017).
Heidari-Foroozan, M. et al. Hypertension prevalence and cascade of care in Iran: Updates from the STEPs 2021 national and subnational survey. (2024).
Sun, H. et al. IDF diabetes atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Ameli, A. et al. The diabetes cascade of care through the 14 years in iran: findings of nationwide STEPS surveys 2007–2021. J. Diabetes Metabolic Disorders. 22 (2), 1731–1743 (2023).
Hazar, N., Jokar, M., Namavari, N., Hosseini, S. & Rahmanian, V. An updated systematic review and Meta-analysis of the prevalence of type 2 diabetes in Iran, 1996–2023. Front. public. Health. 12, 1322072 (2024).
Yildiz, M., Esenboğa, K. & Oktay, A. A. Hypertension and diabetes mellitus: highlights of a complex relationship. Curr. Opin. Cardiol. 35(4), 397–404 (2020).
Wang, F., Han, L. & Hu, D. Fasting insulin, insulin resistance and risk of hypertension in the general population: A meta-analysis. Clin. Chim. Acta. 464, 57–63 (2017).
Tatsumi, Y. & Ohkubo, T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens. Res. 40 (9), 795–806 (2017).
Mancusi, C. et al. Insulin resistance the hinge between hypertension and type 2 diabetes. High. Blood Press. Cardiovasc. Prev. 27, 515–526 (2020).
Huang, X. et al. Prevalence of diabetes and unrecognized diabetes in hypertensive patients aged 40 to 79 years in Southwest China. PloS One. 12 (2), e0170250 (2017).
Arauz-Pacheco, C., Parrott, M. A. & Raskin, P. Hypertension management in adults with diabetes. Diabetes Care. 27, S65 (2004).
Wang, Z., Yang, T. & Fu, H. Prevalence of diabetes and hypertension and their interaction effects on cardio-cerebrovascular diseases: a cross-sectional study. BMC Public. Health. 21 (1), 1224 (2021).
Behnoush, A. H. et al. Blood Pressure Control among Diabetic Patients in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis (Curr Diabetes Rev, 2024).
Bakris, G. L. Maximizing cardiorenal benefit in the management of hypertension: achieve blood pressure goals. J. Clin. Hypertens. (Greenwich). 1 (2), 141–147 (1999).
Colosia, A. D., Palencia, R. & Khan, S. Prevalence of hypertension and obesity in patients with type 2 diabetes mellitus in observational studies: a systematic literature review. Diabetes Metab. Syndr. Obes. 6, 327–338 (2013).
Djalalinia, S. et al. Protocol design for surveillance of risk factors of Non-communicable diseases during the COVID-19 pandemic: an experience from Iran STEPS survey 2021. Arch. Iran. Med. 25, 634–646 (2022).
Riley, L. et al. The world health organization STEPwise approach to noncommunicable disease risk-factor surveillance: methods, challenges, and opportunities. Am. J. Public Health. 106 (1), 74–78 (2016).
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint National committee (JNC 8). JAMA 311(5), 507–520 (2014).
Organization, W. H. WHO STEPS Surveillance Manual: the WHO STEPwise Approach To Chronic Disease Risk Factor Surveillance (World Health Organization, 2005).
Association, A. D. 2. Classification and diagnosis of diabetes: standards of medical care in Diabetes—2021. Diabetes Care. 44 (Supplement_1), S15–S33 (2020).
Azizi, F. et al. Appropriate waist circumference cut-off points among Iranian adults: the first report of the Iranian National committee of obesity. Arch. Iran. Med. 13 (3), 243–244 (2010).
Armstrong, T. & Bull, F. Development of the world health organization global physical activity questionnaire (GPAQ). J. Public Health. 14, 66–70 (2006).
WHO. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. Available from: https://www.who.int/docs/default-source/ncds/ncd-surveillance/gpaq-analysis-guide.pdf (2021).
Levey, A. S. et al. Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 67 (6), 2089–2100 (2005).
Cleeman, J. I. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). (2001).
Hedayatnia, M. et al. Dyslipidemia and cardiovascular disease risk among the MASHAD study population. Lipids Health Dis. 19, 1–11 (2020).
Lumley, T. Analysis of complex survey samples. J. Stat. Softw. 9, 1–19 (2004).
Jafari, A. et al. Cardiometabolic risk factors trend in Iranian adults with hypertension over 15 years: findings of nationwide steps of 2007–2021. J. Diabetes Metab. Disord. 23(2), 2315–2328 (2024).
Kramer, C. K., von Mühlen, D. & Barrett-Connor, E. Mid-life blood pressure levels and the 8-year incidence of type 2 diabetes mellitus: the rancho Bernardo study. J. Hum. Hypertens. 24 (8), 519–524 (2010).
Conen, D. et al. Blood pressure and risk of developing type 2 diabetes mellitus: the women’s health study. Eur. Heart J. 28 (23), 2937–2943 (2007).
DeFronzo, R. A. & Ferrannini, E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 14 (3), 173–194 (1991).
Ferrannini, E. et al. Insulin resistance in essential hypertension. N Engl. J. Med. 317 (6), 350–357 (1987).
Derakhshan, A. et al. Different combinations of glucose tolerance and blood pressure status and incident Diabetes, Hypertension, and chronic kidney disease. J. Am. Heart Assoc. 5(8), e003917 (2016).
Sun, D. et al. Type 2 diabetes and hypertension. Circul. Res. 124 (6), 930–937 (2019).
Wu, Y. et al. Association of hypertension and incident diabetes in Chinese adults: a retrospective cohort study using propensity-score matching. BMC Endocr. Disorders. 21 (1), 87 (2021).
Emdin Connor, A. et al. Usual blood pressure and risk of New-Onset diabetes. J. Am. Coll. Cardiol. 66 (14), 1552–1562 (2015).
Landsberg, L. & Molitch, M. Diabetes and hypertension: Pathogenesis, prevention and treatment. Clin. Exp. Hypertens. 26 (7–8), 621–628 (2004).
Mirahmadizadeh, A. et al. The prevalence of undiagnosed type 2 diabetes and prediabetes in Eastern mediterranean region (EMRO): a systematic review and meta-analysis. Diabetes Res. Clin. Pract. 160, 107931 (2020).
García-Puig, J. et al. Glucose metabolism in patients with essential hypertension. Am. J. Med. 119 (4), 318–326 (2006).
Liu, J. et al. Prevalence of diabetes mellitus in outpatients with essential hypertension in china: a cross-sectional study. BMJ open. 3 (11), e003798 (2013).
Qin, X. et al. Prevalence and associated factors of diabetes and impaired fasting glucose in Chinese hypertensive adults aged 45 to 75 years. PLoS One 7(8), e42538 (2012).
Danaei, G. et al. Effects of diabetes definition on global surveillance of diabetes prevalence and diagnosis:a pooled analysis of 96 population-based studies with 331 288 participants. Lancet Diabetes Endocrinol. 3 (8), 624–637 (2015).
Hare, M. J., Shaw, J. E. & Zimmet, P. Z. Current controversies in the use of haemoglobin A1c. J. Intern. Med. 271 (3), 227–236 (2012).
Azadnajafabad, S. et al. Evaluation of the diabetes care cascade and compliance with WHO global coverage targets in Iran based on STEPS survey 2021. Sci. Rep. 13 (1), 13528 (2023).
Alzaheb, R. A. & Altemani, A. H. The prevalence and determinants of poor glycemic control among adults with type 2 diabetes mellitus in Saudi Arabia. Diabetes, metabolic syndrome and obesity: targets and therapy, 15–21. (2018).
Borgharkar, S. S. & Das, S. S. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in india: the TIGHT study. BMJ Open. Diabetes Res. Care. 7 (1), e000654 (2019).
Fang, M. et al. Trends in diabetes treatment and control in US adults, 1999–2018. N. Engl. J. Med. 384 (23), 2219–2228 (2021).
Elliott, W. J. & Meyer, P. M. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 369 (9557), 201–207 (2007).
McClure, S. T. et al. Dietary intake of adults with and without diabetes: results from NHANES 2013–2016. BMJ Open. Diabetes Res. Care. 8 (1), e001681 (2020).
Jannasch, F., Kröger, J. & Schulze, M. B. Dietary patterns and type 2 diabetes: A systematic literature review and Meta-Analysis of prospective Studies12. J. Nutr. 147 (6), 1174–1182 (2017).
Muleta, S. et al. Blood pressure control and its determinants among diabetes mellitus co-morbid hypertensive patients at Jimma university medical center, South West Ethiopia. Clin. Hypertens. 23, 1–9 (2017).
Dedefo, M. G. et al. Blood pressure control among hypertensive diabetic patients on Follow-Up at chronic clinic of Nekemte referral hospital in West Ethiopia. Int. J. Hypertens. 2020 (1), 7526257 (2020).
Yamada, M. H. et al. Associations of systolic blood pressure and diastolic blood pressure with the incidence of coronary artery disease or cerebrovascular disease according to glucose status. Diabetes Care. 44 (9), 2124–2131 (2021).
Duggirala, M. K. et al. Predictors of blood pressure control in patients with diabetes and hypertension seen in primary care Clinics*. Am. J. Hypertens. 18 (6), 833–838 (2005).
Liakos, C. I. et al. Blood Pressure-Lowering effect of newer antihyperglycemic agents (SGLT-2 Inhibitors, GLP-1 receptor Agonists, and DPP-4 Inhibitors). Am. J. Cardiovasc. Drugs. 21 (2), 123–137 (2021).
Stanciu, S. et al. Links between metabolic syndrome and hypertension: the relationship with the current antidiabetic drugs. Metabolites 13 (1), 87 (2023).
Qayyum, R. & Adomaityte, J. A meta-analysis of the effect of Thiazolidinediones on blood pressure. J. Clin. Hypertens. 8 (1), 19–28 (2006).
Ilias, I. et al. Antidiabetic drugs and blood pressure changes. Pharmacol. Res. 161, 105108 (2020).
Acknowledgements
This study was supported by I.R. Iran’s National Institute of Health Research, Tehran University of Medical Sciences, Iran. Contract NO: 241/M/9839. The authors wish to convey their appreciation to the Deputy of Research and Technology, the Deputy of Health at the Ministry of Health and Medical Education, the National Institute of Health Research, the World Health Organization, and numerous other scholars and experts in pertinent fields. Furthermore, we express our gratitude to all participants, as well as the scientific and executive collaborators from several medical research colleges who facilitated this event. The authors express their gratitude to the workers of the Non-Communicable Diseases Research Center of the Endocrinology and Metabolism Population Sciences Institute of Tehran University of Medical Sciences, especially Dr. Yosra Azizpour, for their unwavering collaboration.
Funding
Grant IDs 1403-2-221-73074 from the Endocrinology and Metabolism Population Sciences Institute at Tehran University of Medical Sciences in Tehran, Iran, funded this study. No part of the study’s planning, execution, analysis, or manuscript preparation was influenced by the funders.
Author information
Authors and Affiliations
Contributions
Conceptualization: O.T.-M., M.M., A.G., S.K.; Methodology: M.M., A.G., S.K., O.T.-M.; Formal analysis: M.M., A.G.; Investigation: N.R., M.M., A.G., S.K.; Resources: O.T.-M., N.R.; Data Curation: M.M., A.G.; Validation: M.M., A.G., 0.T.-M., N.R., N.P., M.L.; Writing - Original Draft: M.M., A.G.; Writing - Review and Editing: M.M., A.G., O.T.-M., S.K., N.R., N.P, M.L.; Supervision: O.T.-M.; Project administration: O.T.-M.; Funding acquisition: O.T.-M. All authors have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Proposal of the current study was approved by the Ethical Committee of Endocrinology and Metabolism Research Institute, Tehran University of Medical Sciences, Tehran, Iran (IR.TUMS.EMRI.REC.1403.071).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mirzad, M., Golestani, A., Khosravi, S. et al. Prevalence of diabetes/prediabetes and their associated risk factors among adults with hypertension from iran: a nationwide study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-35998-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-35998-1