Abstract
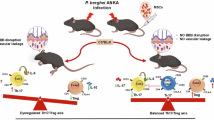
The signaling pathway activated by sphingosine-1-phosphate (S1P) through S1P receptor 1 (S1PR1) plays specific roles in regulating vascular integrity and preventing vascular leakage during inflammatory response. Endothelial cell barrier dysfunction has been implicated in cerebral malaria (CM) pathology. To explore the S1P/S1PR1 signaling pathway in CM, the study investigated the expression of S1PR1 in the brain of fatal malaria and correlated with the level of S1P and malaria severity. Localisation of S1PR1 in brain tissues was evaluated using immunohistochemistry technique in archived brain tissues of fatal P. falciparum malaria. S1P level was determined using enzyme-linked immunosorbent assay (ELISA). S1PR1 expression was intense in cerebral blood vessels and neurons of fatal CM patients compared to brain tissues from control group and non-CM patients (all p < 0.001). S1P level in the blood decreased significantly in CM group and was negatively correlated with S1PR1 expression in blood vessels and neurons. The expression of S1PR1 in cerebral blood vessels and neurons indicates that S1P/S1PR1 signaling pathway is involved in malaria pathogenesis and represents potential targets for S1P/S1PR1 modulators to treat CM. The outcomes can serve as a basis to explore measures to block the expression of S1PR1 which could reduce sequestration.
Similar content being viewed by others
Data availability
All data generated and analysed during the current study are included in this published articles and its supplementary information.
Abbreviations
- ABC:
-
Avidin–biotin complex
- BBB:
-
Blood brain barrier
- CM:
-
Cerebral malaria
- °C:
-
Degree Celsius
- DAB:
-
3,3'-Diaminobenzidine
- ECs:
-
Endothelial cells
- EDG1:
-
Endothelial differentiation gene 1
- ELISA:
-
Enzyme-linked immunosorbent assay
- Fig:
-
Figure
- FTY720:
-
Fingolimod hydrochloride
- Gi:
-
G protein alpha subunit
- h:
-
Hour
- H&E:
-
Haematoxylin and eosin
- HCl:
-
Hydrochloric acid
- HRP:
-
Horseradish peroxidase
- IFN-γ:
-
Interferon gamma
- IL:
-
Interleukin
- LPF:
-
Low power fields
- min:
-
Minute
- N:
-
Normal
- NCM:
-
Non-cerebral malaria
- p :
-
p-value
- pH:
-
Potential of hydrogen
- PRBCs:
-
Parasitized red blood cells
- RBCs:
-
Red blood cells
- r s :
-
Spearman’s rank correlation coefficient
- RT:
-
Room temperature
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SEM:
-
Standard error of the mean
- S1P:
-
Sphingosine-1-phosphate
- S1PR1:
-
Sphingosine-1-phosphate receptor 1
- SPSS:
-
Statistical Package for the Social Sciences
- TBS:
-
Tris-buffered saline
- TMB:
-
3, 3’, 5, 5’-Tetramethylbenzidine
- TNF:
-
Tumour necrosis factor
- TS:
-
Total score
- µm:
-
Micrometre
- µM:
-
Micromolar
References
Song, X. et al. Cerebral malaria induced by Plasmodium falciparum: clinical features, pathogenesis, diagnosis, and treatment. Front. Cell. Infect. Microbiol. 12, 939532. https://doi.org/10.3389/fcimb.2022.939532 (2022).
Solomon, W. et al. Neuregulin-1 attenuates mortality associated with experimental cerebral malaria. J. neuroinflammation. 11, 1–13. https://doi.org/10.1186/1742-2094-11-9 (2014).
Wiser, M. F. Knobs, adhesion, and severe falciparum malaria. Trop. Med. Infect. Dis. 8, 353. https://doi.org/10.3390/tropicalmed8070353 (2023).
Nishanth, G. & Schluter, D. Blood-brain barrier in cerebral malaria: Pathogenesis and therapeutic intervention. Trends Parasitol. 35, 516–528. https://doi.org/10.1016/j.pt.2019.04.010 (2019).
Leao, L. et al. Association of cerebral malaria and TNF-alpha levels: a systematic review. BMC Infect. Dis. 20, 442. https://doi.org/10.1186/s12879-020-05107-2 (2020).
Dunst, J., Kamena, F. & Matuschewski, K. Cytokines and chemokines in cerebral malaria pathogenesis. Front. Cell. Infect. Microbiol. 7, 324. https://doi.org/10.3389/fcimb.2017.00324 (2017).
Royo, J. et al. Elevated plasma interleukin-8 as a risk factor for mortality in children presenting with cerebral malaria. Infect. Dis. Poverty. 12, 8. https://doi.org/10.1186/s40249-023-01059-2 (2023).
Idro, R., Jenkins, N. E. & Newton, C. R. Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol. 4, 827–840. https://doi.org/10.1186/s40249-023-01059-210.1016/S1474-4422(05)70247-7 (2005).
Lyke, K. E. et al. Serum levels of the proinflammatory cytokines interleukin-1 beta (IL-1beta), IL-6, IL-8, IL-10, tumor necrosis factor alpha, and IL-12 (p70) in Malian children with severe Plasmodium falciparum malaria and matched uncomplicated malaria or healthy controls. Infect. Immun. 72, 5630–5637. https://doi.org/10.1128/IAI.72.10.5630-5637.2004 (2004).
Mshana, R. N., Boulandi, J., Mshana, N. M., Mayombo, J. & Mendome, G. Cytokines in the pathogenesis of malaria: levels of IL-I beta, IL-4, IL-6, TNF-alpha and IFN-gamma in plasma of healthy individuals and malaria patients in a holoendemic area. J Clin Lab Immunol. 34, 131–139 (1991).
Okamoto, Y., Wang, F., Yoshioka, K., Takuwa, N. & Takuwa, Y. Sphingosine-1-phosphate-specific G protein-coupled receptors as novel therapeutic targets for atherosclerosis. Pharmaceuticals. 4(1), 117–137. https://doi.org/10.3390/ph4010117 (2011).
Weigel, C., Bellaci, J. & Spiegel, S. Sphingosine-1-phosphate and its receptors in vascular endothelial and lymphatic barrier function. J. Biol. Chem. 299, 104775. https://doi.org/10.1016/j.jbc.2023.104775 (2023).
Chatzikonstantinou, S. et al. Signaling through the S1P–S1PR Axis in the gut, the immune and the central nervous system in multiple sclerosis: Implication for pathogenesis and treatment. Cells 10, 3217. https://doi.org/10.3390/cells10113217 (2021).
Ono, Y. et al. Sphingosine 1-phosphate release from platelets during clot formation: close correlation between platelet count and serum sphingosine 1-phosphate concentration. Lipids Health Dis. 12, 20. https://doi.org/10.1186/1476-511X-12-20 (2013).
Lucke, S. & Levkau, B. Endothelial functions of sphingosine-1-phosphate. Cell. Physiol. Biochem. 26, 87–96. https://doi.org/10.1159/000315109 (2010).
Mendelson, K., Evans, T. & Hla, T. Sphingosine 1-phosphate signalling. Development 141, 5–9. https://doi.org/10.1242/dev.094805 (2014).
Lee, M. J. et al. Vascular endothelial cell adherens junction assembly and morphogenesis induced by sphingosine-1-phosphate. Cell 99, 301–312. https://doi.org/10.1016/s0092-8674(00)81661-x (1999).
Garcia, J. G. et al. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J Clin Invest. 108, 689–701. https://doi.org/10.1172/JCI12450 (2001).
Yun, T. et al. Expression of sphingosine-1-phosphate receptor 1 in neuroinflammation of canine brains. Top. Companion Anim. Med. 60, 100847. https://doi.org/10.1016/j.tcam.2024.100847 (2024).
Iwasawa, E. et al. Sphingosine-1-phosphate receptor 1 activation enhances leptomeningeal collateral development and improves outcome after stroke in mice. J Stroke Cerebrovasc Dis. 27, 1237–1251. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.11.040 (2018).
Robert, P. et al. EDG1 receptor stimulation leads to cardiac hypertrophy in rat neonatal myocytes. J Mol Cell Cardiol. 33, 1589–1606. https://doi.org/10.1006/jmcc.2001.1433 (2001).
Punsawad, C., Maneerat, Y., Chaisri, U., Nantavisai, K. & Viriyavejakul, P. Nuclear factor kappa B modulates apoptosis in the brain endothelial cells and intravascular leukocytes of fatal cerebral malaria. Malar J. 12, 260. https://doi.org/10.1186/1475-2875-12-260 (2013).
Srisook, C., Glaharn, S., Punsawad, C. & Viriyavejakul, P. Apoptotic changes and aquaporin-1 expression in the choroid plexus of cerebral malaria patients. Malar J. 21, 43. https://doi.org/10.1186/s12936-022-04044-6 (2022).
Turner, G. Cerebral malaria. Brain Pathol. 7, 569–582. https://doi.org/10.1111/j.1750-3639.1997.tb01075.x (1997).
MacPherson, G. G., Warrell, M. J., White, N. J., Looareesuwan, S. & Warrell, D. A. Human cerebral malaria. A quantitative ultrastructural analysis of parasitized erythrocyte sequestration. Am. J. Pathol. 119, 385–401 (1985).
Prapansilp, P. et al. A clinicopathological correlation of the expression of the angiopoietin-Tie-2 receptor pathway in the brain of adults with Plasmodium falciparum malaria. Malar J. 12, 50. https://doi.org/10.1186/1475-2875-12-50 (2013).
Xiao, S., Peng, K., Li, C., Long, Y. & Yu, Q. The role of sphingosine-1-phosphate in autophagy and related disorders. Cell Death Discov. 9, 380. https://doi.org/10.1038/s41420-023-01681-x (2023).
Hashemi, E. et al. Visualizing Sphingosine-1-phosphate receptor 1 (S1PR1) signaling during central nervous system de- and remyelination. Cell. Mol. Neurobiol. 43, 1219–1236. https://doi.org/10.1007/s10571-022-01245-0 (2023).
Pyne, S. & Pyne, N. J. Sphingosine 1-phosphate signalling in mammalian cells. Biochem. J. 349, 385–402. https://doi.org/10.1042/0264-6021:3490385 (2000).
Gaire, B. P. & Choi, J. W. Sphingosine 1-phosphate receptors in cerebral ischemia. Neuromolecular Med. 23, 211–223. https://doi.org/10.1007/s12017-020-08614-2 (2021).
Garcia, J. G. et al. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J. Clin. Invest. 108, 689–701. https://doi.org/10.1172/JCI12450 (2001).
Modak, A. et al. Fingolimod (FTY720), an FDA-approved sphingosine 1-phosphate (S1P) receptor agonist, restores endothelial hyperpermeability in cellular and animal models of dengue virus serotype 2 infection. IUBMB Life 76, 267–285. https://doi.org/10.1002/iub.2795 (2024).
Camerer, E. et al. Sphingosine-1-phosphate in the plasma compartment regulates basal and inflammation-induced vascular leak in mice. J. Clin. Invest. 119, 1871–1879. https://doi.org/10.1172/jci38575 (2009).
Punsawad, C. & Viriyavejakul, P. Reduction in serum sphingosine 1-phosphate concentration in malaria. PLoS ONE 12, e0180631. https://doi.org/10.1371/journal.pone.0180631 (2017).
Sah, R. K. et al. Reduction of sphingosine kinase 1 phosphorylation and activity in plasmodium-infected erythrocytes. Front. Cell. Dev. Biol. 8, 80. https://doi.org/10.3389/fcell.2020.00080 (2020).
Finney, C. A. et al. S1P is associated with protection in human and experimental cerebral malaria. Mol Med. 17, 717–725. https://doi.org/10.2119/molmed.2010.00214 (2011).
Karam, M. & Auclair, C. Sphingosine-1-phosphate as lung and cardiac vasculature protecting agent in SARS-CoV-2 Infection. Int. J. Mol. Sci. 24, 13088. https://doi.org/10.3390/ijms241713088 (2023).
Winkler, M. S. et al. Erythrocytes increase endogenous sphingosine 1-phosphate levels as an adaptive response to SARS-CoV-2 infection. Clin. Sci (Lond) 135, 2781–2791. https://doi.org/10.1042/CS20210666 (2021).
Marfia, G. et al. Decreased serum level of sphingosine-1-phosphate: a novel predictor of clinical severity in COVID-19. EMBO Mol. Med. 13, 13424. https://doi.org/10.15252/emmm.202013424 (2021).
Gomes, L. et al. Sphingosine 1-phosphate in acute dengue infection. PLoS ONE 9, e113394. https://doi.org/10.1371/journal.pone.0113394 (2014).
Michels, M. et al. Decreased plasma levels of the endothelial protective sphingosine-1-phosphate are associated with dengue-induced plasma leakage. J. Infect. 71, 480–487. https://doi.org/10.1016/j.jinf.2015.06.014 (2015).
Winkler, M. S. et al. Loss of sphingosine 1-phosphate (S1P) in septic shock is predominantly caused by decreased levels of high-density lipoproteins (HDL). J. Intensive Care. 7, 23. https://doi.org/10.1186/s40560-019-0376-2 (2019).
Winkler, M. S. et al. Decreased serum concentrations of sphingosine-1-phosphate in sepsis. Crit Care. 19, 372. https://doi.org/10.1186/s13054-015-1089-0 (2015).
Bai, Q. et al. Serum sphingosine-1-phosphate level and peritonitis in peritoneal dialysis patients. Ren. Fail. 42, 829–835. https://doi.org/10.1080/0886022X.2020.1805763 (2020).
Yang, X. et al. Association of plasma sphingosine-1-phosphate levels with disease severity and prognosis after intracerebral hemorrhage. Front. Neurol. 15, 1365902. https://doi.org/10.3389/fneur.2024.1365902 (2024).
Hsu, S. C. et al. Circulating sphingosine-1-phosphate as a prognostic biomarker for community-acquired pneumonia. PLoS ONE 14, e0216963. https://doi.org/10.1371/journal.pone.0216963 (2019).
Zhao, Y. et al. Pathogenic sphingosine 1-phosphate pathway in psoriasis: a critical review of its pathogenic significance and potential as a therapeutic target. Lipids Health Dis. 22, 52. https://doi.org/10.1186/s12944-023-01813-3 (2023).
Ding, F., Wang, Z., Wang, J., Ma, Y. & Jin, J. Serum S1P level in interstitial lung disease (ILD) is a potential biomarker reflecting the severity of pulmonary function. BMC Pulm. Med. 24, 266. https://doi.org/10.1186/s12890-024-03081-y (2024).
Miura, K. et al. Dysregulation of sphingolipid metabolic enzymes leads to high levels of sphingosine-1-phosphate and ceramide in human hepatocellular carcinoma. Hepatol Res. 51, 614–626. https://doi.org/10.1111/hepr.13625 (2021).
Blachnio-Zabielska, A. U. et al. The Interplay between oxidative stress and sphingolipid metabolism in endometrial cancer. Int. J. Mol. Sci. 25. https://doi.org/10.3390/ijms251910243 (2024).
Oggungwan, K., Glaharn, S., Ampawong, S., Krudsood, S. & Viriyavejakul, P. FTY720 restores endothelial cell permeability induced by malaria sera. Sci. Rep. 8, 10959. https://doi.org/10.1038/s41598-018-28536-1 (2018).
Thompson, J. et al. Progressive disruption of sphingosine-1-phosphate receptor 1 correlates with blood-brain barrier leakage in a rat model of chronic hypoxic hypoperfusion. Aging Dis. 16, 2. https://doi.org/10.14336/AD.2024.0098 (2024).
Nacer, A. et al. Neuroimmunological blood brain barrier opening in experimental cerebral malaria. PLoS Pathog. 8, e1002982. https://doi.org/10.1371/journal.ppat.1002982 (2012).
Yang, L. X. et al. Sphingosine-1-phosphate receptor 1 regulates blood-brain barrier permeability in epileptic mice. Neural Regen. Res. 18, 1763–1769. https://doi.org/10.4103/1673-5374.360263 (2023).
Groves, A., Kihara, Y. & Chun, J. Fingolimod: direct CNS effects of sphingosine 1-phosphate (S1P) receptor modulation and implications in multiple sclerosis therapy. J. Neurol. Sci. 328, 9–18. https://doi.org/10.1016/j.jns.2013.02.011 (2013).
Burg, N., Salmon, J. E. & Hla, T. Sphingosine 1-phosphate receptor-targeted therapeutics in rheumatic diseases. Nat Rev Rheumatol. 18, 335–351. https://doi.org/10.1038/s41584-022-00784-6 (2022).
Patmanathan, S. N. et al. Mechanisms of sphingosine 1-phosphate receptor signalling in cancer. Cell Signal. 34, 66–75. https://doi.org/10.1016/j.cellsig.2017.03.002 (2017).
Jiang, H. et al. Quantitative Analysis of S1PR1 expression in the postmortem multiple sclerosis central nervous system. ACS Chem. Neurosci. 14, 4039–4050. https://doi.org/10.1021/acschemneuro.3c00581 (2023).
Nishimura, H., Akiyama, T., Irei, I., Hamazaki, S. & Sadahira, Y. Cellular localization of sphingosine-1-phosphate receptor 1 expression in the human central nervous system. J. Histochem. Cytochem. 58, 847–856. https://doi.org/10.1369/jhc.2010.956409 (2010).
Gao, P. et al. S1PR1 regulates NDV-induced IL-1beta expression via NLRP3/caspase-1 inflammasome. Vet Res. 53, 58. https://doi.org/10.1186/s13567-022-01078-1 (2022).
Chavez, A. et al. S1PR1 Tyr143 phosphorylation downregulates endothelial cell surface S1PR1 expression and responsiveness. J Cell Sci. 128, 878–887. https://doi.org/10.1242/jcs.154476 (2015).
Acknowledgements
Our gratitude goes to the Central Equipment Unit, Faculty of Tropical Medicine, Mahidol University, Thailand for facilitating the laboratory equipment. We thank all staff at the Department of Tropical Pathology, Faculty of Tropical Medicine, Mahidol University, Thailand for their support throughout this study.
Funding
This research project is supported by Faculty of Tropical Medicine, Mahidol University, Fiscal year 2011. RN is the grant recipient.
Author information
Authors and Affiliations
Contributions
P.V., C.S. and R.N. initiated the research idea, designed the experiments, gathered clinical data and retrieved archived paraffin blocks. P.V., C.S., R.N., C.P. and S.G. performed immunohistochemistry study. P.V., C.S., S.G. and T.T. worked on ELISA. All authors analysed the results, interpreted the data and drafted the manuscript. PV provided technical guidance, gave advices and revised the final manuscript. R.N. obtained funding, was affiliated with Department of Tropical Pathology, Faculty of Tropical Medicine, Mahidol University during the initial part of the research, and is currently an independent researcher. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was obtained from the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University (MUTM 2011-027-01, MUTM 2011-27-02: for using tissue specimens and MUTM 2024-033-01: for using left-over human sera).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Srisook, C., Nintasen, R., Punsawad, C. et al. Expression of sphingosine-1-phosphate receptor 1 in the brain of fatal cerebral malaria. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36072-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36072-6