Abstract
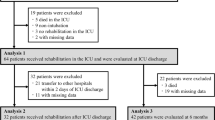
Emotional distress, including anxiety and sadness, is common among patients in the intensive care unit (ICU). It may be influenced by clinical factors but also by physical distress symptoms such as dyspnea and pain; however, trajectories of emotional and physical distress and interactions throughout the ICU stay, and their potential impact after discharge, remain relatively unexplored. The main objective of the study was to investigate the trajectory and interplay of anxiety, sadness, dyspnea, and pain during the ICU stay, and also their associations with clinical and demographic factors and with cognitive status at discharge. Observational, longitudinal study in non-delirious adult ICU patients in whom emotional state (anxiety and sadness) and physical discomfort (dyspnea and pain) were assessed daily using a visual analog scale, once an adequate level of consciousness (RASS between − 1 and + 1) had been achieved. A new variable was created to compare the evolution of distress in the different phases of admission. Mixed-effects models were used to explore associations with the phase of ICU stay, invasive mechanical ventilation (IMV), and other clinical variables. Cognitive status was assessed at ICU discharge with the MoCA test. In 62 ICU patients, levels of sadness consistently exceeded anxiety during ICU stay, although both remained stable and declined only in the final phase. IMV was associated with higher levels of sadness (β = 2.45, p < 0.001) and dyspnea (β = 1.24, p = 0.003). Male patients reported lower anxiety levels (β = − 1.34, p = 0.039). Pain correlated with sadness early in the ICU period (r = 0.44, p = 0.016), and with dyspnea during the second (r = 0.54, p = 0.001) and late phases (r = 0.34, p = 0.004). At ICU discharge, 70.9% of patients showed cognitive impairment unrelated to distress, clinical or demographic variables. Sadness was identified as a more prominent component of emotional distress than anxiety during the ICU stay. The findings underscore the impact of IMV on both sadness and dyspnea, highlighting the value of a multidimensional psychological assessment in critically ill patients. The lack of association between cognitive impairment at discharge and in-ICU emotional/physical distress trajectories suggests that cognitive and emotional sequelae may arise from distinct underlying mechanisms.
Trial registration: ClinicalTrials.gov (NCT07153380).
Similar content being viewed by others
Data availability
The dataset generated and analyzed during the current study is available in the RDR (Research Data Repository), a federated and multidisciplinary repository for Catalan universities, CERCA research centers, and other research institutions. RDR complies with the FAIR principles (Findable, Accessible, Interoperable, and Reusable) and follows the EOSC (European Open Science Cloud) guidelines. RDR will comply with the FAIR principles (Findable, Accessible, Interoperable, and Reusable) and will follow the EOSC (European Open Science Cloud) guidelines. The datasets generated and analyzed during the current study are available in the Cora RDR (Research Data Repository), (https://doi.org/10.34810/data2719). The files are available upon request.
References
Cardoso, G., Alexandre, J. & Rosa, A. Depression, anxiety and alcohol abuse in a gastroenterology intensive care unit: Prevalence and detection. Clin. Pract. Epidemiol. Ment. Health 6(1), 47–52 (2010).
Rincon, H. G. et al. Prevalence, detection and treatment of anxiety, depression, and delirium in the adult critical care unit. Psychosomatics 42(5), 391–396 (2001).
Shdaifat, S. A. & Al, Q. M. Anxiety and depression among patients admitted to intensive care. Nurs. Crit. Care 27(1), 106–112. https://doi.org/10.1111/nicc.12536 (2022).
Biancofiore, G. et al. Stress-inducing factors in ICUs: What liver transplant recipients experience and what caregivers perceive. Liver Transp. 11(8), 967–972 (2005).
Sher, Y., Desai, N., Sole, J. & D’souza, M. P. Dyspnea and dyspnea-associated anxiety in the ICU patient population: A narrative review for CL psychiatrists. J. Acad. Consult. Liaison Psychiatry 65(1), 54–65 (2024).
Granja, C. et al. Patients’ recollections of experiences in the intensive care unit may affect their quality of life. Crit. Care. 9(2), R96 (2005).
Myhren, H., Ekeberg, Ø., Tøien, K., Karlsson, S. & Stokland, O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit. Care 14(1), R14. https://doi.org/10.1186/cc8870 (2010).
Tøien, K. et al. Psychological distress after severe trauma: A prospective 1-year follow-up study of a trauma intensive care unit population. J. Trauma: Injury, Infect. Crit. Care. 69(6), 1552–1559 (2010).
Bjørnøy, I., Rustøen, T., Mesina, R. J. S. & Hofsø, K. Anxiety and depression in intensive care patients six months after admission to an intensive care unit: A cohort study. Intens. Crit. Care Nurs. 78, 103473 (2023).
Bonsaksen, T. et al. Self-diagnosed depression in the Norwegian general population – associations with neuroticism, extraversion, optimism, and general self-efficacy. BMC Public Health 18(1), 1076. https://doi.org/10.1186/s12889-018-5990-8 (2018).
Lee, M., Kang, J. & Jeong, Y. J. Risk factors for post–intensive care syndrome: A systematic review and meta-analysis. Aust. Crit. Care 33(3), 287–294 (2020).
Navarra-Ventura, G. et al. Occurrence, co-occurrence and persistence of symptoms of depression and post-traumatic stress disorder in survivors of COVID-19 critical illness. Eur. J. Psychotraumatol. 15(1), 2363654 (2024).
Fernández-Gonzalo, S. et al. Characterization of postintensive care syndrome in a prospective cohort of survivors of COVID-19 critical illness: A 12-month follow-up study. Can. J. Anesthesia/J. canadien d’anesthésie. 71(9), 1282–1301 (2024).
Wang, S. et al. Prevalence and risk factors of depression and anxiety symptoms in intensive care unit patients with cardiovascular disease: A cross-sectional study. J. Clin. Nurs. https://doi.org/10.1111/jocn.17203 (2024).
Hamilton, M. et al. Determinants of depressive symptoms at 1 year following ICU discharge in survivors of ≥ 7 days of mechanical ventilation. Chest 156(3), 466–476 (2019).
Yamamoto, H. et al. Physical function and mental health trajectories in COVID-19 patients following invasive mechanical ventilation: A prospective observational study. Sci. Rep. 13(1), 14529 (2023).
Schmidt, M. et al. Dyspnea in mechanically ventilated critically ill patients*. Crit Care Med. 39(9), 2059–2065 (2011).
Fukushi, I., Pokorski, M. & Okada, Y. Mechanisms underlying the sensation of dyspnea. Respir Investig. 59(1), 66–80 (2021).
Laviolette, L. & Laveneziana, P. Dyspnoea: A multidimensional and multidisciplinary approach. Eur. Respir. J. 43(6), 1750–1762 (2014).
von Leupoldt, A. Treating anxious expectations can improve dyspnoea in patients with COPD. Eur. Respir. J. 50(3), 1701352 (2017).
Similowski, T. Treat the lungs, fool the brain and appease the mind: Towards holistic care of patients who suffer from chronic respiratory diseases. Euro. Respirat. J. 51(2), 1800316. https://doi.org/10.1183/13993003.00316-2018 (2018).
Tan, Y., Van den Bergh, O., Qiu, J. & von Leupoldt, A. The impact of unpredictability on dyspnea perception, anxiety and interoceptive error processing. Front. Physiol. 10, 535. https://doi.org/10.3389/fphys.2019.00535/full (2019).
Demoule, A. et al. Prevalence, intensity, and clinical impact of dyspnea in critically ill patients receiving invasive ventilation. Am. J. Respir. Crit. Care Med. 205(8), 917–926. https://doi.org/10.1164/rccm.202108-1857OC (2022).
Persichini, R. et al. Diagnostic accuracy of respiratory distress observation scales as surrogates of Dyspnea self-report in intensive care unit patients. Anesthesiology 123(4), 830–837 (2015).
Worsham, C. M., Banzett, R. B. & Schwartzstein, R. M. Dyspnea, acute respiratory failure, psychological trauma, and post-ICU mental health: A caution and a call for research. Chest 159(2), 749–756 (2021).
Röser, E. et al. Differences between women and men in prolonged weaning. Respir. Res. 25(1), 363 (2024).
Szokol, J. W. & Vender, J. S. Anxiety, delirium, and pain in the intensive care unit. Crit. Care Clin. 17(4), 821–842 (2001).
Chanques, G. et al. A prospective study of pain at rest: Incidence and characteristics of an unrecognized symptom in surgical and trauma versus medical intensive care unit patients. Anesthesiology 107(5), 858–860 (2007).
Puntillo, K. A. et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am. J. Respir. Crit. Care Med. 189(1), 39–47. https://doi.org/10.1164/rccm.201306-1174OC (2014).
Oh, J. et al. Mutual relationship between anxiety and pain in the intensive care unit and its effect on medications. J. Crit. Care 30(5), 1043–1048 (2015).
Devlin, J. W. et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit. Care Med. 46(9), e825–e873 (2018).
Myhren, H. et al. Patients’ memory and psychological distress after ICU stay compared with expectations of the relatives. Intens. Care Med. 35(12), 2078. https://doi.org/10.1007/s00134-009-1614-1 (2009).
Cuthbertson, B. H., Hull, A., Strachan, M. & Scott, J. Post-traumatic stress disorder after critical illness requiring general intensive care. Intens. Care Med. 30(3), 450–455 (2004).
Ely, E. W. et al. Evaluation of delirium in critically ill patients: Validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. 29(7), 1370–1379 (2001).
Goldberg, T. E. et al. Association of delirium with long-term cognitive decline. JAMA Neurol. 77(11), 1373 (2020).
Sakuramoto, H., Subrina, J., Unoki, T., Mizutani, T. & Komatsu, H. Severity of delirium in the ICU is associated with short term cognitive impairment. A prospective cohort study. Intens. Crit. Care Nurs. 31(4), 250–257 (2015).
Ko, R. E. et al. Association between the presence of delirium during intensive care unit admission and cognitive impairment or psychiatric problems: The Korean ICU national data study. J Intensive Care. 10(1), 7 (2022).
Wu, T. T. et al. Baseline anxiety and depression and risk for ICU delirium: A prospective cohort study. Crit. Care Explor 4(7), e0743. https://doi.org/10.1097/CCE.0000000000000743 (2022).
Andrews, P. S. et al. Delirium, depression, and long-term cognition. Int. Psychogeriatr 35(8), 433–438 (2023).
Barros de Oliveira, S. H. & Lins Fumis, R. R. Sex and spouse conditions influence symptoms of anxiety, depression, and posttraumatic stress disorder in both patients admitted to intensive care units and their spouses. Rev. Bras Ter Intensiva 30(1), 35–41 (2018).
Skalski, C. A., DiGerolamo, L. & Gigliotti, E. Stressors in five client populations: Neuman systems model-based literature review. J Adv Nurs. 56(1), 69–78 (2006).
Castillo, M. I., Aitken, L. M. & Cooke, M. L. Study protocol: Intensive care anxiety and emotional recovery (Icare)—A prospective study. Aust. Crit. Care 26(3), 142–147 (2013).
Salem, A. & Ahmad, M. M. Communication with invasive mechanically ventilated patients and the use of alternative devices: integrative review. J. Res. Nurs. 23(7), 614–630 (2018).
Forcano García, M., Ortiz, P. & de Pinedo, F. Deterioro cognitivo: uso de la versión corta del test del informador (IQCODE) en consultas de geriatría. Rev Esp Geriatr Gerontol. 37(2), 81–85 (2002).
Wagner, D. P. & Draper, E. A. Acute physiology and chronic health evaluation (APACHE II) and medicare reimbursement. Health Care Financ. Rev. 1984(Suppl), 91 (1984).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 40(5), 373–383 (1987).
Tobar, E. et al. Método para la evaluación de la confusión en la unidad de cuidados intensivos para el diagnóstico de delírium: adaptación cultural y validación de la versión en idioma español. Med. Intensiva. 34(1), 4–13 (2010).
Joyce, C. R. B., Zutshi, D. W., Hrubes, V. & Mason, R. M. Comparison of fixed interval and visual analogue scales for rating chronic pain. Eur. J. Clin. Pharmacol. 8(6), 415–420. https://doi.org/10.1007/BF00562315 (1975).
Cao, X. et al. A novel visual facial anxiety scale for assessing preoperative anxiety. PLoS ONE 12(2), e0171233 (2017).
Boonstra, A. M., Schiphorst Preuper, H. R., Balk, G. A. & Stewart, R. E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 155(12), 2545–2550 (2014).
Nasreddine, Z. S. et al. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53(4), 695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x (2005).
Chahraoui, K., Laurent, A., Bioy, A. & Quenot, J. P. Psychological experience of patients 3 months after a stay in the intensive care unit: A descriptive and qualitative study. J. Crit. Care 30(3), 599–605 (2015).
Schwartzstein, R. M. & Campbell, M. L. Dyspnea and mechanical ventilation: The emperor has no clothes. Am. J. Respir. Crit. Care Med. 205(8), 864–865. https://doi.org/10.1164/rccm.202201-0078ED (2022).
Banzett, R. & Georgopoulos, D. Dyspnea in the ICU: It is difficult to see what patients feel. Am. J. Respir. Crit. Care Med. 208(1), 6–7. https://doi.org/10.1164/rccm.202304-0677ED (2023).
Christiansen, D. M. & Hansen, M. Accounting for sex differences in PTSD: A multi-variable mediation model. Eur. J. Psychotraumatol. 6(1), 26068. https://doi.org/10.3402/ejpt.v6.26068 (2015).
Ervin, J., Taouk, Y., Alfonzo, L. F., Hewitt, B. & King, T. Gender differences in the association between unpaid labour and mental health in employed adults: A systematic review. Lancet Public Health 7(9), e775–e786 (2022).
Lat, T. I., McGraw, M. K. & White, H. D. Gender differences in critical illness and critical care research. Clin. Chest. Med. 42(3), 543–555 (2021).
Bhardwaj, A., Sharma, M., Kumar, S., Sharma, S., Sharma, P. C. Transforming pediatric speech and language disorder diagnosis and therapy: The evolving role of artificial intelligence. health sciences review [Internet]. 2024 Jun; 100188. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2772632024000412
Rose, L., Muttalib, F. & Adhikari, N. K. J. Psychological consequences of admission to the ICU. JAMA 322(3), 213 (2019).
Demoule, A. et al. Dyspnoea in acutely ill mechanically ventilated adult patients: An ERS/ESICM statement. Intensive Care Med. 50(2), 159–180. https://doi.org/10.1007/s00134-023-07246-x (2024).
Kalfon, P. et al. Risk factors and events in the adult intensive care unit associated with pain as self-reported at the end of the intensive care unit stay. Crit. Care. 24(1), 685 (2020).
Filipovic-Grcic, I., Tonkovic, D., Grubisin, J., Peric, M. & Kogler, V. M. Hospital anxiety depression scale in our surgical ICU. Crit Care. 14(Suppl 1), P499 (2010).
Segernäs, A., Skoog, J., Ahlgren Andersson, E., Almerud Österberg, S., Thulesius, H., Zachrisson, H. Prediction of Postoperative Delirium After Cardiac Surgery with A Quick Test of Cognitive Speed, Mini-Mental State Examination and Hospital Anxiety and Depression Scale. Clin Interv Aging [Internet]. 2022 Apr; Volume 17:359–68. Available from: https://www.dovepress.com/prediction-of-postoperative-delirium-after-cardiac-surgery-with-a-quic-peer-reviewed-fulltext-article-CIA
Acknowledgements
The authors thank Michael Maudsley for his invaluable support in editing the manuscript. Special acknowledgements are due to all the patients who voluntarily agreed to participate in the study.
Funding
This work was supported by the Instituto de Salud Carlos III (ISCIII) under Grant number PI21/01592, La Marató 3CAT, under Grant numbers 202118 (413/C/2021) and 202214–30-31 (262/C/2022); CIBER -Consorcio Centro de Investigación Biomédica en Red- CB06/06/1097, ISCIII, Ministerio de Ciencia e Innovación and Unión Europea-European Regional Development Fund; CERCA Programme/Generalitat de Catalunya; and Fundació Institut d’Investigació i Innovació Parc Taulí-I3PT (CIR2017/032).
Author information
Authors and Affiliations
Contributions
EDL, MGG, AFO and SFG designed the study and the protocols. GG, JEE, CDH and EDS contributed in the sample recruitment and provided clinical expertise in designing the protocol. EDL, MGG, GNV, MJ and SFG provided psychological and neuropsychological advice in the design of the protocol. EDL, MGG, GNV and SFG performed the neuropsychological assessment. AFO, EDL and SFG performed the statistical analysis. EDL, SFG, LS, JLA and LB drafted the manuscript. All authors were involved in the interpretation of the results and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Data collection for each cohort was independently approved by the Institutional Review Board of the Parc Taulí University Hospital (2018/542, 2021/5088, 2022/6011). The reanalysis for the current project was approved. (2025/5057) and registered on ClinicalTrials.gov (NCT07153380) on September 3, 2025. All participants (or their authorized representatives) provided written informed consent prior to inclusion in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Doña-López, E., Godoy-González, M., Navarra-Ventura, G. et al. Trajectories of emotional and physical distress during ICU stay and their association with clinical factors and cognitive status at discharge. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36684-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36684-y