Abstract
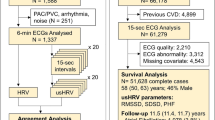
This study aims to evaluate and compare cardiac autonomic function, specifically through heart rate variability (HRV), between individuals with bronchiectasis and their age- and gender-matched healthy counterparts. This study employed a case-control design, involving 60 participants diagnosed with bronchiectasis (cases) and a control group of healthy individuals matched by age and gender. HRV data was collected over a five-minute interval, focusing on frequency domain parameters including total power, very low frequency (VLF), low frequency (LF), high frequency (HF), and the LF/HF ratio. The bronchiectasis group exhibited a significantly elevated LF/HF ratio, indicating a shift in cardiac sympathovagal balance, relative to the control group (2.25 ± 0.39 vs. 2.05 ± 0.38; p = 0.006). Additionally, marked differences were found in specific frequency domain parameters: LF (2.33 ± 0.55 vs. 2.55 ± 0.46; p = 0.021) and HF (2.06 ± 0.75 vs. 2.5 ± 0.56; p = 0.001). The results suggest a notable disturbance in cardiac autonomic regulation among individuals with bronchiectasis, compared to healthy individuals.
Similar content being viewed by others
Data availability
Research data will be available from the corresponding author with a reasonable request.
Abbreviations
- HRV:
-
Heart rate variability
- COPD:
-
Chronic obstructive pulmonary diseases
- BA:
-
Bronchial asthma
- PAH:
-
Pulmonary artery hypertension
- OSA:
-
Obstructive sleep apnea
- SpO2:
-
Saturation of peripheral oxygen
- SDNN:
-
Standard deviation of all NN intervals
- RMSSD:
-
The square root of the mean of the sum of the squares of differences between adjacent NN intervals
- pNN50:
-
Percentage of successive RR intervals that differ by more than 50 ms
- VLF:
-
Power in very low-frequency range
- LF:
-
Power in low frequency range
- HF:
-
Power in high frequency range
- LF/HF:
-
Ratio LF/HF
References
Barker, A. Medical progress: Bronchiectasis. N. Engl. J. Med. 346, 1383–1393 (2002).
Chang, A. & Bilton, D. Exacerbations of cystic fibrosis: Non-cystic fibrosis bronchiectasis. Thorax 63, 269–276 (2008).
Khoo, J. K. et al. Bronchiectasis in the last five years: New developments. J. Clin. Med. 5, 115 (2016).
Polverino, E. et.al. Global burden of non-cystic fibrosis bronchiectasis: A simple epidemiological analysis. ERS 1–2 (2012).
EMBARC- The European Bronchiectasis Registry. What is Bronchiectasis? [Internet] [cited June 26, 2014] Available from: https://www.bronchiectasis.eu/what-is-bronchiectasis.
McDonnell, M. J., Ward, C., Lordan, J. L. & Rutherford, R. M. Non cystic fibrosis bronchiectasis. Q. J. Med. 106, 709–715 (2013).
Cantin, A. M. Bronchiectasis: From targets to therapies. Can. J. Respir., Critical Care, Sleep Med. 7(4), 206–212 (2023).
King, P. T. The role of the immune response in the pathogenesis of bronchiectasis. Biomed. Res. Int. 2018(1), 6802637 (2018).
Johnson, E., Long, M. B. & Chalmers, J. D. Biomarkers in bronchiectasis. Eur. Respir. Rev. 33(173), 230234 (2024).
Doumat, G., Aksamit, T. R. & Kanj, A. N. Bronchiectasis: A clinical review of inflammation. Respir. Med. 25, 108179 (2025).
Giannoni, A. et al. Autonomic and respiratory consequences of altered chemoreflex function: clinical and therapeutic implications in cardiovascular diseases. Eur. J. Heart Fail. 25(5), 642–656 (2023).
Rached, S., Amaral, T. S., Angelis, K. D., Sartori, M. Abnormal heart rate variability in patients with bronchiectasis. ERS (2015).
Sáez-Pérez, J. A. et al. Heart rate recovery after the 6-min walk test in people with bronchiectasis. ERJ Open Res. 11(2), 00694 (2025).
Alam, M. A. et al. Bronchiectasis-COPD overlap syndrome: A comprehensive review of its pathophysiology and potential cardiovascular implications. Ther. Adv. Pulmon. Crit. Care Med. 19, 29768675241300810 (2024).
Achten, J. & Jeukendrup, A. E. Heart rate monitoring: Applications and limitations. Sports Med. 33, 517–538 (2003).
Acharya, U. R. et al. Heart rate variability: a review: Med Biol Eng Comput. 44, 1031–1051 (2006).
Vanderlei, L. C. et al. Basic notions of heart rate variability and its clinical applicability. Rev. Bras. Cir. Cardiovasc. 24, 205–217 (2009).
Camillo, C. A. et al. Heart rate variability and disease characteristics in patients with COPD. Lung 186, 393–401 (2008).
Von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guIdelines for reporting observational studies. The Lancet. 370(9596), 1453–1457 (2007).
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93,1043–1065 (1996).
Porto, L. G. G. & Junqueira Júnior, L. F. Comparison of time-domain short-term heart interval variability analysis using a wrist-worn heart rate monitor and the conventional electrocardiogram. PACE 32, 43–51 (2008).
Vanderlei, L. C., Silva, R. A., Pastre, C. M., Azevedo, F. M. & Godoy, M. F. Comparison of the Polar S810i monitor and the ECG for the analysis of heart rate variability in the time and frequency domains. Braz. J. Med. Biol. Res. 41, 854–859 (2008).
Montemurro, L. T. et al. Cardiac sympathetic hyperactivity in patients with chronic obstructive pulmonary disease and obstructive sleep apnea. COPD 13, 706–711 (2016).
Marcu, D. T. et al. Cardiovascular involvement in tuberculosis: From pathophysiology to diagnosis and complications—a narrative review. Diagnostics. 13(3), 432 (2023).
Katicheva, A. V. et al. Assesment of premarure death in patients with pulmonary tuberculosis and chronic obstructive pulmonary disease. Bull. Russ. Military Med. Acad. 22(2), 19–22 (2020).
Mitroi, D. M. et al. Hypercoagulability in tuberculosis: Pathophysiological mechanisms, associated risks, and advances in management—a narrative review. J. Clin. Med. 14(3), 762 (2025).
George, P. J. et al. Coincident helminth infection modulates systemic inflammation and immune activation in active pulmonary tuberculosis. PLoS Negl. Trop. Dis. 8(11), e3289 (2014).
Van Gestel, A. J. & Steier, J. Autonomic dysfunction in patients with chronic obstructive pulmonary disease (COPD). J Thorac Dis. 2, 215–222 (2010).
Liu, Z., Wu, H. & Hu, M. Heart rate variability in patients with generalized anxiety disorder and depressive disorder. Chin. General Pract. 22(33), 4069–4072 (2019).
Chen, L. F. et al. Depression, anxiety, and heart rate variability: a case-control study in Taiwan. J. Med. Sci. 34(1), 9–18 (2014).
Liu, W., Wang, S., Gu, H. & Li, R. Heart rate variability, a potential assessment tool for identifying anxiety, depression, and sleep disorders in elderly individuals. Front. Psych. 23(16), 1485183 (2025).
Schiweck, C., Piette, D., Berckmans, D., Claes, S. & Vrieze, E. Heart rate and high frequency heart rate variability during stress as biomarker for clinical depression. A systematic review. Psychol. Med. 49(2), 200–211 (2019).
Chen, W. L., Chen, G. Y. & Kuo, C. D. Hypoxemia and autonomic nervous dysfunction in patients with chronic obstructive pulmonary disease. Respir. Med. 100(9), 1547–1553 (2006).
Corbo, G. M. et al. C-reactive protein, lung hyperinflation and heart rate variability in chronic obstructive pulmonary disease–a pilot study. COPD J. Chronic Obstr. Pulmon. Dis. 10(2), 200–207 (2013).
Leigh, R. et al. Human rhinovirus infection enhances airway epithelial cell production of growth factors involved in airway remodeling. J. Allergy Clin. Immunol. 121(5), 1238–1245 (2008).
Bernardi, L., Porta, C., Gabutti, A., Spicuzza, L. & Sleight, P. Modulatory effects of respiration. Auton. Neurosci. 90(1–2), 47–56 (2001).
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal
Author information
Authors and Affiliations
Contributions
D.D., M.K.S., A.B., A.M.P., and V.K. were involved in conceptualizing the study, developing methodologies, acquiring data, and writing the manuscript. D.D., M.K.S., A.B., and V.K. contributed significantly to the design, data acquisition, analysis, and writing of the results. All authors reviewed the final draft of the manuscript. D.D., A.B., and M.K.S. wrote the preliminary draft, and A.M.P. and V.K. reviewed it. The final version was prepared with the consensus of all the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved by Kasturba Medical College and Kasturba Hospital Institutional Ethics Committee (IEC: 72/2018) and was registered under the Clinical Trial Registry of India.(CTRI/2018/11/016355)(https://ctri.nic.in/Clinicaltrials/pmaindet2.php?EncHid=MjU2MzE=&Enc=&userName=CTRI/2018/11/016355 ). Before their participation, all participants provided informed consent by signing and returning the consent documents.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dinesh, D., Vaishali, K., Bhat, A. et al. Cardiac autonomic function in bronchiectasis and age and gender-matched healthy participants: case–control study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36722-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36722-9