Abstract
The angiotensin-converting enzyme (ACE) insertion/deletion (I/D) polymorphism influences renin-angiotensin-aldosterone system activity and may modulate cardiovascular adaptations to exercise. Yet, evidence regarding genotype-dependent responses to aquatic high-intensity interval training (HIIT) in postmenopausal women is limited. We aimed to compare the effects of 12-week aquatic HIIT on blood pressure, lipid profile, and arterial stiffness between postmenopausal women with the ACE II genotype and those carrying at least one D allele (ID/DD genotype). Sixty postmenopausal women aged 45–75 years were recruited, with ten participants voluntarily withdrawing from the study and three lost to follow-up. A total of 47 participants completed the intervention (21.7% attrition). Participants were stratified into ACE II (n = 25, 59.0 ± 5.52 years) and ID/DD (n = 22, 57.4 ± 7.52 years) genotype groups. Participants performed a 12-week aquatic HIIT program, with three 40-minute sessions per week. Each session consisted of a 6-minute warm-up, 30 min of main training (involving strength and jumping exercises), and a 4-minute cool-down. key cardiovascular outcomes were measured at pre- and post-intervention. Following a 12-week aquatic HIIT program, no significant differences were observed in post-intervention systolic blood pressure (SBP), diastolic blood pressure (DBP), or mean arterial pressure (MAP) between the II and ID/DD groups (all p > 0.05). While no significant between-group differences were found in brachial-ankle pulse wave velocity (baPWV) on either side (p = 0.058, 0.086), a greater magnitude of change in baPWV values was observed in the ID/DD group. Within-group analyses revealed that the II group exhibited significant reductions in SBP, DBP, MAP, and baPWV(right) (p = 0.023, 0.041, 0.020, 0.019), whereas the ID/DD group showed significant increases in baPWV (right/left, p = 0.013, 0.002). Post-intervention TG levels were significantly lower in the ID/DD group compared to the II group (p = 0.000), with a non-significant trend toward higher HDL-C levels (p = 0.053). Both groups demonstrated significant improvements in lipid profiles, characterized by increased HDL-C and decreased LDL-C (p < 0.05). The aquatic HIIT program significantly improved blood lipids in postmenopausal women, yet no significant ACE genotype-specific effects were observed on blood pressure or arterial stiffness. While the II group exhibited favorable reductions in blood pressure, the ID/DD group showed increased arterial stiffness, suggesting potential vascular risks and underscoring the need for monitoring during exercise.
Trial registration: ChiCTR2400087544 (July 30, 2024).
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Abbreviations
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MAP:
-
Mean arterial pressure
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- baPWV:
-
Brachial-ankle pulse wave velocity
- HIIT:
-
High-intensity interval training
- HRR:
-
Heart rate reserve
- RPE:
-
Rating of perceived exertion
- PAR-Q:
-
Physical activity readiness questionnaire
- Mean ± SD:
-
Mean ± standard deviation
- ACE:
-
Angiotensin-converting enzyme
- II:
-
Insertion/insertion genotype
- ID/DD:
-
Insertion/deletion and deletion/deletion genotypes
- RAAS:
-
Renin-angiotensin-aldosterone system
- Ang II:
-
Angiotensin II
- NO:
-
Nitric oxide
- Ct:
-
Cycle threshold
Refferences
Lu, Y., Tian, J., Wu, L., Xia, Q. & Zhu, Q. Low appendicular skeletal muscle index increases the risk of carotid artery plaque in postmenopausal women with and without hypertension/hyperglycemia: a retrospective study. BMC Geriatr. 23, 379 (2023).
van Roeters, J. E. et al. Women, lipids, and atherosclerotic cardiovascular disease: a call to action from the European atherosclerosis society. Eur. Heart J. 44, 4157–4173 (2023).
Lu, Y. et al. Trajectories of Age-Related arterial stiffness in Chinese men and women. J. Am. Coll. Cardiol. 75, 870–880 (2020).
Cignarella, A., Kratz, M. & Bolego, C. Emerging role of Estrogen in the control of cardiometabolic disease. Trends Pharmacol. Sci. 31, 183–189 (2010).
Lisabeth, L. & Bushnell, C. Stroke risk in women: the role of menopause and hormone therapy. Lancet Neurol. 11, 82–91 (2012).
de Faria, M. H. S. et al. Lower limb strength training (LLST) modulates serum and urinary levels of renin angiotensin system molecules in healthy young males. Sport Sci Health 18, 55–66 (2022).
Shin, J. et al. Age at menopause and risk of heart failure and atrial fibrillation: a nationwide cohort study. Eur. Heart J. 43, 4148–4157 (2022).
Manson, J. E. et al. The women’s health initiative randomized trials and clinical practice: A review. JAMA 331, 1748–1760 (2024).
Chlebowski, R. T. et al. Influence of Estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the women’s health initiative randomized trial. JAMA 289, 3243–3253 (2003).
Rossouw, J. E. et al. Risks and benefits of Estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA 288, 321–333 (2002).
Langrish, J. P. et al. Cardiovascular effects of physiological and standard sex steroid replacement regimens in premature ovarian failure. Hypertension 53, 805–811 (2009).
Canoy, D. et al. Antihypertensive drug effects on long-term blood pressure: an individual-level data meta-analysis of randomised clinical trials. Heart 108, 1281–1289 (2022).
Chalmers, J. et al. 1999 world health Organization-International society of hypertension guidelines for the management of hypertension. Clin. Exp. Hypertens. 21, 1009–1060 (1999).
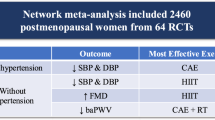
Yang, D. et al. Effectiveness of exercise training on arterial stiffness and blood pressure among postmenopausal women: a systematic review and meta-analysis. Syst. Rev. 13, 169 (2024).
Unger, T. et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension 75, 1334–1357 (2020).
China Lipid Management Guideline Revision Joint Expert Committee. China lipid management guidelines (Community health version 2024). Chin. J. Cardiol. 52, 330–337 (2024).
Phillips, S. A., Mahmoud, A. M., Brown, M. D. & Haus, J. M. Exercise interventions and peripheral arterial function: implications for cardio-metabolic disease. Prog Cardiovasc. Dis. 57, 521–534 (2015).
Fukuie, M. et al. The effect of head-out aquatic exercise on arterial stiffness in middle-aged and elderly people. Pulse (Basel). 7, 51–59 (2019).
Hagberg, J. M., Park, J. J. & Brown, M. D. The role of exercise training in the treatment of hypertension: an update. Sports Med. 30, 193–206 (2000).
Roltsch, M. H., Mendez, T., Wilund, K. R. & Hagberg, J. M. Acute resistive exercise does not affect ambulatory blood pressure in young men and women. Med. Sci. Sports Exerc. 33, 881–886 (2001).
Focht, B. C. & Koltyn, K. F. Influence of resistance exercise of different intensities on state anxiety and blood pressure. Med. Sci. Sports Exerc. 31, 456–463 (1999).
Gao, B., Chen, P. & Yang, Z. Research progress on the relationship between angiotensin-converting enzyme gene polymorphism and exercise capacity. J. Shanghai Univ. Sport. 30, 75–81 (2006).
Montgomery, H. et al. Angiotensin-converting-enzyme gene insertion/deletion polymorphism and response to physical training. Lancet 353, 541–545 (1999).
Mota, M. R. et al. Acute and chronic effects of resistance exercise on blood pressure in elderly women and the possible influence of ACE I/D polymorphism. Int. J. Gen. Med. 6, 581–587 (2013).
Montrezol, F. T. et al. ACE gene plays a key role in reducing blood pressure in the hyperintensive elderly after resistance training. J. Strength. Cond Res. 33, 1119–1129 (2019).
Sayed-Tabatabaei, F. A., Oostra, B. A., Isaacs, A., van Duijn, C. M. & Witteman, J. C. ACE polymorphisms. Circ. Res. 98, 1123–1133 (2006).
Rigat, B. et al. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J. Clin. Invest. 86, 1343–1346 (1990).
Zhang, B. et al. Association of angiotensin-converting-enzyme gene polymorphism with the depressor response to mild exercise therapy in patients with mild to moderate essential hypertension. Clin. Genet. 62, 328–333 (2002).
Jones, J. M. et al. Renin-angiotensin system genes and exercise training-induced changes in sodium excretion in African American hypertensives. Ethn. Dis. 16, 666–674 (2006).
Warburton, D. E. R., Jamnik, V. K., Bredin, S. S. D. & Gledhill, N. The physical activity readiness questionnaire for everyone (PAR-Q+) and electronic physical activity readiness medical examination (ePARmed-X+). Health Fit. J. Can. 4, 3–17 (2011).
Grummt, M., Hafermann, L., Claussen, L., Herrmann, C. & Wolfarth, B. Rating of perceived exertion: a large cross-sectional study defining intensity levels for individual physical activity recommendations. Sports Med. Open. 10, 71 (2024).
Kundu, R., Biswas, S. & Das, M. Mean arterial pressure classification: a better tool for statistical interpretation of blood pressure related risk covariates. Cardiol. Angiol. 6, 1–7 (2017).
Kaess, B. M. et al. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 308, 875–881 (2012).
Luo, Y. et al. Epidemiological status and trends of hypertension among adults in China. Chin. J. Thorac. Cardiovasc. Surg. Clin. Med. 31, 922–928 (2024).
Fornage, M. et al. Variation in the region of the angiotensin-converting enzyme gene influences interindividual differences in blood pressure levels in young white males. Circulation 97, 1773–1779 (1998).
Santana, H. A. et al. The higher exercise intensity and the presence of allele I of ACE gene elicit a higher post-exercise blood pressure reduction and nitric oxide release in elderly women: an experimental study. BMC Cardiovasc. Disord. 11, 71 (2011).
Azadpour, N., Tartibian, B. & Koşar, Ş. N. Effects of aerobic exercise training on ACE and ADRB2 gene expression, plasma angiotensin II level, and flow-mediated dilation: a study on obese postmenopausal women with prehypertension. Menopause 24, 269–277 (2017).
Bo, W., Cai, M. & Tian, Z. Aerobic exercise improves cardiac function in mice after myocardial infarction by inhibiting sympathetic overactivation via the brain-heart axis. Chin. J. Sport Sci. 44, 30–40 (2024).
Evans, L. C., Dayton, A. & Osborn, J. W. Renal nerves in physiology, pathophysiology and interoception. Nat. Rev. Nephrol. 21 (1), 57–69 (2025).
Hall, J. E., do Carmo, J. M., da Silva, A. A., Wang, Z. & Hall, M. E. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat. Rev. Nephrol. 15, 367–385 (2019).
Kaufmann, H., Norcliffe-Kaufmann, L. & Palma, J. A. Baroreflex dysfunction. N Engl. J. Med. 382, 163–178 (2020).
Yamashina, A. et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens. Res. 25, 359–364 (2002).
Fujie, S. et al. Impact of resistance training and chicken intake on vascular and muscle health in elderly women. J. Cachexia Sarcopenia Muscle. 16, e100–e112 (2025).
Toussaint, O., Medrano, E. E. & von Zglinicki, T. Cellular and molecular mechanisms of stress-induced premature senescence (SIPS) of human diploid fibroblasts and melanocytes. Exp. Gerontol. 35, 927–945 (2000).
Touyz, R. M. & Schiffrin, E. L. Signal transduction mechanisms mediating the physiological and pathophysiological actions of angiotensin II in vascular smooth muscle cells. Pharmacol. Rev. 52, 639–672 (2000).
Tang, D. H. et al. Exercise combined with dietary control improves endothelial function in male obese adolescents by reducing renin-angiotensin-aldosterone system activity. Chin. J. Sport Sci. 37, 48–54 (2017).
Miyachi, M. Effects of resistance training on arterial stiffness: a meta-analysis. Br. J. Sports Med. 47, 393–396 (2013).
Mahmood, S. S., Levy, D., Vasan, R. S. & Wang, T. J. The Framingham heart study and the epidemiology of cardiovascular disease: a historical perspective. Lancet 383, 999–1008 (2014).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Circulation 140, e596–e646 (2019).
Kim, J. H., Ha, M. S., Ha, S. M. & Kim, D. Y. Aquatic exercise positively affects physiological frailty among postmenopausal women: a randomized controlled clinical trial. Healthc. (Basel). 9, 409 (2021).
Woo-Cheol, K., Suk-Lip, C., Sung-Woon, K. & Hae-Ryoung, P. The effects of aquarobics on blood pressure, heart rate, and lipid profile in older women with hypertension. Indian J. Sci. Technol. 9, 1–7 (2016).
Huynh, E. et al. The effects of aerobic exercise on cardiometabolic health in postmenopausal females: a systematic review and meta-analysis of randomized controlled trials. Womens Health (Lond). 20, 17455057241290889 (2024).
Igarashi, Y. & Nogami, Y. Response of lipids and lipoproteins to regular aquatic endurance exercise: a meta-analysis of randomized controlled trials. J. Atheroscler Thromb. 26, 14–30 (2019).
Wei, C. et al. Exercise might favor reverse cholesterol transport and lipoprotein clearance: potential mechanism for its anti-atherosclerotic effects. Biochim. Biophys. Acta. 1723, 124–127 (2005).
Zhou, W. S. & Yang, Y. Meta-analysis of the effects of aquatic exercise on cardiovascular health in postmenopausal women. Chin. J. Sport Sci. 55, 27–38 (2019).
Stein, R. A. et al. Effects of different exercise training intensities on lipoprotein cholesterol fractions in healthy middle-aged men. Am. Heart J. 119, 277–283 (1990).
Vaughan, D., Huber-Abel, F. A., Graber, F., Hoppeler, H. & Flück, M. The angiotensin converting enzyme insertion/deletion polymorphism alters the response of muscle energy supply lines to exercise. Eur. J. Appl. Physiol. 113, 1719–1729 (2013).
Miyoshi, H. et al. Perilipin promotes hormone-sensitive lipase-mediated adipocyte lipolysis via phosphorylation-dependent and -independent mechanisms. J. Biol. Chem. 281, 15837–15844 (2006).
Acknowledgements
We gratefully acknowledge all authors for their contributions to this study.
Funding
This study was supported by the Project Funding of Humanities and Social Sciences Research in China, Ministry of Education (Grant Number: 21YJC890051 to W-SZ).
Author information
Authors and Affiliations
Contributions
LT and W-SZ: Conceptualization, methodology, supervision, writing the original draft. Y-HL and NX: Data curation, formal analysis, and review. B-FL, Z-HL, S-JG, R-YZ, XX, CY, Q-YW, and LS: Investigation, data acquisition, project administration. MG and T-QZ: Data curation. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Review Committee for Biomedical Studies at Nanjing Normal University (Approval No. NNU202407009). All procedures were conducted in accordance with the Declaration of Helsinki and relevant ethical guidelines. Written informed consent was obtained from all participants prior to their inclusion in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, Ws., Li, Yh., Xu, N. et al. Effects of 12-week aquatic HIIT on blood pressure lipid profile and BaPWV in postmenopausal women with different ACE genotypes. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36835-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36835-1