Abstract
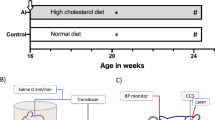
Bladder rupture repair surgery is limited by its long duration, significant blood loss, and complex procedures. Biological welding technology, which integrates multiple functions such as cutting, hemostasis, and tissue fusion, has shown potential in the field of soft tissue repair surgery but has not yet been widely explored in clinical applications for bladder rupture repair. This study used 32 adult male Beagle dogs to establish a bladder rupture model, randomly assigned to the biological welding group or the traditional suturing group. Outcomes assessed included surgical time, blood loss, postoperative inflammation, and hematuria. Histopathological analysis and RNA sequencing analysis were performed at multiple postoperative time points to evaluate the tissue recovery process and repair mechanisms. The results demonstrated that biological welding significantly reduced surgical time (21.80 ± 4.79 min vs. 75.15 ± 13.26 min, p < 0.001) and intraoperative blood loss (6.37 ± 0.89 g vs. 30.36 ± 6.59 g, p < 0.001) compared to traditional suturing. Postoperative complications, such as hematuria and inflammatory response, were notably lower in the biological welding group. Histopathological analysis revealed enhanced cell migration and tissue fusion in the biological welding group, leading to accelerated bladder healing and reduced adhesions. Transcriptomic sequencing indicated that biological welding activated a limited number of immune-related genes and signaling pathways in the early postoperative period, facilitating rapid repair and a shorter duration of abnormal gene expression. Our research indicates that biological welding technology demonstrates significant advantages in bladder rupture repair surgery, including enhanced surgical efficiency, reduced incidence of postoperative complications, and accelerated tissue healing process, with broad prospects for clinical application.
Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available in the Zenodo repository, https://doi.org/10.5281/zenodo.18255296.
References
Morey, A. F., Broghammer, J. A., Hollowell, C. M. P., McKibben, M. J. & Souter, L. Urotrauma guideline 2020: AUA guideline. J. Urol. 205, 30–35. https://doi.org/10.1097/ju.0000000000001408 (2021).
Reddy, D., Laher, A. E., Lawrentschuk, N. & Adam, A. Spontaneous (idiopathic) rupture of the urinary bladder: a systematic review of case series and reports. BJU Int. 131, 660–674. https://doi.org/10.1111/bju.15974 (2023).
Stabile, G. et al. Spontaneous Bladder Rupture after Normal Vaginal Delivery: Description of a Rare Complication and Systematic Review of the Literature. Diagnostics https://doi.org/10.3390/diagnostics11101885 (2021).
Da Huang, J., Shao, E. X., Tham, C. M., Chung, E. & Rhee, H. Bladder malignancy as a cause of spontaneous bladder rupture: A systematic review. BJUI Compass. 5, 12–16. https://doi.org/10.1002/bco2.281 (2024).
Piramide, F. et al. Atlas of intracorporeal orthotopic neobladder techniques after Robot-assisted radical cystectomy and systematic review of clinical outcomes. Eur. Urol. 85, 348–360. https://doi.org/10.1016/j.eururo.2023.11.017 (2024).
Masone, M. C. HRQOL after radical cystectomy. Nat. Rev. Urol. 18, 706. https://doi.org/10.1038/s41585-021-00540-7 (2021).
Fu, S. et al. Robot-assisted radical cystectomy with intracorporeal urinary diversion: an updated systematic review and meta-analysis of its differential effect on effectiveness and safety. Int. J. Surg. (London England). 110, 2366–2380. https://doi.org/10.1097/js9.0000000000001065 (2024).
Li, H. P., Luo, N. Q., Zhang, M. & Liu, Y. Laparoscopic repair of extraperitoneal bladder rupture via the extraperitoneal approach: A case report. Asian J. Surg. 47, 4855–4856. https://doi.org/10.1016/j.asjsur.2024.05.162 (2024).
Catto, J. W. F. et al. Effect of Robot-Assisted radical cystectomy with intracorporeal urinary diversion vs open radical cystectomy on 90-Day morbidity and mortality among patients with bladder cancer: A randomized clinical trial. Jama 327, 2092–2103. https://doi.org/10.1001/jama.2022.7393 (2022).
Katsimperis, S. et al. Complications after radical cystectomy: A systematic review and Meta-analysis of randomized controlled trials with a Meta-regression analysis. Eur. Urol. Focus. 9, 920–929. https://doi.org/10.1016/j.euf.2023.05.002 (2023).
Martini, A. et al. Robot-assisted radical cystectomy with orthotopic neobladder reconstruction: techniques and functional outcomes in males. Eur. Urol. 84, 484–490. https://doi.org/10.1016/j.eururo.2023.04.009 (2023).
Tuderti, G. et al. Impact of diabetes mellitus on oncologic outcomes in patients receiving robot-assisted radical cystectomy for bladder cancer. World J. Urol. 42, 479. https://doi.org/10.1007/s00345-024-05178-9 (2024).
Ahmadi, H. et al. Long-term renal function in patients with chronic kidney disease following radical cystectomy and orthotopic neobladder. BJU Int. 130, 200–207. https://doi.org/10.1111/bju.15685 (2022).
Umanets, N., Pasyechnikova, N. V., Naumenko, V. A. & Henrich, P. B. High-frequency electric welding: a novel method for improved immediate chorioretinal adhesion in vitreoretinal surgery.. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 252, 1697–1703. https://doi.org/10.1007/s00417-014-2709-0 (2014).
Wang, H. et al. Temperature Distribution of Vessel Tissue by High Frequency Electric Welding with Combination Optical Measure and Simulation. Biosensors https://doi.org/10.3390/bios12040209 (2022).
Yin, L. et al. Dynamic Impedance Analysis of Intestinal Anastomosis during High-Frequency Electric Field Welding Process. Sensors https://doi.org/10.3390/s22114101 (2022).
Zabolotnyi, D. & Kvasha, O. Bipolar high-frequency electric welding in radical resection of frontal sinus tumors. Carcinogenesis 44, 175–181. https://doi.org/10.1093/carcin/bgad018 (2023).
Tryliskyy, Y. et al. Safety analysis of endoscopic haemostasis using a high-frequency live tissue electric welding device - EKVZ300 PATONMED. Przeglad Gastroenterologiczny. 13, 234–237. https://doi.org/10.5114/pg.2018.78289 (2018).
Tyselskyi, V., Poylin, V. & Kebkalo, A. Biological welding - novel technique in the treatment of esophageal metaplasia. Polski Przeglad Chirurgiczny. 92, 1–5. https://doi.org/10.5604/01.3001.0014.1176 (2020).
Zeng, F., Cao, Q., Fu, F., Wang, B. & Sun, Z. Biological welding: a rapid and bloodless approach to circumcision. World J. Urol. 43, 25. https://doi.org/10.1007/s00345-024-05355-w (2024).
Zhu, C. et al. Characteristics of Collagen Changes in Small Intestine Anastomoses Induced by High-Frequency Electric Field Welding. Biomolecules https://doi.org/10.3390/biom12111683 (2022).
Becker, L. et al. Raman microspectroscopy identifies fibrotic tissues in collagen-related disorders via deconvoluted collagen type I spectra. Acta Biomater. 162, 278–291. https://doi.org/10.1016/j.actbio.2023.03.016 (2023).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–d592. https://doi.org/10.1093/nar/gkac963 (2023).
Zhu, C. et al. Assessing the influence of parameters on tissue welding in small bowel end-to-end anastomosis in vitro and in vivo. Surg. Endosc. 38, 3126–3137. https://doi.org/10.1007/s00464-024-10795-x (2024).
Davis, L. et al. Female sexual function following radical cystectomy in bladder cancer. Sex. Med. Reviews. 10, 231–239. https://doi.org/10.1016/j.sxmr.2021.10.005 (2022).
Yang, Z., Dou, X., Zhou, W. & Liu, Q. Robot-assisted, laparoscopic and open radical cystectomy for bladder cancer: A systematic review and network meta-analysis. Int. Braz. J. Urol. 50, 683–702. https://doi.org/10.1590/s1677-5538.Ibju.2024.0191 (2024).
Saiz, A. M. Jr. et al. Bladder repair with irrigation and debridement and open reduction internal fixation of the anterior pelvic ring is safe and decreases risk of infection in pelvic ring injuries with extraperitoneal bladder ruptures. J. Orthop. Trauma. 38, 72–77. https://doi.org/10.1097/bot.0000000000002720 (2024).
Xiong, X. et al. Effect of neurovascular bundle sparing radical cystectomy on post-operative continence and sexual function: A systematic review and meta-analysis. Andrology 9, 221–232. https://doi.org/10.1111/andr.12898 (2021).
Zhu, C. et al. Vivo tissue healing mechanism at the intestinal anastomosis site following high-frequency electric welding. Int. J. Surg. (London England). 111, 1614–1618. https://doi.org/10.1097/js9.0000000000002093 (2024).
Feleshtynskyi, Y. P., Oparin, S. O., Sorokin, B. V., Boiarskaia, M. G. & Lutsenko, D. V. Endoscopic hemostasis in ulcerative gastroduodenal bleeding using high-frequency biological welding electroligation. Wiadomosci lekarskie (Warsaw, Poland: 1960) 74, 2159–2162. (2021).
Savolyuk, S. I., Khodos, V. A., Herashchenko, R. A. & Horbovets, V. S. Comparative evaluation of the results of surgical treatment of acute ascending thrombophlebitis of the great saphenous vein using the endovascular high-frequency welding technique and traditional technique. Wiadomosci lekarskie (Warsaw, Poland: 1960) 73, 638–641. (2020).
Funding
This research was supported by the International Cooperation in Science and Technology of The Science and Technology Ministry (2014DFR30860), Shenzhen Science and Technology Program (JCYJ20220531103004008), International Cooperative Research Program of Shenzhen (GJHZ20220913143006011) and Medicine-Engineering Interdisciplinary Research Foundation of Shenzhen University (2023YG018).
This manuscript utilized AI tools (Grammarly and ChatGPT)for language polishing.
Author information
Authors and Affiliations
Contributions
Conception and design: Zhongyi Sun, Fanchun Zeng. Collection data: Fanchun Zeng, Fengwen Fu, Quanfu Cao,Minggan Guo,Yuan Chen. Data analysis and interpretation: Zhongyi Sun and Fanchun Zeng. Manuscript preparation: Fanchun Zeng, Revision of the manuscript: Zhongyi Sun. Manuscript: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The experiments adhered to the guidelines for the care and use of laboratory animals and were approved by the Animal Ethics Committee of the Third Military Medical University Daping Hospital (Animal Ethics Approval :Medical Research and Review (2015) No. 53).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zeng, F., Chen, Y., Guo, M. et al. Biological welding enables rapid and efficient bladder cystotomy closure and reveals the underlying repair mechanism. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36959-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36959-4