Abstract
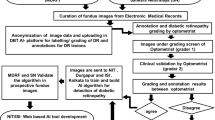
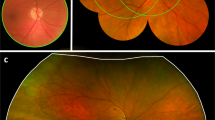
The escalating prevalence of diabetes mellitus (DM) emphasizes the critical need for early detection of diabetic retinopathy (DR). This study assesses the performance of the autonomous AI-based diagnostic system IDx-DR in detecting DR and its associated confounders in a real-world clinical setting. This prospective cross-sectional study involved 875 diabetic patients with a mean age of 52 years (range: 8–92). Retinal images were captured by trained assistants. IDx-DR results were compared with mydriatic fundus examination (gold standard) and Ophthalmologists’ image analysis. Factors impacting image acquisition or analyzability were examined. Among all patients, 10.5% yielded no image in miosis, and 26.1% were unanalyzable by IDx-DR. Confounders affecting image acquisition were examiner, pupil size, patient age and patients’ visual acuity. When good quality images were achieved, IDx-DR performed well, particularly in detection of severe DR (sensitivity 94.4%; specificity 90.5%). IDx-DR results exactly matched Ophthalmologists’ mydriatic fundoscopy gradings in 54.2% if images of sufficient quality were obtainable. Undergrading of DR severity by IDx-DR was rare (4.8%). IDx-DR shows promise in detecting DR, especially in resource-limited settings and in detecting severe DR. One remaining challenge is good image acquisition in miotic patients.
Similar content being viewed by others
Data availability
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy of the patients.
References
Tönnies, T. et al. Projected number of people with diagnosed Type 2 diabetes in Germany in 2040. Diabet. Med. 36, 1217–1225 (2019).
Williams, L. B., Prakalapakorn, S. G., Ansari, Z. & Goldhardt, R. Impact and Trends in Global Ophthalmology. Curr Ophthalmol Rep 8, 136–143 (2020).
Rohan, T. E., Frost, C. D. & Wald, N. J. Prevention of blindness by screening for diabetic retinopathy: A quantitative assessment. BMJ 299, 1198–1201 (1989).
Aderneuer, H. Telemedizin und künstliche Intelligenz im Zusammenhang mit Augenscreening. 11.
Lei, C. et al. Facial expression of patients with Graves’ orbitopathy. J Endocrinol Invest 46, 2055–2066 (2023).
Grzybowski, A. & Brona, P. Analysis and Comparison of Two Artificial Intelligence Diabetic Retinopathy Screening Algorithms in a Pilot Study: IDx-DR and Retinalyze. JCM 10, 2352 (2021).
Abràmoff, M. D., Lavin, P. T., Birch, M., Shah, N. & Folk, J. C. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. npj Digital Med 1, 39 (2018).
Paul, S. et al. Einsatz von künstlicher Intelligenz im Screening auf diabetische Retinopathie an einer diabetologischen Schwerpunktklinik. Ophthalmologe https://doi.org/10.1007/s00347-021-01556-5 (2022).
Ziemssen, F., Lemmen, K., Bertram, B., Hammes, H. P. & Agostini, H. Nationale Versorgungsleitlinie (NVL) Diabetische Retinopathie: 2. Auflage der NVL zur Therapie der diabetischen Retinopathie. Ophthalmologe 113, 623–638 (2016).
Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 98, 823–833 (1991).
The ACCORD Study Group and ACCORD Eye Study Group. Effects of Medical Therapies on Retinopathy Progression in Type 2 Diabetes. N Engl J Med 363, 233–244 (2010).
Landis, J. R. & Koch, G. G. The Measurement of Observer Agreement for Categorical Data. Biometrics 33, 159 (1977).
Motulsky, H. J. & Brown, R. E. Detecting outliers when fitting data with nonlinear regression – a new method based on robust nonlinear regression and the false discovery rate. BMC Bioinformatics 7, 123 (2006).
Bellemo, V. et al. Artificial intelligence using deep learning to screen for referable and vision-threatening diabetic retinopathy in Africa: A clinical validation study. The Lancet Digital Health 1, e35–e44 (2019).
Krause, J. et al. Grader Variability and the Importance of Reference Standards for Evaluating Machine Learning Models for Diabetic Retinopathy. Ophthalmology 125, 1264–1272 (2018).
Grzybowski, A. et al. Variability of Grading DR Screening Images among Non-Trained Retina Specialists. JCM 11, 3125 (2022).
Srinivasan, S. et al. Inter-observer agreement in grading severity of diabetic retinopathy in wide-field fundus photographs. Eye 37, 1231–1235 (2023).
Verbraak, F. D. et al. Diagnostic Accuracy of a Device for the Automated Detection of Diabetic Retinopathy in a Primary Care Setting. Dia Care 42, 651–656 (2019).
Treder, M., Diener, R. & Eter, N. Künstliche Intelligenz zum Management von Makulaödemen: Chancen und Herausforderungen. Ophthalmologe 117, 989–992 (2020).
Zhang, W. et al. The Validation of Deep Learning-Based Grading Model for Diabetic Retinopathy. Front. Med. 9, 839088 (2022).
Sedova, A. et al. Comparison of early diabetic retinopathy staging in asymptomatic patients between autonomous AI-based screening and human-graded ultra-widefield colour fundus images. Eye 36, 510–516 (2022).
Roser, P., Grohmann, C., Aberle, J., Spitzer, M. S. & Kromer, R. Evaluation der Implementierung eines zugelassenen Künstliche-Intelligenz-Systems zur Erkennung der diabetischen Retinopathie. Diabetologie und Stoffwechsel 16, 402–408 (2021).
Mehra, A. A., Softing, A., Guner, M. K., Hodge, D. O. & Barkmeier, A. J. Diabetic Retinopathy Telemedicine Outcomes with Artificial Intelligence-Based Image Analysis, Reflex Dilation, and Image Overread. American Journal of Ophthalmology S0002939422003105 (2022) https://doi.org/10.1016/j.ajo.2022.08.008.
Liew, G., Mitchell, P., Wang, J. J. & Wong, T. Y. Fundoscopy: To dilate or not to dilate?. BMJ 332, 3 (2006).
Guillon, M. et al. The Effects of Age, Refractive Status, and Luminance on Pupil Size. Optom Vis Sci 93, 1093–1100 (2016).
Asbell, P. et al. Age-related cataract. The Lancet 365, 599–609 (2005).
Goldstein, J., Weitzman, D., Lemerond, M. & Jones, A. Determinants for scalable adoption of autonomous AI in the detection of diabetic eye disease in diverse practice types: Key best practices learned through collection of real-world data. Front. Digit. Health 5, 1004130 (2023).
Helmchen, L. A., Lehmann, H. P. & Abràmoff, M. D. Automated detection of retinal disease. Am J Manag Care 20, eSP48–52 (2014).
Oke, J. L., Stratton, I. M., Aldington, S. J., Stevens, R. J. & Scanlon, P. H. The use of statistical methodology to determine the accuracy of grading within a diabetic retinopathy screening programme. Diabet. Med. 33, 896–903 (2016).
Tufail, A. et al. An observational study to assess if automated diabetic retinopathy image assessment software can replace one or more steps of manual imaging grading and to determine their cost-effectiveness. Health Technol Assess 20, 1–72 (2016).
Sahoo, M., Ghorai, S., Pal, S. & Mitra, M. A Multi-Layer stacked ensemble classifier model for improved classification accuracy of Maculopathy gradation. Displays 73, 102213 (2022).
Zhang, X., Li, Y., Dong, S., Di, C. & Ding, M. The influence of user cognition on consumption decision-making from the perspective of bounded rationality. Displays 77, 102392 (2023).
Acknowledgements
Special thanks go to the non-medical functional team at the Karlsburg Clinic for Diabetes and Metabolic Diseases for their active support in this project.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University Medical Center Greifswald (BB 025/20).
Funding
Open Access funding enabled and organized by Projekt DEAL. This project was supported in part by funds from the EYEnovative grant from Novartis (to B.G.).
Author information
Authors and Affiliations
Contributions
Conceptualization, A. Stahl, A. Tayar, S. Paul, J. Kuhn, P. Augstein, W. Kerner; methodology, A. Stahl, A. Tayar, S. Paul, J. Kuhn, P. Augstein, W. Kerner; software, B. Poschkamp, R. Großjohann, J. Pfeil; validation E. Hunfeld, A. Tayar, S. Paul, B. Poschkamp, R. Großjohann, E. Morawiec-Kisiel, B. Bohl, J. Pfeil, M. Busch, M. Dähmcke, T. Brauckmann, S. Eilts, M-C. Bründer, M. Grundel, B. Grundel, F. Tost, J. Kuhn, J. Reindel, P. Augstein, W. Kerner, A. Stahl; formal analysis, E. Hunfeld, B. Poschkamp, A. Stahl; investigation, A. Tayar, S. Paul, B. Bohl, E. Morawiec-Kisiel, E. Hunfeld; resources, A. Stahl, B. Grundel, W. Kerner, J. Reindel, P. Augstein; data curation, E. Hunfeld, B. Poschkamp, R. Großjohann; writing—original draft preparation, E. Hunfeld; writing—review and editing, E. Hunfeld, A. Tayar, S. Paul, B. Poschkamp, R. Großjohann, E. Morawiec-Kisiel, B. Bohl, J. Pfeil, M. Busch, M. Dähmcke, T. Brauckmann, S. Eilts, M-C. Bründer, M. Grundel, B. Grundel, F. Tost, J. Kuhn, J. Reindel, P. Augstein, W. Kerner, A. Stahl; visualization, E. Hunfeld, J. Pfeil, B. Poschkamp, A. Stahl; supervision, A. Stahl, W. Kerner, J. Reindel, P. Augstein; project administration, E. Hunfeld, A. Stahl; funding acquisition, B. Grundel, J. Reindel, P. Augstein, W. Kerner, A. Stahl.
All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
B. Grundel points out the following relationships: Relationship: Novartis, Specifications: EYEnovative Förderpreis. E. Hunfeld, A. Tayar, S. Paul, B. Poschkamp, R. Großjohann, E. Morawiec-Kisiel, B. Bohl, J.M. Pfeil, M. Busch, M. Dähmcke, T. Brauckmann, S. Eilts, M.-C. Bründer, M. Grundel, B. Grundel, F. Tost, J. Kuhn, J. Reindel, P. Augstein, W. Kerner and A. Stahl declare that there is no conflict of interest.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hunfeld, E., Tayar, A., Paul, S. et al. Real-world performance of the AI diagnostic system IDx-DR in the diagnosis of diabetic retinopathy and its main confounders. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36970-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36970-9