Abstract
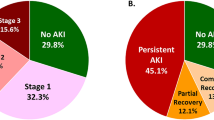
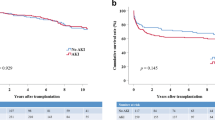
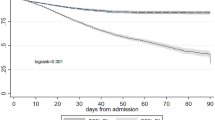
Deceased donor kidney transplantation (DDKT) has a serious problem of donor organ shortage, particularly in Asia. Consequently, donor kidneys with acute kidney injury (AKI) have been utilized for transplantation. This study aimed to evaluate the prognosis of DDKT using AKI kidneys. We analyzed the data of 8,523 adult patients who underwent DDKT between 2008 and 2022 using the Korean nationwide DDKT database. The association between donor AKI and death-censored graft failure was assessed using competing risk analysis, with adjustment through inverse probability of treatment weighting (IPTW). The AKI group included 3,453 patients (40.51%) and had a higher death-censored graft failure risk than the no-AKI group (hazard ratio: 1.27; 95% confidence interval: 1.05–1.53). Especially, AKI stage 3 subgroup had a higher death-censored graft failure risk than the no-AKI group. Furthermore, the AKI group had a higher death-censored graft failure risk than the no-AKI group in the subgroup with a Korean-kidney donor profile index (K-KDPI) ≥ 70 or the stable- or increasing trend of serum creatinine. In conclusion, using AKI kidneys with a K-KDPI < 70% or a decreasing creatinine trend, or at stage 1 and 2, could help in combating organ shortage, especially in areas with a long waiting time.
Similar content being viewed by others
Data availability
Data supporting the findings of this study are available from the corresponding author uponreasonable request.
References
Abecassis, M. et al. Kidney transplantation as primary therapy for end-stage renal disease: a National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQI™) conference. Clin. J. Am. Soc. Nephrol. 3, 471–480 (2008).
Azegami, T. et al. Efficacy of pre-emptive kidney transplantation for adults with end-stage kidney disease: a systematic review and meta-analysis. Ren. Fail. 45, 2169618 (2023).
Bastani, B. The present and future of transplant organ shortage: some potential remedies. J. Nephrol. 33, 277–288 (2020).
Transplantation IRiODa. Worldwide Actual Deceased Organ Donors Rate 2021. Web site. (accessed 21 April 2025). https://www.irodat.org/img/database/pdf/IRODaT_Newsletter_2021.pdf (2022).
USRDS. Annual Data Report, International Comparisons: Average yearly change in incidence of treated ESRD by country or region, 2010 versus 2020. Web site. (accessed 21 April 2022). https://usrds-adr.niddk.nih.gov/2022/end-stage-renal-disease/11-international-comparisons (2022).
Ng, Y-M. et al. Comparison of clinical outcomes among deceased donor kidney transplant recipients before and after utilizing estimated posttransplant survival score for kidneys allocation in Malaysia. Transpl. Proc. 54, 278–281 (2022).
Manla, Y. et al. Temporal trends in brain-death organ donation in asia: results from the global observatory on donation and transplantation. Transpl. Proc. 54, 233–236 (2022).
Wu, D. A. et al. Global trends and challenges in deceased donor kidney allocation. Kidney Int. 91, 1287–1299 (2017).
Glorioso, J. M. Kidney allocation policy: past, present, and future. Adv. Kidney Dis. Health. 28, 511–516 (2021).
Sethi, S. et al. Allocation of the highest quality kidneys and transplant outcomes under the new kidney allocation system. Am. J. Kidney Dis. 73, 605–614 (2019).
Rao, P. S. et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation 88, 231–236 (2009).
Kidney Donor Profile Index Calculator. Organ Procurement and Transplantation Network. Web site. https://optn.transplant.hrsa.gov/data/allocation-calculators/kdpi-calculator/
Merion, R. M. et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 294, 2726–2733 (2005).
Massie, A. B. et al. Survival benefit of primary deceased donor transplantation with high-KDPI kidneys. Am. J. Transpl. 14, 2310–2316 (2014).
Heilman, R. L. et al. Long-term outcomes following kidney transplantation from donors with acute kidney injury. Transplantation 103, e263–e272 (2019).
Hall, I. E. et al. Deceased-donor acute kidney injury is not associated with kidney allograft failure. Kidney Int. 95, 199–209 (2019).
Boffa, C. et al. Transplantation of kidneys from donors with acute kidney injury: friend or foe? Am. J. Transpl. 17, 411–419 (2017).
Lenain, R. et al. Association between deceased donor acute kidney injury assessed using baseline serum creatinine back-estimation and graft survival: results from the French National CRISTAL registry. Am. J. Kidney Dis. 79, 164–174 (2022).
International Summit on Transplant T, Organ T. The declaration of Istanbul on organ trafficking and transplant tourism. Kidney Int. 74, 854–859 (2008).
Mehta, R. L. et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit. Care. 11, R31 (2007).
Koo, T. Y. et al. A prognostic index for deceased donor kidneys and criteria for identifying suitable candidates for kidney transplantation from expanded criteria donors with prolonged waiting times. Kidney Dis. (Basel). 11, 143–153 (2025).
Liu, C. et al. Association of deceased donor acute kidney injury with recipient graft survival. JAMA Netw. Open. 3, e1918634–e1918634 (2020).
Lassnigg, A. et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J. Am. Soc. Nephrol. 15, 1597–1605 (2004).
Chertow, G. M., Burdick, E., Honour, M., Bonventre, J. V. & Bates, D. W. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 16, 3365–3370 (2005).
Meeusen, J. W., Kasozi, R. N., Larson, T. S. & Lieske, J. C. Clinical impact of the refit CKD-EPI 2021 creatinine-based eGFR equation. Clin. Chem. 68, 534–539 (2022).
Chan-On, C. & Sarwal, M. M. A comprehensive analysis of the current status and unmet needs in kidney transplantation in Southeast Asia. Front. Med. (Lausanne). 4, 84 (2017).
Hart, A. et al. OPTN/SRTR 2014 annual data report: kidney. Am. J. Transpl. 16 (Suppl 2), 11 (2016).
Kidney: donation, waiting list and transplants. Table 5.1 (ii) Deceased donors / kidneys in Eurotransplant in 2015. Eurotransplant Annual Report. (2015). https://www.eurotransplant.org/wp-content/uploads/2019/12/AR2015.pdf
Kim, K. H. et al. Current status of discarded grafts in Korean organ transplantation. Transpl. Proc. 51, 1478–1480 (2019).
Mohan, S. et al. Factors leading to the discard of deceased donor kidneys in the united States. Kidney Int. 94, 187–198 (2018).
Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 120, c179–184 (2012).
Park, W. Y. et al. Impact of acute kidney injury in expanded criteria deceased donors on post-transplant clinical outcomes: multicenter cohort study. BMC Nephrol. 20, 1–11 (2019).
Metzger, R. A. et al. Expanded criteria donors for kidney transplantation. Am. J. Transpl. 3, 114–125 (2003).
Port, F. K. et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation 74, 1281–1286 (2002).
Grams, M. E. et al. A meta-analysis of the association of estimated GFR, albuminuria, age, race, and sex with acute kidney injury. Am. J. Kidney Dis. 66, 591–601 (2015).
Singh, R. et al. The impact of trimethoprim-sulfamethoxazole as Pneumocystis Jiroveci pneumonia prophylaxis on the occurrence of asymptomatic bacteriuria and urinary tract infections among renal allograft recipients: a retrospective before-after study. BMC Infect. Dis. 16, 90 (2016).
Siew, E. D. et al. Estimating baseline kidney function in hospitalized patients with impaired kidney function. Clin. J. Am. Soc. Nephrol. 7, 712 (2012).
Bonomini, V., Stefoni, S. & Vangelista, A. Long-term patient and renal prognosis in acute renal failure. Nephron 36, 169–172 (1984).
Acknowledgements
We thank the Korean Network for Organ Sharing (KONOS) and the National Health Insurance Data Sharing Service (NHISS) for sharing their database.
Funding
This study was supported by a grant from the National Institute of Organ, Tissue and Blood. Management (20232400C1B-00), which was not involved in the design or analysis of the study.
Author information
Authors and Affiliations
Contributions
Research idea and study design: O.N., J.Y.; data acquisition: O.N., G.L., T.Y.K.; data analysis/interpretation: O.N., G.L., T.Y.K., B.K., J.Y.; statistical analysis: O.N., G.L., T.Y.K., J.H.L., H.B.K.; wrote the manuscript: O.N., J.Y. All authors read and approved of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All co-authors agreed to publication of the acquired data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Na, O., Lee, G., Koo, T.Y. et al. Impact of donor’s acute kidney injury on graft outcomes of deceased donor kidney transplantation. Sci Rep (2026). https://doi.org/10.1038/s41598-026-37147-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-37147-0