Abstract
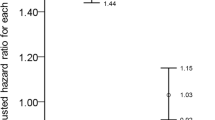
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease increasingly viewed as systemic. Irritable bowel syndrome (IBS) has been proposed as a comorbidity, yet longitudinal data remain limited. A retrospective cohort study was conducted using the U.S. Collaborative Network of the TriNetX platform, including adults diagnosed with HS from 2005–2023 and matched controls without HS. Patients with prior IBS or cancer were excluded. Propensity score matching (1:1) accounted for demographic, socioeconomic, and clinical variables. Incident IBS, defined by ICD-10-CM codes, was assessed over 15 years. Hazard ratios (HRs) with 95% confidence intervals (CIs) were estimated. Sensitivity analyses varied washout periods, follow-up times, and HS definitions; subgroups were stratified by age and sex. The matched cohort comprised 119,848 HS patients and equal controls. HS was associated with greater IBS risk (HR 1.422, 95% CI 1.308–1.547), consistent across sensitivity analyses. Compared with psoriasis, HS conferred higher IBS risk (HR 1.268, 95% CI 1.157–1.390). Age-stratified analyses showed increased risk in both 18–64 years (HR 1.538, 95% CI 1.397–1.694) and ≥ 65 years (HR 2.443, 95% CI 1.619–3.686). Risk was also elevated in males (HR 1.556, 95% CI 1.221–1.983) and females (HR 1.489, 95% CI 1.354–1.638). HS independently predicts higher long-term IBS risk, supporting shared inflammatory and barrier dysfunction pathways.
Similar content being viewed by others
Data availability
Data in this study were retrieved from TriNetX Research Network. All data available in the database were administrated by the TriNetX platform. Detailed information can be retrieved at the official website of the research network (https://trinetx.com).
References
Sabat, R. et al. Hidradenitis suppurativa. Nat. Rev. Dis. Primers. 6, 18. https://doi.org/10.1038/s41572-020-0149-1 (2020).
Jfri, A., Netchiporouk, E., Raymond, K., Litvinov, I. V. & O’Brien, E. Association of clinical severity scores with psychosocial impact in patients with hidradenitis suppurativa. J. Am. Acad. Dermatol. 84, 1712–1715. https://doi.org/10.1016/j.jaad.2020.08.022 (2021).
Kimball, A. B. et al. Burden of hidradenitis suppurativa: A systematic literature review of patient reported outcomes. Dermatol. Ther. (Heidelb) 14, 83–98. https://doi.org/10.1007/s13555-023-01085-w (2024).
Kashyap, M. P. et al. CD2 expressing innate lymphoid and T cells are critical effectors of immunopathogenesis in hidradenitis suppurativa. Proc. Natl. Acad. Sci. U S A 121, e2409274121. https://doi.org/10.1073/pnas.2409274121 (2024).
Oliveira, C. B. et al. Neutrophil extracellular traps activate Notch-γ-secretase signaling in hidradenitis suppurativa. J. Allergy Clin. Immunol. 155, 188–198. https://doi.org/10.1016/j.jaci.2024.09.001 (2025).
Rastrick, J. et al. The roles of interleukin (IL)-17A and IL-17F in hidradenitis suppurativa pathogenesis: Evidence from human in vitro preclinical experiments and clinical samples. Br. J. Dermatol. 192, 660–671. https://doi.org/10.1093/bjd/ljae442 (2025).
Garg, A. et al. Comorbidity screening in hidradenitis suppurativa: Evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J. Am. Acad. Dermatol. 86, 1092–1101. https://doi.org/10.1016/j.jaad.2021.01.059 (2022).
Gau, S. Y., Chan, W. L. & Tsai, J. D. Risk of atopic diseases in patients with hidradenitis suppurativa: A systematic review and meta-analysis of observational studies. Dermatology 239, 314–322. https://doi.org/10.1159/000528920 (2023).
Gau, S. Y., Hsiao, Y. P., Liao, W. C., Ma, K. S. & Wu, M. C. Risk of liver dysfunction and non-alcoholic fatty liver diseases in people with hidradenitis suppurativa: A systematic review and meta-analysis of real-world evidences. Front. Immunol. 13, 959691. https://doi.org/10.3389/fimmu.2022.959691 (2022).
Li, C. P., Lo, S. W., Tsai, R. Y., Chang, H. C. & Gau, S. Y. New-onset hidradenitis suppurativa in psoriasis patients: A Multi-Center Retrospective Cohort Study. Life https://doi.org/10.3390/life14060730 (2024).
Sperber, A. D. et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of rome foundation global study. Gastroenterology 160, 99-114.e113. https://doi.org/10.1053/j.gastro.2020.04.014 (2021).
Saha, L. Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World J. Gastroenterol. 20, 6759–6773. https://doi.org/10.3748/wjg.v20.i22.6759 (2014).
Chey, W. D., Kurlander, J. & Eswaran, S. Irritable bowel syndrome: A clinical review. JAMA 313, 949–958. https://doi.org/10.1001/jama.2015.0954 (2015).
Chen, S. J., Chang, H. C. & Gau, S. Y. Psoriasis patients are associated with increased risk of new-onset irritable bowel syndrome: A multicenter, retrospective cohort study. Int. J. Med. Sci. 22, 3422–3428. https://doi.org/10.7150/ijms.116551 (2025).
Marginean, C. M. et al. Gut-brain axis, microbiota and probiotics—Current knowledge on their role in irritable bowel syndrome: A review. Gastrointest. Disord. 5, 517–535 (2023).
Demirbaş, A. et al. The relationship between hidradenitis suppurativa and irritable bowel syndrome: A cross-sectional study. Turk. J. Med. Sci. 52, 97–104. https://doi.org/10.3906/sag-2107-158 (2022).
Gau, S. Y. et al. Human papillomavirus infection is associated with increased risk of new-onset hidradenitis suppurativa: A population-based cohort study. J. Am. Acad. Dermatol. https://doi.org/10.1016/j.jaad.2024.10.055 (2024).
Gau, S. Y. et al. Human papillomavirus infection increases risk of new-onset prurigo nodularis: A multicenter retrospective cohort study using global and US electronic medical records of TriNetX network. J. Am. Acad. Dermatol. https://doi.org/10.1016/j.jaad.2025.05.1442 (2025).
Egeberg, A. et al. Prevalence and risk of inflammatory bowel disease in patients with hidradenitis suppurativa. J. Invest. Dermatol. 137, 1060–1064. https://doi.org/10.1016/j.jid.2016.11.040 (2017).
Almenara-Blasco, M. et al. Multimorbidity of hidradenitis suppurativa: A cross-sectional population-based study of its associated comorbidities. Front. Med. 12, 1618975. https://doi.org/10.3389/fmed.2025.1618975 (2025).
Cascio Ingurgio, R. et al. An updated safety review of hidradenitis suppurativa treatment options. Expert Opinion Drug Saf. 24, 1121–1129. https://doi.org/10.1080/14740338.2025.2484022 (2025).
Naik, H. B., Jo, J. H., Paul, M. & Kong, H. H. Skin microbiota perturbations are distinct and disease severity-dependent in hidradenitis suppurativa. J. Invest. Dermatol. 140, 922-925.e923. https://doi.org/10.1016/j.jid.2019.08.445 (2020).
McCarthy, S. et al. Altered skin and gut microbiome in hidradenitis suppurativa. J. Investig. Dermatol. 142, 459-468.e415. https://doi.org/10.1016/j.jid.2021.05.036 (2022).
Sarnoff, R. P. et al. A multi-omic brain gut microbiome signature differs between IBS subjects with different bowel habits. Neuropharmacology 225, 109381. https://doi.org/10.1016/j.neuropharm.2022.109381 (2023).
Chen, B., Kim, J. J., Zhang, Y., Du, L. & Dai, N. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: A systematic review and meta-analysis. J. Gastroenterol. 53, 807–818. https://doi.org/10.1007/s00535-018-1476-9 (2018).
Mahmud, M. R. et al. Impact of gut microbiome on skin health: Gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut. Microbes 14, 2096995. https://doi.org/10.1080/19490976.2022.2096995 (2022).
Yuan, Y., Wang, X., Huang, S., Wang, H. & Shen, G. Low-level inflammation, immunity, and brain-gut axis in IBS: Unraveling the complex relationships. Gut. Microbes 15, 2263209. https://doi.org/10.1080/19490976.2023.2263209 (2023).
Dmitriev, A. et al. mTORC1—A potential player in the pathogenesis of hidradenitis suppurativa?. J. Eur. Acad. Dermatol. Venereol. 35, e444–e447. https://doi.org/10.1111/jdv.17202 (2021).
Vellaichamy, G. et al. Insights from γ-Secretase: Functional genetics of hidradenitis suppurativa. J. Investig. Dermatol. 141, 1888–1896. https://doi.org/10.1016/j.jid.2021.01.023 (2021).
Ratanasirintrawoot, S. & Israsena, N. Stem cells in the intestine: Possible roles in pathogenesis of irritable bowel syndrome. J. Neurogastroenterol. Motil. 22, 367–382. https://doi.org/10.5056/jnm16023 (2016).
Vural, S. et al. Evaluating dietary considerations in hidradenitis suppurativa: A critical examination of existing knowledge. Int. J. Dermatol. 63, 987–998. https://doi.org/10.1111/ijd.17101 (2024).
Bertin, L. et al. The Role of the FODMAP Diet in IBS. Nutrients 16 (2024).
Patel, K. R. et al. Association between hidradenitis suppurativa, depression, anxiety, and suicidality: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 83, 737–744. https://doi.org/10.1016/j.jaad.2019.11.068 (2020).
Kimball, A. B., Sundaram, M., Banderas, B., Foley, C. & Shields, A. L. Development and initial psychometric evaluation of patient-reported outcome questionnaires to evaluate the symptoms and impact of hidradenitis suppurativa. J. Dermatolog. Treat 29, 152–164. https://doi.org/10.1080/09546634.2017.1341614 (2018).
Koloski, N. A., Talley, N. J. & Boyce, P. M. A history of abuse in community subjects with irritable bowel syndrome and functional dyspepsia: The role of other psychosocial variables. Digestion 72, 86–96. https://doi.org/10.1159/000087722 (2005).
Black, C. J. & Ford, A. C. Global burden of irritable bowel syndrome: Trends, predictions and risk factors. Nat. Rev. Gastroenterol. Hepatol. 17, 473–486. https://doi.org/10.1038/s41575-020-0286-8 (2020).
Goldburg, S. R., Strober, B. E. & Payette, M. J. Hidradenitis suppurativa: Epidemiology, clinical presentation, and pathogenesis. J. Am. Acad. Dermatol. 82, 1045–1058. https://doi.org/10.1016/j.jaad.2019.08.090 (2020).
Nguyen, T. V., Damiani, G., Orenstein, L. A. V., Hamzavi, I. & Jemec, G. B. Hidradenitis suppurativa: An update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. J. Eur. Acad. Dermatol. Venereol. JEADV 35, 50–61. https://doi.org/10.1111/jdv.16677 (2021).
Sultan, S. & Malhotra, A. Irritable bowel syndrome. Ann. Intern. Med. 166, Itc81-itc96. https://doi.org/10.7326/aitc201706060 (2017).
Funding
This study was partially funded by Chung Shan Medical University Hospital (CSH-2025-C-007) and the Research Foundation of Taichung Veterans General Hospital.
Author information
Authors and Affiliations
Contributions
All the authors involved in drafting or revising the article and approved of the submitted version. Study conception and design: Chang HC, Hsu YH, Wu MC, Chen SJ Gau SY Data acquisition: Chang HC, Gau SY Data analysis and demonstration: Chang HC, Gau SY Original draft preparation: Chang HC, Hsu YH, Wu MC, Chen SJ, Gau SY.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Institutional Review Board of Chung Shan Medical University Hospital (CS1-25002) and Ditmanson Medical Foundation Chia-Yi Christian Hospital (IRB No. IRB2025121).
Informed consent
Due to the deidentification process of TriNetX research network, the need of informed consent was waived by the Institutional Review Board of Chung Shan Medical University Hospital (CS1-25002).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chang, HC., Hsu, YH., Chen, SJ. et al. Risk of irritable bowel syndrome in patients with hidradenitis suppurativa: a global-federated, multicenter cohort study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38442-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38442-6